Abstract
Study design
A retrospective clinical study.
Objective
To elucidate the usefulness of the patellar tendon reflex (PTR), bulbocavernosus reflex (BCR), and plantar response (PR) as factors in the prognostic prediction of motor function in complete paralysis due to cervical spinal cord injuries (CSCIs) at the acute phase.
Setting
Department of Orthopedic Surgery, Spinal Injuries Center, Japan.
Methods
99 patients assessed as the American Spinal Injury Association Impairment Scale (AIS) grade A (AIS A) were included in this study. The PTR, BCR, and PR were evaluated respectively as positive or negative at the time of injury. We classified the patients into two groups based on their neurological recovery at 3 months after injury: “recovered” group was defined as AIS C, D, or E; “non-recovered” group was defined as AIS A or B.
Results
Eight patients demonstrated positive PTR, while 91 demonstrated negative. Three out of eight patients with positive PTR (37.5%) were R group, while 83 out of 91 patients with negative PTR (91.2%) were N group. A significant difference was observed (p = 0.043). For BCR, no significant difference was observed (p > 0.05). Twenty-six patients demonstrated positive PTR, while 73 demonstrated negative. Nine out of twenty-six patients with positive PR (34.6%) were R group, while 71 out of 73 patients with negative PR (97.3%) were N group. A significant difference was observed (p = 0.000068).
Conclusion
The PTR and PR are useful for poor prognostic prediction of motor function in CSCI at the acute phase.
Similar content being viewed by others
Introduction
Cervical spinal cord injuries (CSCIs) are the most severe cases of spinal cord injuries which often result in complete or partial loss of sensorimotor functions or even fatalities. Since the severity of CSCI differs considerably from patient to patient and substantial spontaneous functional recovery is often observed during the acute phase, the prognostic prediction of motor function is extremely difficult for CSCI at the acute phase. In fact, even in mild CSCI, severe paralysis was temporarily observed during the acute phase, followed by a drastic functional recovery. Therefore, accurate evaluation for the efficacy of acute therapeutic interventions is particularly difficult. Regarding cases of complete sensorimotor paralysis caused by CSCIs, Frankel et al. [1] and Ueta et al. [2] reported that 17.1% and 23.8% of patients, respectively, recovered to incomplete motor paralysis.
Kawano et al. [3] reported that confirmation of permanent complete paralysis due to CSCI requires eight weeks; however, if we have accurate diagnostic methods for the prognostic prediction of CSCI at the acute phase, we can prepare for patient’s early therapeutic intervention and social rehabilitation.
Evaluation of paralytic severity during the very acute phase of CSCI is particularly difficult because of patient-specific factors such as deterioration of consciousness, presence of respiratory failure, multiple traumas, and psychiatric disorders. However, reflexes are an involuntary, unlearned, and repeatable response to a specific stimulus that does not require any input from the brain [4], i.e., reflexes are not affected by any patient-specific factors and are real basal neural responses. Thus, we focused on early responses of the patellar tendon reflex (PTR), bulbocavernosus reflex (BCR), and plantar response (PR) as the prognostic prediction factors for complete CSCI at the acute phase.
Patients and methods
Study design: a retrospective clinical study
Study population
From 2012 to 2021, a total of 555 patients with a traumatic CSCI were treated at the Spinal Injuries Center. Of these, 99 patients were hospitalized within 72 h of injury and neurologically evaluated as the American Spinal Injury Association Impairment Scale (AIS) grade A (AIS A) (average age: 59.6 years, range: 17–86 years) [5]. CSCI with major bone injury were surgically treated immediately after hospitalization. With respect to CSCI without major bone injury, the cases with severe cervical cord compression were treated surgically, and the others with mild compression were treated conservatively.
Neurological status was evaluated using the AIS at the time of injury and 3 months after the injury. Additionally, the PTR, BCR, and PR were evaluated respectively as positive or negative at the time of injury. The plantar response included: (1) normal flexor plantar response; (2) pathologic or abnormal extensor plantar response (Babinski sign) [6], and the delayed plantar response was excluded.
We classified the subjects into two groups based on their neurological recovery at 3 months after injury: ‘recovered’ (R) group was defined as AIS C, D, or E; “non-recovered” (N) group was defined as AIS A or B.
This study was approved by the Ethical Review Board of Japan Labor Health and Welfare Organization Spinal Injuries Center. We had all the necessary consent from the patients involved in the study, including consent to participate in the study where appropriate.
Statistical analysis
Fisher’s exact test was used to calculate the differences between the recovered group and the non-recovered group. Statistical significance was set at p < 0.05. Moreover, the sensitivity, specificity, positive likelihood ratios and negative likelihood ratios were calculated.
Results
Eleven Patients were classified into R group (AIS C 8 patients, AIS D 3 patients) and 88 patients were classified into N group (AIS A 80 patients, AIS B 8 patients). 11.1% (11 out of 99) of patients with complete CSCI recovered their motor function.
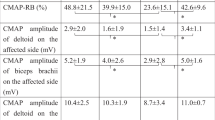
Table 1 shows the relationship between the PTR and motor recovery status. Eight patients demonstrated positive PTR, while 91 demonstrated negative. Three out of eight patients with positive PTR (37.5%) were R group, while 83 out of 91 patients with negative PTR (91.2%) were N group. A significant difference was observed (p = 0.043). The sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were 27.2%, 94.3%, 4.77 and 0.772, respectively.
Table 2 shows the relationship between the BCR and motor recovery status. Fifty patients demonstrated positive BCR, while 49 demonstrated negative. Four out of fifty patients with positive BCR (8.0%) were R group, while 42 out of 49 patients with negative BCR (85.7%) were N group. No significant difference was observed (p > 0.05). The sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were 36.4%, 47.7%, 0.696 and 1.33, respectively.
Table 3 shows the relationship between the PR and motor recovery status. Twenty-six patients demonstrated positive PTR, while 73 demonstrated negative. Nine out of twenty-six patients with positive PR (34.6%) were R group, while 71 out of 73 patients with negative PR (97.3%) were N group. A significant difference was observed (p = 0.000068). The sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were 81.8%, 80.7%, 4.24 and 0.226, respectively.
Additionally, combination of the PTR and PR were analyzed. Table 4 shows the relationship between the PTR with PR and motor recovery status. Twenty-eight patients demonstrated positive PTR and positive PR, while 71 demonstrated negative PTR and negative PR. Ten out of twenty-eight patients with positive PTR and/or positive PR (35.7%) were R group, while 70 out of 71 patients with negative PTR and negative PR (98.6%) were N group. A significant difference was observed (p = 0.0000076). The sensitivity, specificity, positive likelihood ratio and negative likelihood ratio were 90.9%, 79.5%, 4.43 and 0.114, respectively.
Discussion
Various methods have been described to predict the prognosis of motor paralysis in patients with complete CSCI at the acute phase, including the use of magnetic resonance (MR) images [7,8,9], somatosensory evoked potentials (SSEP) [10,11,12,13], or determination of amplitude in electromyography [14, 15]. However, these examinations for prognostic values are still controversial. Recently, blood glucose or serum zinc concentrations were proved to be the indicators for functional prognosis of spinal cord injuries [16, 17]. However, specialized maneuvers are complicated.
The pathway through which nerve signals pass during physiological reflexes is called the reflex arc. The components of the spinal reflex arc are (1) sensory receptors (skin, muscle, tendon, etc.), (2) afferent nerves (sensory input), (3) spinal interneuron, (4) efferent nerves (output), and (5) effector (muscle). In CSCI, the pathway of the reflex arc should not be impaired, and the reflex should occur normally. However, all reflexes vanish completely during the spinal shock due to CSCI. Usually, superficial reflexes might recover after several days, and deep tendon reflexes recover after 1-2 weeks [18]. The pathophysiology of spinal shock is an ongoing physiologic continuum, and there are 4 stages in spinal shock. However, spinal shock cannot be classified strictly. We evaluated at the acute phase (within 72 h), i.e. phase 1 and 2 advocated by Ditunno et al. [19].
In the study by Morishita et al. [20], patients with complete CSCI that demonstrated positive PTR at within 72 h of injury had 94.1% of motor functional recovery rate. In our study, only 37.5% of complete CSCI with positive PTR demonstrated motor functional recovery. We hypothesized that the age at injury might greatly contribute to this discrepancy. Average age for the study by Morishita et al. [20] was 44.2 year-old and ours was 59.6 year-old. In our study, negative or weak PTR ratio before injury might be higher than the report of Morishita et al. [20]. It is well known that recovery of paralysis in elderly CSCI patients is worse than in younger patients [21, 22]. Despite the occurrence of change to positive PTR or the maintenance of positive PTR after injury, the motor function might not recover in elderly patients. On the other hand, both studies showed same negative rate (Morishita et al. [20] 91.2%; 114 out of 125 patients, ours 91.2%; 83 out of 91 patients: negative PTR and non-recovered). Therefore, positive PTR might not be a useful prognostic factor, but negative PTR might be a reliable negative prognostic factor.
We additionally evaluated the BCR and PR. There was no significant relationship in the BCR value. The BCR is a well-known somatic reflex that is useful for gaining information about the state of the sacral spinal cord segments [23] and the appearance of BCR was classically interpreted as the end of the spinal shock within CSCI [24, 25]. However, based on the report of Ditunno et al [19], the appearance of BCR is not the end of the spinal shock. Instead of the appearance of BCR in early phase of the spinal shock, our study shows the BCR might not be a useful prognostic factor for motor functional recovery in CSCI. While, regarding to the PR, similar reliability was seen with the PTR. To the best of our knowledge, no reports have thus far referred to the detailed relationship between the PR and motor functional recovery in CSCI. Therefore, combination with the PTR and PR might be more useful predictor. 98.6% (70 out of 71 patients) with negative PTR and negative PR showed none of motor functional recovery during 3 months after injury. Moreover, combination of the PTR and PR showed the reduction of the false R group patients with negative PTR and negative PR, and improved the sensitivity (90.9%). Complete CSCI with negative PTR and negative PR at the acute phase cannot be expected of motor functional recovery.
Limitations
Certain issues remain unaddressed in the current study. We did not discuss the effects of patients aging to reflex response in the study. Moreover, we only indicated the negative prognostic prediction for CSCI. Therefore, using the current investigation as a pilot study, further research with different age bracket using a larger patient population and may help in resolving several remaining unclear issues. Moreover, prognostic prediction for motor functional recovery in acute CSCI needs to be clarified in greater detail.
Conclusion
The PTR and PR are useful for poor prognostic prediction for motor functional recovery in complete CSCI at the acute phase. Complete CSCI with negative PTR and negative PR at the acute phase cannot be expected of motor functional recovery.
Data availability
The data that support the findings of this study are available from the corresponding author, Hironari Kaneyama, upon reasonable request.
References
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–92.
Ueta T, Shiba K. Cervical cord injuries; comprehensive treatment in the acute stage and neurological prognosis. J Jsrs. 2001;12:389–417. (in Japanese)
Kawano O, Maeda T, Mori E, Takao T, Sakai H, Masuda M, et al. How much time is necessary to confirm the diagnosis of permanent complete cervical spinal cord injury? Spinal Cord. 2020;58:284–9.
Boes CJ. The history of examination of reflexes. J Neurol. 2014;261:2264–74.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2021;34:535–46.
Geeta AK. Plantar reflex. JIACM. 2005;6:193–7.
Boldin C, Raith J, Fankhauser F, Haunschmid C, Schwantzer G, Schweighofer F, et al. Predicting neurologic recovery in cervical spinal cord injury with postoperative MR imaging. Spine 2006;31:554–9.
Flanders AE, Spettell CM, Tartaglino LM, Friedman DP, Herbison GJ. Forecasting motor recovery after cervical spinal cord injury: value of MR imaging. Radiology. 1996;201:649–55.
Miyanji F, Furlan JC, Aarabi B, Arnold PM, Fehlings MG. Acute cervical traumatic spinal cord injury: MR imaging findings correlated with neurologic outcome-prospective study with 100 consecutive patients. Radiology. 2007;243:820–7.
Curt A, Dietz V. Ambulatory capacity in spinal cord injury: significance of somatosensory evoked potentials and ASIA protocol in predicting outcome. Arch Phys Med Rehabil. 1997;78:39–43.
Curt A, Dietz V. Electrophysiological recordings in patients with spinal cord injury: significance for predicting outcome. Spinal Cord. 1999;37:157–65.
Jacobs SR, Yeaney NK, Herbison GJ, Ditunno JF Jr. Future ambulation prognosis as predicted by somatosensory evoked potentials in motor complete and incomplete quadriplegia. Arch Phys Med Rehabil. 1995;76:635–41.
Xie J, Boakye M. Electrophysiological outcomes after spinal cord injury. Neurosurg Focus. 2008;25:E11.
Calancie B, Molano MR, Broton JG. Abductor hallucis for monitoring lower-limb recovery after spinal cord injury in man. Spinal Cord. 2004;42:573–80.
Calancie B, Molano MR, Broton JG. Tendon reflexes for predicting movement recovery after spinal cord injury in humans. Clin Neurophysiol. 2004;115:2350–63.
Kobayakawa K, Kumamaru H, Saiwai H, Kubota K, Ohkawa Y, Kishimoto J, et al. Acute hyperglycemia impairs functional improvement after spinal cord injury in mice and humans. Sci Transl Med. 2014;6:256ra137.
Kijima K, Kubota K, Hara M, Kobayakawa K, Yokota K, Saito T, et al. The acute phase serum zinc concentration is a reliable biomarker for predicting the functional outcome after spinal cord injury. EBioMedicine 2019;41:659–69.
Ko HY, Ditunno JF Jr, Graziani V, Little JW. The pattern of recovery during spinal shock. Spinal Cord. 1999;37:402–9.
Ditunno JF, Little JW, Tessler A, Burns AS. Spinal shock revisited: a four-phase model. Spinal Cord. 2004;42:383–95.
Morishita K, Kasai Y, Ueta T, Shiba K, Akeda K, Uchida A, et al. Patellar tendon reflex as a predictor of improving motor paralysis in complete paralysis due to cervical cord injury. Spinal Cord. 2009;47:640–2.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M. Effects on age on spinal cord lesion patients’ rehabilitation. Spinal Cord. 2003;41:457–64.
Johansson E, Luoto TM, Vainionpää A, Kauppila AM, Kallinen M, Väärälä E, et al. Epidemiology of traumatic spinal cord injury in Finland. Spinal Cord. 2021;59:761–8.
Previnaire JG. The importance of the bulbocavernosus reflex. Spinal Cord Ser Cases. 2018;4:2.
Holdsworth FW. Neurological diagnosis and the indications for treatment of paraplegia and tetraplegia, associated with fractures of the spine. Manit Med Rev. 1968;48:16–18.
Stauffer ES. Diagnosis and prognosis of acute cervical spinal cord injury. Clin Orthop Relat Res. 1975;112:9–15.
Acknowledgements
We gratefully acknowledge the work of past and present members of our institution, Spinal Injuries Center in Japan.
Author information
Authors and Affiliations
Contributions
HK was involved in the design of the study, supervised data collection, conducted data analysis and interpreted the findings, was responsible for drafting, revising, and finalizing the manuscript for submission. OK developed the study protocol and contributed to revising the manuscript. YM, TY, and TM provided feedback and approved the manuscript draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaneyama, H., Kawano, O., Morishita, Y. et al. Predicting motor function recovery in cervical spinal cord injury-induced complete paralysis with reflex response. Spinal Cord 60, 1020–1022 (2022). https://doi.org/10.1038/s41393-022-00821-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00821-x