Abstract
Study design
Cohort comparative study.
Objective
Evaluate the suitability of satisfaction scores for the assessment of quality of care and service in spinal rehabilitation.
Setting
Spinal rehabilitation department.
Methods
Fifty-two inpatients participated anonymously in a large satisfaction survey, in 2017. A questionnaire containing the same questions was completed by 96 other inpatients, whose personal details were known, admitted to the same department between 2017 and 2019. Differences in satisfaction scores were compared between the two groups, between years, and between identified patients with differences in perceived progress and satisfaction with progress, using Mann–Whitney tests. In the identified patients, the association between satisfaction and patient demographic, neurological, and functional characteristics was evaluated using Pearson correlations. Analysis of variance and t test assessed the effect of comorbidities on satisfaction. T test assessed gender differences between groups. The effect of associated factors on satisfaction was examined using a stepwise linear regression.
Results
The total satisfaction score was 86.05 ± 16.99 for the anonymous group and 88.75 ± 12.45 for the identified patients (p > 0.05). The only patient characteristics that were associated with satisfaction were years of education, the perception of progress during rehabilitation, and the satisfaction with progress (p < 0.02). Their contribution to the total satisfaction variance, however, was relatively small (R2 = 0.211).
Conclusions
The small effect of patient characteristics on total satisfaction indicates that satisfaction scores can be used to assess the quality of care and service in spinal rehabilitation. This and the similarity in findings between the groups supports the validity of the questionnaires.
Similar content being viewed by others
Introduction
Many service providers consider client satisfaction to be an indication of quality of service [1, 2]. Following this understanding, much effort has been devoted in recent years to assessing the quality of medical care and services from the patients’ perspective [3,4,5,6,7]. In healthcare services, however, patient satisfaction may be influenced also by factors related to the patients themselves, rather than exclusively by the service and medical care provided [3, 8, 9]. Chow et al. assigned the term “satisfaction determinants” to patient-related variables that affect patient satisfaction, including patients’ expectations and characteristics, such as their perspective of their health condition, age, education, ethnic group, and economic or social class [10]. The authors assigned the term “satisfaction components” to measures of care or service that patients receive in practice [10, 11]. Health status was frequently found to be a strong predictor of patient satisfaction: healthier patients were more satisfied [3, 12]. Mental state also affected satisfaction: patients with psychiatric diagnosis were less satisfied with their treatment than were those without such diagnosis [13, 14]. Findings regarding the association between patient satisfaction and demographic determinants, such as age, gender, and education were conflicting [3, 7, 9].
For inpatient rehabilitation, the relationship between quality of service and care may be considered more complex than in other health domains. The relatively long stay in hospital of rehabilitation inpatients, and their exposure to many staff members from different disciplines, may cause difficulty in integrating the qualities of the various components of service or care, and satisfaction may hinge on incidental events. Disparities between the goals of the patient, who is seeking a cure, and those of caregivers, who strive to improve performance, may be a source of dissatisfaction, regardless of the quality of care. At the same time, patients may be aware of differences in goals, and report a high degree of satisfaction, although actual progress did not match their expectations [15]. Rehabilitation outcomes, which may be affected by patient cooperation, can also affect patient satisfaction, further hampering the ability to attribute patient satisfaction to the quality of care.
Therefore, constructing a satisfaction questionnaire in rehabilitation should take into account the unique aspects of the rehabilitation process, although most of the questionnaires in use in rehabilitation do not address these aspects [16,17,18,19,20]. Patient satisfaction surveys, however, are used widely in rehabilitation, as in other health services, to quantitatively assess patient satisfaction and allow comparison between different services, departments, and institutions [16,17,18,19,20]. Among these surveys are those conducted by the Israel Ministry of Health and the health organization “Clalit”. Clalit, which provides health services to over 4.7 million persons in Israel, designed a satisfaction questionnaire for geriatric and rehabilitation departments (S1 Appendix 1). In 2017, Clalit used this questionnaire in a survey of rehabilitation inpatients, including those of a Spinal Rehabilitation Department (SRD), and their relatives. The questionnaire, however, was not validated in a rehabilitation ward, and it was not clear to what extent the findings of the study reflect satisfaction determinants or components.
The present study was conducted to examine the utility of a satisfaction survey for the assessment of quality of care and service in spinal rehabilitation. To this end, it examined whether findings of the Clalit survey of satisfaction with care and service can be used to assess the quality of care and service in a spinal rehabilitation ward. A direct comparison of the findings of the satisfaction survey with measures of care or service that patients receive in practice in spinal rehabilitation was not practical because we did not find valid measures that integrate the dozens of indicators required for direct assessment of the quality of care and service actually received in spinal rehabilitation. These indicators include the structure of the healthcare system and the characteristics of the medical process, which are related to individuals with SCI. They also include patient satisfaction and characteristics examined in this study [21].
At the same time, researchers have used patient satisfaction related to characteristics of care and service as a proxy for the quality of care and service, if patient characteristics do not bias it.
To evaluate the reliability of the satisfaction questionnaire and the risk of such a bias, we compared, the responses of two patient groups to the questionnaire, and tested the associations between the responses and patient characteristics.
Methods
Participants
For comparison with 52 unidentified patients of the SRD who had been examined in the Clalit satisfaction survey in 2017 (Clalit Group), and for the examination of the association between the satisfaction and characteristics of identified patients, we enrolled inpatients who were admitted to the SRD between the years 2017 and 2019 (SRD group). The patients were selected according to inclusion and exclusion criteria, and based on their availability to be interviewed, on the day of their discharge from rehabilitation. Availability depended on the timing of the interview, which had to be coordinated with external interviewers; to avoid bias, these interviewers were not part of the department staff, and were not familiar with the patients. Inclusion criteria were: admission for rehabilitation with a spinal cord injury (SCI), spinal roots injury, Guillain-Barré syndrome, or other debilitating polyneuropathy; stay in rehabilitation of at least 28 days; age of 18 years or older at admission; and proficiency in understanding Hebrew. Exclusion criteria were documented psychiatric, behavioral, or cognitive conditions, which could influence the reliability of the answers.
The questionnaire and scoring of satisfaction
The questionnaire used in the interview for the identified SRD patients (the combined Clalit-SRD questionnaire) consisted of 41 questions. Thirty nine “Clalit questions” (from the original Clalit survey), focused on the quality of care and service, or the satisfaction with them, and two “specific questions” about the participants’ assessment of their progress, and their satisfaction with that progress, which were added to the questionnaire for the identified SRD patients (S1 Appendix 1). The Clalit questions are divided into 6 categories, each of which was assigned a weight, as a percent of the total score: 15% for the category of strategic questions, 25% for attitude of staff, 25% for information quality, 10% for availability of staff, 10% for coordination of staff, and 15% for conditions at the facility.
The Clalit questions offered a choice between 2, 5, and 10 answers. The answers for each question were scored as follows: for most of the questions, which offered five choices, the score for the answer was 1 (indicating that the participant was satisfied) if the participants selected one of the first two choices (top 2), and 0 (indicating that the participant was not satisfied) if the participant selected choices 3 or 4. If the participant selected the 5th choice, indicating that the question was irrelevant, the answer was not assigned a score. Answers for the two-choice questions were scored 1 if the participant selected the first choice and 0 if the participant selected the second choice. Answers to the 10-choice questions were scored 1 if the participant selected choices 8–10 and 0 if the selected score was lower.
For each of the six categories, the patients’ raw score was calculated by dividing the number of answers scored 1 (“satisfied”) by the total number of scored answers. Questions that were not scored because they were found irrelevant, or for any other reason, were not counted for this calculation.
We weighted each Clalit question category score. For each patient, we calculated the weighted category satisfaction score by multiplying the category raw score by its weight, as a percent of the total score. We calculated the total satisfaction score, reflecting the overall level of satisfaction for each participant, by summing up the weighted Clalit question category satisfaction scores. We then determined the group total satisfaction score by calculating the mean of the total satisfaction scores of all patients.
Procedure
External interviewers met the identified enrolled patients, on their discharge day and completed the combined Clalit-SRD satisfaction questionnaire. The data collected by the interviewers were entered into an Excel spreadsheet, together with demographic and clinical information retrieved from the patients’ hospital records. We retrieved the following variables: age, gender, years of education, date of lesion onset (defined as the date on which the lesion appeared or the first time it was mentioned in the patient’s medical records), comorbidities, length of stay in rehabilitation (LOS) in days, admission American Spinal Injury Association (ASIA) Impairment Scale (AIS) grade (A–E), admission and discharge ASIA Motor Score (AMS; range 0–100) and Sensory Score (ASS; range 0–112) [22], Spinal Cord Independence Measure third version (SCIM III; range 0–100) [23], and Spinal Cord Ability Realization Measurement Index (SCI-ARMI; range 0–100) [24]. SCIM III is a scale for the assessment of performance of daily function. SCI-ARMI is a scale for the assessment of disability weighted for the neurologic deficit. It allows evaluating quantitatively the independent role of rehabilitation in improving function, beyond that expected following spontaneous neurologic improvement.
Data analysis
We used mean and standard deviation, or standard error of the mean, for descriptive statistics.
To compare the total satisfaction scores among participants of the anonymous Clalit group with those of the identified SRD group, as well as between subgroups of identified patients, we used the Mann–Whitney nonparametric tests for independent samples.
To assess the relationship between the total satisfaction score of the SRD group and most of the variables retrieved from the patients’ hospital records, the time from lesion onset to discharge from rehabilitation, and the change from admission to discharge (delta) of SCIM, AMS, ASS, and SCI-ARMI, we used the Pearson correlation coefficient. To assess the effect of comorbidities, which may not affect daily functioning and may not be reflected in SCIM (Table 1), we used analysis of variance and t test. We assessed the gender difference in total satisfaction score using a t test.
To evaluate associations between the total satisfaction and the perception of progress during rehabilitation of patients in the SRD group, and their satisfaction with progress, we compared the total scores on the 39 Clalit questions, between identified SRD patients who selected different choices, on each of the two “specific questions” (S1 Appendix 1, questions 40–41). We used the Mann–Whitney nonparametric test for this comparison.
To confirm the effect on the total satisfaction of the patient characteristics that were found to be associated with it, and to assess their contribution to the total variance in satisfaction, we performed a stepwise linear regression.
P values lower than 0.05 were considered significant. Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS version 25.0, Chicago, IL, USA).
Results
Patient data
Ninety-nine identified inpatients were initially enrolled to the SRD group. We excluded two patients who stayed in rehabilitation less than 28 days, and a patient who changed her mind and refused to participate, leaving 96 patients who were included in the analysis and contributed to study findings. Of these, 32 were admitted to the SRD during 2017.
The sample of identified patients included 66 men (68.8%) and 30 women (31.3%). Patient characteristics and clinical findings of the sample are presented in Tables 1 and 2. Calculated delta AMS was 10 (±18.7), delta ASS 2 (±11.64), delta SCIM 25 (±16.69), and delta SCI-ARMI 26 (±18.4).
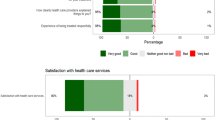
Satisfaction in the identified patients’ sample
The mean total satisfaction score on the 39 Clalit questions of the 96 identified patients was 88.79 (SD = 12.45). It was 86.21 (SD = 12.05; N = 32) in 2017, 91.83 (SD = 11.08; N = 39) in 2018, and 87.34 (SD = 14.34; N = 25) in 2019. The difference in total satisfaction score between the years 2017 and 2018, and between 2018 and 2019 was significant (p < 0.01, p < 0.03). The difference in total satisfaction between 2017 and 2019 was not significant (p = 0.69). Comparison of satisfaction in individual categories between years is presented in Fig. 1. The satisfaction scores for answers to individual questions ranged between 60.29 and 100. These and the category-weighted scores are shown in Table 3.
Comparison of the studies
The total satisfaction rate in the anonymous Clalit group, in 2017, was 86.05 (SD = 16.99, N = 52). Comparison of total satisfaction rate between this group and the participants of the identified SRD group, who were enrolled during 2017, and the 96 participants of the entire identified SRD group, did not show a significant difference (p > 0.05). The difference between these groups was not found to be significant in any of the six categories of the questionnaire (Fig. 2).
Association between satisfaction rate and patient characteristics
No statistically significant associations were found between the SRD group total satisfaction score on the 39 Clalit questions concerning care and service, and the following variables: age, gender, LOS, time from lesion onset to discharge from rehabilitation, and admission AIS grade. The associations with admission, discharge, and delta AMS, ASS, SCIM III, and SCI-ARMI scores were also non-significant (p > 0.05). The satisfaction scores did not differ significantly either between any of the four groups with or without comorbidities (detailed in Table 1), or between the three groups with comorbidities combined and the patients’ group with no comorbidity (p > 0.3). The negative correlations of total satisfaction scores with years of education were significant but weak (r = −0.264, p < 0.02).
Total satisfaction scores were higher for the SRD group patients who perceived their condition at discharge as “much better” than on admission (according to the scores of the last two questions in Appendix 1 (S1), than for those who perceived their discharge condition as “better” (91.3 vs. 87.55; p < 0.04). Total satisfaction scores were also higher for the SRD group patients who perceived the discharge condition as “better” than for those who perceived “no change” (87.55 vs. 77.7; p < 0.04). Total satisfaction scores tended to be higher for SRD group patients who were “very much satisfied” with their progress than for those who were “much satisfied” (92.7 vs. 88.8; p = 0.15), and were higher for those who were “much satisfied” than for those who were “moderately satisfied” (88.8 vs. 78.96; p < 0.01).
The effect of years of education, perception of progress during rehabilitation, and satisfaction with progress (patient characteristics that were found to be associated with the total satisfaction) on total satisfaction was found to be significant (p < 0.01). Their contribution to the total variance of satisfaction, however, was relatively small (R2 of their accumulated effect model = 0.211).
Discussion
This study shows that a satisfaction survey can be used to assess quality of care and service in spinal rehabilitation. This conclusion has been reached because the influence of patient characteristics on total satisfaction was minor in the present study, indicating that satisfaction scores that address quality of care and service, reflect mainly the quality of care and service in the examined rehabilitation department.
Patient characteristics and satisfaction
The satisfaction of SRD patients was not found to be significantly associated with most of the examined patient characteristics (demographic, those related to time from lesion onset, to comorbidities, to neurological or functional condition, to ability realization, or to change in their values during rehabilitation). The few patient characteristics that affected satisfaction (years of education, perception of progress, and satisfaction with progress) made a small contribution to variance in total satisfaction, indicating that the effect of patient characteristics on SRD satisfaction scores in spinal rehabilitation was negligible. This suggests that the main factors affecting patient satisfaction in the rehabilitation ward were the quality of care and quality of service that the questionnaire addresses, not patient factors.
Validity of the questionnaires
The similarity in findings between the two examined groups, in response to repeated use of the same questions, supports the reliability of the questionnaires. Total satisfaction rate in the 32 identified SRD patients admitted to rehabilitation in 2017 (86.21, SD = 12.05), and of the 96 identified patients admitted between 2017 and 2019 (88.79, SD = 12.45) was found similar to the total satisfaction rate in the group of 52 anonymous patients of the Clalit survey from 2017 (86.05, SD = 16.99). The similarity in satisfaction scores between the groups also indicates that satisfaction scoring was independent of identification, and that satisfaction rate in the SRD was stable. The stability persisted for three years and across all satisfaction categories (Figs. 1 and 2). The slight fluctuation in satisfaction between years, mainly with regard to the availability of the staff, indicated in Fig. 1, may be attributed to fluctuations in the size of nursing staff that occur from time to time, which may affect timely response to calls and requests, and sensitivity to patients’ pain.
The patients included in the identified sample most likely had medical conditions similar to those in the Clalit survey because they had typical admission diagnoses encountered in the inpatient SCI rehabilitation unit, and showed changes in neurological and functional conditions that characterize patients admitted to the SRD (Tables 1 and 2).
The combination of being reliable and able to reflect the quality of care and service, and not other traits, supports the validity of the questionnaires used in Clalit study and in the study of identified SRD patients.
Satisfaction of patients after SCI
The total rate of satisfaction with care and service in the SRD of both the anonymous and identified patients described here was 86–91%. The main satisfaction class studied after SCI is satisfaction with life, and most of the studies on life satisfaction after SCI examined patients in the community [25,26,27,28,29,30]. Jörgensen et al. recently examined satisfaction with life as a whole and in ten domains of life in Sweden. The authors found that 78% of SCI patients were at least “rather satisfied,” which is quite close to the satisfaction rate in our study.
In most studies, however, Satisfaction with life after SCI was associated with patient characteristics. In the Swedish study, life satisfaction was negatively associated with the severity of the neurological deficit and with secondary health conditions [25]. In a British study, life satisfaction was found to be related to appraisal of disability, participation, and secondary complications of the SCI [26]. In other studies, life satisfaction was associated with gender, re-hospitalization, time from injury, level of injury, disability, handicap, pain, education, social skills, and the economic condition of the person and the country [27,28,29,30]. Satisfaction with life may also influence the report on satisfaction with care and service [4]. But most of the studies examined its relationship with patient characteristics, in the chronic SCI phase in the community, and some of the studies showed conflicting relationships, or no correlation with time from injury [28, 29]. By contrast, the present study examined inpatients.
Only a few publications assessed the satisfaction of SCI patients with care or service. Two of these assessed it in the community, and showed that 70% of participants indicated satisfaction with healthcare services, which correlated with various patient characteristics [4, 5]. We found one study of satisfaction with care during acute SCI hospitalization. It showed that most patients were satisfied with the quality of the information received and the relationship with the healthcare practitioners, but reported dissatisfaction with the content of the information [6]. We found no previous study that assessed overall satisfaction with care and service, and its relationship with patient characteristics, at discharge from inpatient rehabilitation.
Study limitations
The indirect inferences of the present study from the Clalit survey and the possibility of additional reasons for the minimal influence of patient characteristics on satisfaction may limit the robustness of the findings of the present study. If the data of the patients who participated in the Clalit study had been analyzed, it could have demonstrated the effect of patient factors on the satisfaction score of that survey more precisely than did the data obtained from another patient group. We were not able, however, to use the data of the patients who participated in the Clalit survey because that study was anonymous, but the similarity we demonstrated between the study groups minimizes the likelihood of bias due to this limitation.
It is possible to attribute the minimal influence of patient characteristics on satisfaction to reasons other than those suggested here. These include the omission from our analysis of factors, such as the mental condition of the patient, the mode of payment, and a general tendency of patients to report relatively high satisfaction during rehabilitation [25, 26]. Note, however, that we excluded patients with mental conditions that may affect satisfaction, and we found no difference in satisfaction between those with mental conditions who complied with the inclusion-exclusion criteria, and the other patients. The mode of payment was similar for most participating patients, who are insured by one of the four HMOs in Israel. The distribution of scores in this study (range 60.29–100; SD = 12.45) reflects a substantial variability, and does not support the possibility that a general tendency influenced the reported satisfaction. These factors, therefore, are unlikely to have affected the findings.
Conclusions
This study showed that patient characteristics scarcely affect satisfaction in spinal rehabilitation, and that inpatient satisfaction reflects mainly the quality of care and service in this patient population. Satisfaction surveys, therefore, can be used to assess quality of care and service in spinal rehabilitation.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Johnston R. The zone of tolerance: exploring the relationship between service transactions and satisfaction with the overall service. Int J Serv Ind Manag. 1995;6:46–61.
Gogoi D, Jyoti B. Service quality measure: how it impacts customer satisfaction and loyalty. Int J Manag. 2020;11:354–65.
Kitano CPT, Kawakami M, Fukui D, Ishimoto Y, Nagata K, Yamada H, et al. Preoperative psychological factors affecting surgical satisfaction of elderly patients with lumbar spinal stenosis. J Orthop Sci. 2020;25:751–6.
Post MWM, van Asbeck FWA, van Dijk AJ, Schrijvers AJ. Services for spinal cord injured: availability and satisfaction. Spinal Cord. 1997;35:109–15.
Ronca E, Scheel-Sailer A, Koch HG, Essig S, Brach M, Münzel N, et al. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J Spinal Cord Med. 2020;43:111.
Lusilla-Palacios P, Castellano-Tejedor C. Acute spinal cord injury patients’ satisfaction with care: Results from an intervention study in a specialized rehabilitation unit. J Health Psychol. 2017;22:1289–99.
Johnson BC, Vasquez-Montes D, Steinmetz L, Buckland AJ, Bendo JA, Goldstein JA, et al. Association between nonmodifiable demographic factors and patient satisfaction scores in spine surgery clinics. Orthopedics. 2019;42:143–8.
Dijkers M. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Rehab. 1999;80:867–76.
Arraras JI, Illarramendi JJ, Viudez A. Determinants of patient satisfaction with care in a Spanish oncology day hospital and its relationship with quality of life. Psychooncology. 2013;22:2454–61.
Chow A, Mayer EK, Darzi AW, Athanasiou T. Patient-reported outcome measures: the importance of patient satisfaction in surgery. Surgery. 2009;146:435–43.
Ware JE, Snyder MK, Wright WR, Davies AR. Defining and measuring patient satisfaction with medical care. Eval Program Plann. 1983;6:247–63.
Covinsky KE, Rosenthal GE, Chren MM, Justice AC, Fortinsky RH, Palmer RM, et al. The relation between health status changes and patient satisfaction in older hospitalized medical patients. J Gen Intern Med. 1998;13:223–9.
Hoff RA, Rosenheck RA, Meterko M, Wilson NJ. Mental illness as a predictor of satisfaction with inpatient care at Veterans Affairs hospitals. Psychiatr Serv. 1999;50:680–5.
Pitrou I, Berbiche D, Vasiliadis HM. Mental health and satisfaction with primary care services in older adults: a study from the patient perspective on four dimensions of care. Fam Pract. 2020;37:459–64.
Winter PL, Keith RA. A model of outpatient satisfaction in rehabilitation. Rehabil Psychol. 1988;33:131–42.
Leung J, Fereday S, Sticpewich B, Stroud K. Factors influencing the overall satisfaction in patients with severe brain injury with physiotherapy services during inpatient rehabilitation. J Head Trauma Rehabil. 2018;33:E56–63.
Algudairi G, Al-Eisa ES, Alghadir AH, Iqbal ZA. Patient satisfaction with outpatient physical therapy in Saudi Arabia. BMC Health Serv Res. 2018;18:888.
Luthy C, Francis Gerstel P, Pugliesi A, Piguet V, Allaz AF, Cedraschi C, et al. Bedside or not bedside: Evaluation of patient satisfaction in intensive medical rehabilitation wards. PLoS ONE. 2017;12:e0170474.
Holmøy T, Hanssen KT, Beiske AG. Patient satisfaction in rehabilitation of patients with multiple sclerosis. Tidsskr Nor Laegeforen. 2012;132:523–6.
Hansson EE, Beckman A, Wihlborg A, Persson S, Troein M. Satisfaction with rehabilitation in relation to self-perceived quality of life and function among patients with stroke - a 12 month follow-up. Scand J Caring Sci. 2013;27:373–9.
Khosravi S, Khayyamfar A, Shemshadi M, Koltapeh MP, Sadeghi-Naini M, Ghodsi Z, et al. Indicators of quality of care in individuals with traumatic spinal cord injury: a scoping review. Glob Spine J 2022;12:166–81.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26 suppl. 1:S50–6.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multi-center international study on the spinal cord independence measure, version III: Rasch psychometricvalidation. Spinal Cord. 2007;45:275–91.
Scivoletto G, Glass C, Kim A, Galili T, Benjamin Y, Front L, et al. An international age and gender controlled model for the spinal cord injury ability realization measurement index (SCI-ARMI). Neurorehabil Neural Repair. 2015;29:25–32.
Jörgensen S, Hedgren L, Sundelin A, Lexell J. Global and domain-specific life satisfaction among older adults with long-term spinal cord injury. J Spinal Cord Med. 2021;44:322–30.
Kennedy P, Smithson E, McClelland M, Short D, Royle J, Wilson C, et al. Life satisfaction, appraisals and functional outcomes in spinal cord-injured people living in the community. Spinal Cord. 2010;48:144–8.
Tonack M, Hitzig SL, Craven BC, Campbell KA, Boschen KA, McGillivray CF, et al. Predicting life satisfaction after spinal cord injury in a Canadian sample. Spinal Cord. 2008;46:380–5.
Post MWM, van Dijk AJ, van Asbeck FWA, Schrijvers AJ. Life satisfaction of persons with spinal cord injurycompared to a population group. Scand J Rehab Med. 1998;30:23–30.
Van Leeuwen CMC, Post MWM, van Asbeck FWA, Bongers-Janssen HM, van der Woude LH, de Groot S, et al. Life satisfaction in people with spinal cord injury during the first five years after discharge from inpatient rehabilitation. Disabil Rehabil. 2012;34:76–83.
Tasiemski T, Kujawa J, Tederko P, Rubinelli S, Middleton JW, Craig A, et al. Comparison of life satisfaction in persons with spinal cord injury living in 22 countries with different economic status. Arch Phys Med Rehabil. 2021;102:1–27. online ahead of print.
Acknowledgements
We would like to thank Ms. Aida Dinia from Loewenstein Rehabilitation Medical Center, Ms. Polina Mikshevski from the service division of Clalit Health Services, and Ms. Zina Shatz, for their valuable assistance with the data analysis.
Funding
This study was supported by Loewenstein Rehabilitation Medical Center research fund KM600010275.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study (0036-16-LOE) was approved by the local ethics committee, in accordance with the principles of the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Michaeli, D., Kfir, A., Elkayam, K. et al. Satisfaction scores can be used to assess the quality of care and service in spinal rehabilitation. Spinal Cord 60, 1023–1029 (2022). https://doi.org/10.1038/s41393-022-00819-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00819-5