Abstract
Study design
Retrospective multicenter study.
Objectives
To investigate the neurological outcomes of older individuals treated with surgery versus conservative treatment for cervical spinal cord injury (CSCI) without bone injury.
Setting
Thirty-three medical institutions in Japan.
Methods
This study included 317 consecutive persons aged ≥65 years with CSCI without bone injury in participating institutes between 2010 and 2020. The participants were followed up for at least 6 months after the injury. Individuals were divided into surgery (n = 114) and conservative treatment (n = 203) groups. To compare neurological outcomes and complications between the groups, propensity score matching of the baseline factors (characteristics, comorbidities, and neurological function) was performed.
Results
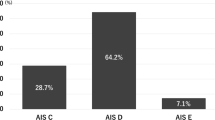
After propensity score matching, the surgery and conservative treatment groups comprised 89 individuals each. Surgery was performed at a median of 9.0 (3–17) days after CSCI. Baseline factors were comparable between groups, and the standardized difference in the covariates in the matched cohort was <10%. The American Spinal Injury Association (ASIA) impairment scale grade and ASIA motor score (AMS) 6 months after injury and changes in the AMS from baseline to 6 months after injury were not significantly different between groups (P = 0.63, P = 0.24, and P = 0.75, respectively). Few participants who underwent surgery demonstrated perioperative complications such as dural tear (1.1%), surgical site infection (2.2%), and C5 palsy (5.6%).
Conclusion
Conservative treatment is suggested to be a more favorable option for older individuals with CSCI without bone injuries, but this finding requires further validation.
Similar content being viewed by others
Introduction
Cervical spinal cord injury (CSCI) without bone injury is defined as a CSCI with no evidence of spinal fracture or dislocation on radiography or computed tomography [1]. This injury is typically the result of hyperextension of the cervical spine and can occur in the presence of pre-existing cervical stenosis [2, 3]. Due to a rapidly progressing aging society, the rate of CSCI without bone injury has been dramatically increasing in Japan [3,4,5]. A recent Japanese nationwide survey reported that the neurological level of traumatic spinal cord injury is most often located at the cervical level (88%), and CSCI without bone injury accounted for 71% of CSCI cases, which can often occur with minor trauma, such as falls on a level surface, in older people [6].
Although surgical reconstruction of the spinal column is not required for CSCI without bone injury, treatment has been historically variable among surgeons. Individual-specific characteristics are factors in treatment decisions. While some spine surgeons advocate surgery in persons who have evidence of pre-existing spinal cord compression and worsening or persistent neurological function, others recommend conservative treatment because no difference in the neurological outcome is observed after surgical decompression [3, 7,8,9,10,11,12,13]. Basically, pre-existing cervical canal stenosis is a different condition from unphysiological and instantaneous dynamic stenosis at the moment of injury [14]. Previous studies have demonstrated that the severity of motor deficit and neurological outcome do not correlate with the degree of pre-existing cervical canal stenosis in CSCI without bone injury [14,15,16,17].
The greatest limitation of previous studies was the small number of participants. Although this multicenter large cohort study is retrospective in nature, we evaluated the largest number of older individuals (aged ≥ 65 years) with CSCI without bone injury (n = 304); therefore, we provide stronger evidence than previous reports. The present study aimed to investigate the neurological outcomes of older persons who were treated with surgical decompression versus conservative treatment for CSCI without bone injury using propensity score matching to adjust for baseline factors.
Methods
Study participants
We reviewed a retrospective multicenter database of 1512 consecutive individuals aged ≥65 years with cervical spine/spinal cord injury in 33 domestic institutes between 2010 and 2020, which was performed by the Japan Association of Spine surgeons with Ambition. The study design was approved by the Institutional Review Boards of each hospital. Of the 1512 individuals, 614 were diagnosed with CSCI without bone injury: CSCI with no evidence of spinal fracture or dislocation on radiography and computed tomography [18]. We excluded individuals whose baseline American Spinal Injury Association (ASIA) motor score (AMS) was missing, whose AMS at 6 months after injury was missing but not because of death before 6-month follow-up, who had diagnostic delay (>24 h after injury), and who had initially been managed conservatively and underwent surgery due to percistance or deterioration of symptoms (Fig. 1). A total of 317 individuals who were followed up for at least 6 months after injury were included in the present study (Fig. 1). The 6-month time period was based on recommendations used in clinical trials [19, 20], and on the findings of previous studies that showed that the majority of the neurological recovery occurred during this period [21]. Participants were divided into two groups according to the therapeutic approach: surgery (n = 114) and conservative treatment (n = 203) groups. Surgical indications, techniques, and levels of decompression and/or fusion were determined at the discretion of the surgeons at each institute. Three different surgical techniques (anterior spinal fusion, posterior surgery, and combined anterior and posterior spinal fusion) were performed. The individuals treated conservatively were placed in a cervical collar. All participants underwent rehabilitation at each institute if their general condition was stable.
We reviewed a retrospective multicenter database of 1512 consecutive individuals aged ≥65 years with cervical spine/spinal cord injury in 33 domestic institutes between 2010 and 2020, which was performed by the Japan Association of Spine surgeons with Ambition. A total of 317 individuals who were followed up for at least 6 months after injury were included in the present study.
Data collection
Individuals’ demographic data (age, sex, body mass index, medical history, and mechanism of injury) were retrospectively obtained. Post-injury days to surgery, surgical technique, operation time, and blood loss were recorded by the attending spine surgeon. Computed tomography scans were used to detect the bone injury. T1- or T2-weighted sagittal and axial magnetic resonance imaging (MRI) scans were used to determine the signal intensity (SI) changes in the spinal cord. Senior spine surgeons and physical therapists at each hospital evaluated the neurological status using the ASIA Impairment Scale (AIS) and AMS on admission and 6 months after injury. We defined the time window in the study protocol for 6-month data as 6 to 11 months after injury. Central cord syndrome was defined as an upper extremity AMS of at least 10 points fewer than the lower extremity AMS on admission [22]. The indication and dose of steroid therapy for CSCI were decided at the discretion of the spine surgeons at each hospital. Perioperative complications (dural tear, surgical site infection [SSI], and C5 palsy) and in-hospital complications (moror or sensory neurological deterioration, cardiac infarction, cerebral infarction, delirium, dysphagia, respiratory failure, pulmonary embolism, pneumonia, and renal infection) were monitored. C5 palsy was defined as postoperative unilateral deterioration of muscle strength localized in the deltoid and biceps by one or more grades according to a manual muscle test conducted within 1 month after surgery. Because C5 palsy was a surgery-specific complication, we divided C5 palsy from other forms of motor deterioration in this study.
Statistical analysis
Baseline characteristics, comorbidities, perioperative and post-injury data, and neurological outcomes were compared between the surgery and conservative treatment groups using an unpaired t-test or the Mann-Whitney U test for continuous variables and a chi-square test for categorical variables, as appropriate for each data distribution. Propensity score-matched analysis was performed to compare neurological outcomes and complications between the groups. A logistic regression model was used to calculate propensity scores. The moderator variables were age, sex, body mass index, comorbidities, cervical ossification of the posterior longitudinal ligament (OPLL), SI changes on MRI, baseline AIS grade, central cord syndrome, baseline AMS, and steroid therapy for CSCI. To adjust for baseline characteristics and comorbidities, 1-to-1 matching with fixed caliper widths (0.01) without replacement was performed. A case in the surgery group was matched to a case in the conservative treatment group with the same propensity score. Pairs consisting of one patient who underwent surgery and one patient who underwent conservative treatment were collected to form two groups: surgery and conservative treatment. We used the standardized difference to measure covariate balance. A standardized difference of <10% was considered to indicate a negligible difference between the groups. A comparison of the AMS between baseline and 6 months after injury was performed using a paired t-test. All statistical analyses were performed using SPSS software (version 26.0, IBM Corporation, Armonk, NY, USA). Continuous variables are presented as mean standard deviation (SD) or median (interquartile range). Statistical significance was set at P < 0.05.
Results
Baseline characteristics and comorbidities according to the therapeutic approach
Our cohort of 317 individuals consisted of 221 men (70%) and 96 women (30%), with a mean age at injury (mean SD) of 75 (6.7) years. The percentage of participants who underwent surgery was 36%. Individuals in the surgery group showed a higher prevalence of cervical OPLL, higher proportion of SI changes on MRI, and worse baseline AIS grade than did those in the conservative treatment group (P < 0.01, P < 0.01, and P < 0.01, respectively). The baseline AMS in the surgery group was on average 10 (95% CI, 2.9–17) lower than that in the conservative treatment group. There were no significant differences in sex ratio, body mass index, mechanism of injury, steroid therapy for CSCI, and prevalence of hypertension, diabetes mellitus, cardiac disease, respiratory disease, renal disease, cerebrovascular disease, or central cord syndrome between the surgery and conservative treatment groups (Table 1).
Perioperative and post-injury data according to the therapeutic approach
Surgery was performed at a median of 7.5 days after the injury. Anterior spinal fusion, posterior surgery (decompression and/or fusion), and combined anterior and posterior spinal fusion were performed in 2.6% (n = 3), 96% (n = 110), and 0.88% (n = 1) of participants in the surgery group, respectively. Fusion surgery was performed in 25% (n = 28) of the individuals who underwent posterior surgery. Perioperative complications (dural tear, SSI, or C5 palsy) were observed in a small proportion of the participants who underwent surgery (0.88%, 1.8%, and 4.4%, respectively) (Table 2). No significant differences were found between the surgery and conservative treatment groups regarding the in-hospital complication rates for neurological deterioration (motor or sensory), cardiac infarction, cerebral infarction, delirium, dysphagia, respiratory failure, pulmonary embolism, or pneumonia. However, individuals in the surgery group showed a higher complication rate for renal infection than did those in the conservative treatment group (P < 0.01) (Table 2). There was no significant difference in the death rates before 6-month follow-up between the surgery and conservative treatment groups (Table 2). Although AMS at 6 months after injury in the surgery group was on average 7.3 (95% CI, 1.6–13) lower than that in the conservative treatment group, we observed greater changes in the AMS from baseline to 6-month post-injury in the surgery group (P = 0.02). The rate of low AIS grade was higher in the surgery group than in the conservative group at 6 months after the injury (P = 0.03) (Table 2). Both groups showed improvement in the AMS at the 6-month follow-up (surgery group: 21 ± 21, 95% CI, 17–25, P < 0.01; conservative treatment group: 16 ± 20, 95% CI, 14–19, P < 0.01).
Propensity score-matched comparison of baseline characteristics and comorbidities
There were 89 individuals each in the surgery and conservative treatment groups after propensity score matching of baseline characteristics, comorbidities, and neurological function. The standardized difference in covariates in the matched cohort was <10%. No significant differences were noted between the groups in terms of age at surgery, sex ratio, body mass index, prevalence of comorbidities, cervical OPLL, central cord syndrome, mechanism of injury, SI changes on MRI, baseline AIS grade, baseline AMS, and steroid therapy for CSCI (Table 3).
Propensity score-matched comparison of perioperative data and complications
Surgery was performed at a median of 9.0 days after injury. Anterior spinal fusion, posterior surgery (decompression and/or fusion), and combined anterior and posterior spinal fusion were performed in 2.2% (n = 2), 97% (n = 86), and 1.1% (n = 1) of participants in the surgery group, respectively. Fusion surgery was performed in 8.1% (n = 7) of the individuals who underwent posterior surgery. Perioperative complications (dural tear, SSI, or C5 palsy) were observed in a small proportion of the participants who underwent surgery (1.1%, 2.2%, and 5.6%, respectively) (Table 4). No difference was observed in the in-hospital complication rates for neurological deterioration (sensory), cerebral infarction, delirium, dysphagia, respiratory failure, pneumonia, or renal infection between the groups. Neurological deterioration (motor), cardiac infarction, and pulmonary embolism were not observed in either group (Table 4). There was no significant difference in the death rates before 6-month follow-up between the groups (Table 4).
Propensity score-matched comparison of AMS and AIS grade at 6 months after injury according to the therapeutic approach
AIS grade, AMS at 6 months after injury, and the change in AMS from baseline to 6-month post injury were not significantly different between the groups (Table 4). Both groups showed improvement in the AMS at the 6-month follow-up (surgery group: 18 ± 20, 95% CI, 13 to 22, P < 0.01; conservative treatment group: 21 ± 22, 95% CI, 16 to 25, P < 0.01).
Discussion
To the best of our knowledge, this is the first multicenter large cohort study using propensity score-matched analysis to compare neurological outcomes and complications between surgery and conservative treatment groups after CSCI without bone injury in older individuals. Because AIS grade and AMS at 6 months after injury and changes in the AMS at the 6-month follow-up were not significantly different between the groups, neurological recovery in the two treatment groups was comparable. Although the rates of death before 6-month follow-up and the rates of other in-hospital complications were not significantly different between the groups, perioperative complications were observed in a small proportion of the participants in the surgery group. We suggest that conservative treatment is a better option for older individuals with CSCI without bone injuries.
The management of CSCI without bone injury has remained controversial with previous studies comparing surgery with conservative treatment. Chen et al. reported that surgical decompression was associated with immediate neurological recovery and a better long-term functional outcome compared with conservative treatment [7]. Although the following studies were not compared with conservative treatment, Uribe et al. and Song et al. concluded that surgical treatment improved neurological status and prevented neurological deterioration [23, 24]. Conversely, Kawano et al. reported no difference in the neurological recovery between the surgery and conservative treatment groups [3]. Another study conducted by Mazaki et al. also showed that neurological improvement does not change with surgical treatment, although they observed a higher complication rate in individuals who underwent surgery [4]. Ishida et al. reported that participants who underwent conservative treatment had significant neurological improvement and none of them required surgery [17]. In the present study, a higher prevalence of cervical OPLL, higher proportion of SI changes on MRI, worse baseline AIS grade, and lower baseline AMS were observed in the surgery group than in the conservative treatment group before propensity score matching. These findings indicate that spine surgeons in Japan tend to perform surgery for cervical OPLL in individuals with more severe CSCI without bone injury. Before propensity score matching, the surgery group showed greater improvement in the AMS at the 6-month follow-up, suggesting a positive effect of surgery on neurological recovery. However, after excluding the confounding factors by propensity score-matched analysis, neurological recovery (changes in the AMS at the 6-month follow-up) were not significantly different between the surgery and conservative treatment groups. Although the frequency of other in-hospital complications was similar between the groups, it is important to consider that perioperative complications such as dural tear, SSI, or C5 palsy were observed in a small proportion of participants who were treated surgically. Conservative treatment is suggested to be a better option for older individuals with CSCI without bone injuries.
Recent studies revealed that early decompressive surgery within 24 h of spinal cord injury was associated with improved neurological recovery [25, 26]. Conversely, a randomized clinical trial of motor-incomplete CSCI without bone injury in participants aged 20 to 79 years revealed that early surgery within 24 h of spinal cord injury produced motor recovery at 1 year after injury comparable to that of late surgery, but demonstrated accerelated recovery within the first 6 months [27]. Because the number of participants who underwent early surgery prior to 24 h after spinal cord injury was small (n = 9) in the present study, we did not statistically compare early surgery with late surgery. Further studies are necessary to determine the benefits of early surgery in older individuals with CSCI without bone injuries.
Limitations
There are potential limitations to the present study. This was a retrospective study that included a selection bias. We realize that a substantial number of participants were lost to the 6-month follow-up. Compared with those who completed follow-up, those who were lost to follow-up showed older age, higher mortality rate, higher prevalence of respiratory disease, and lower baseline AMS (Table S1). Treatment strategy (surgery, conservative treatment, or initial conservative treatment converted to surgery) did not affect the 6-month follow-up rate (Table S2). Because of the small sample size (n = 178) after propensity-score matching, the possibility of a type II error should be acknowledged. Historically, Japanese spine surgeons usually perform elective surgery in individuals with CSCI without bone injury. Similar to a previous study in Japan, in our study, surgery was performed at a median of 7.5 days after injury before propensity-score matching, which may affect the results of the present study [3]. We only included inpatients in acute hospitals and excluded outpatients, resulting in a higher proportion of individuals who underwent surgery. The indications for surgery or conservative treatment and choice of surgical technique were left to the discretion of the surgeon at each hospital. The conservative treatment and rehabilitation program were not standardized due to the lack of a universally accepted care bundle. In general, surgeons tend to perform surgery for individuals with smaller cervical canals, which may result in a difference in cervical canal size between surgery and conservative treatment groups. Because cervical canal diameter data were not obtained in the present study, the influence of cervical canal size on neurological outcomes was not evaluated. Further studies are necessary to determine the influence of degree of pre-existing cervical canal stenosis on neurological outcomes. Because we did not have preoperative (just before surgery) neurological data of individuals who had initially been managed conservatively and underwent surgery due to persistence or deterioration of symptoms, those participants were excluded from the present study. Therefore, this study did not evaluate the effect of surgery on persons with persistent or deteriorated symptoms. We did not evaluate the neurological outcomes over the long term (>6 months after injury) in the present study. Further studies are necessary to determine the benefits of surgery over the long term in individuals with pre-existing cervical stenosis. Biases caused by propensity score matching could have occurred because we did not use data from unmatched participants in the analysis of post-injury outcomes. Therefore, future prospective studies with larger sample sizes may be required to confirm the results of the present study.
Conclusion
In the present study, surgery was performed at a median of 9.0 (3.0–17) days after CSCI without bone injury after propensity-score matching. Neurological recovery was comparable between surgery and conservative treatment after CSCI without bone injury in older individuals. A small proportion of the participants who underwent surgery demonstrated perioperative complications. Conservative treatment is suggested to be a better option for older individuals with CSCI without bone injuries; however, this finding requires further validation.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Maeda T, Ueta T, Mori E, Yugue I, Kawano O, Takao T, et al. Soft-tissue damage and segmental instability in adult patients with cervical spinal cord injury without major bone injury. Spine. 2012;37:E1560–6.
Chikuda H, Seichi A, Takeshita K, Matsunaga S, Watanabe M, Nakagawa Y, et al. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine. 2011;36:1453–8.
Kawano O, Ueta T, Shiba K, Iwamoto Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study. Spinal Cord. 2010;48:548–53.
Mazaki T, Ito Y, Sugimoto Y, Koshimune K, Tanaka M, Ozaki T. Does laminoplasty really improve neurological status in patients with cervical spinal cord injury without bone and disc injury? A prospective study about neurological recovery and early complications. Arch Orthop Trauma Surg. 2013;133:1401–5.
Nakajima H, Takahashi A, Kitade I, Watanabe S, Honjoh K, Matsumine A. Prognostic factors and optimal management for patients with cervical spinal cord injury without major bone injury. J Orthop Sci. 2019;24:230–6.
Miyakoshi N, Suda K, Kudo D, Sakai H, Nakagawa Y, Mikami Y, et al. A nationwide survey on the incidence and characteristics of traumatic spinal cord injury in Japan in 2018. Spinal Cord. 2021;59:626–34.
Chen TY, Dickman CA, Eleraky M, Sonntag VK. The role of decompression for acute incomplete cervical spinal cord injury in cervical spondylosis. Spine. 1998;23:2398–403.
Donovan WH. Operative and nonoperative management of spinal cord injury. A review. Paraplegia. 1994;32:375–88.
Gupta SK, Rajeev K, Khosla VK, Sharma BS, Paramjit, Mathuriya SN, et al. Spinal cord injury without radiographic abnormality in adults. Spinal Cord. 1999;37:726–9.
Newey ML, Sen PK, Fraser RD. The long-term outcome after central cord syndrome: a study of the natural history. J Bone Jt Surg Br 2000;82:851–5.
Papadopoulos SM, Selden NR, Quint DJ, Patel N, Gillespie B, Grube S. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma. 2002;52:323–32.
Saruhashi Y, Hukuda S, Katsuura A, Asajima S, Omura K. Clinical outcomes of cervical spinal cord injuries without radiographic evidence of trauma. Spinal Cord. 1998;36:567–73.
Stevens EA, Marsh R, Wilson JA, Sweasey TA, Branch CL Jr., Powers AK. A review of surgical intervention in the setting of traumatic central cord syndrome. Spine J. 2010;10:874–80.
Takao T, Okada S, Morishita Y, Maeda T, Kubota K, Ideta R, et al. Clinical influence of cervical spinal canal stenosis on neurological outcome after traumatic cervical spinal cord injury without major fracture or dislocation. Asian Spine J. 2016;10:536–42.
Okada S, Maeda T, Ohkawa Y, Harimaya K, Saiwai H, Kumamaru H, et al. Does ossification of the posterior longitudinal ligament affect the neurological outcome after traumatic cervical cord injury? Spine. 2009;34:1148–52.
Katoh S, el Masry WS, Jaffray D, McCall IW, Eisenstein SM, Pringle RG, et al. Neurologic outcome in conservatively treated patients with incomplete closed traumatic cervical spinal cord injuries. Spine. 1996;21:2345–51.
Ishida Y, Tominaga T. Predictors of neurologic recovery in acute central cervical cord injury with only upper extremity impairment. Spine. 2002;27:1652–8.
Kawano O, Maeda T, Mori E, Yugue I, Takao T, Sakai H, et al. Influence of spinal cord compression and traumatic force on the severity of cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine. 2014;39:1108–12.
Geisler FH, Coleman WP, Grieco G, Poonian D. The Sygen multicenter acute spinal cord injury study. Spine. 2001;26:S87–98.
Bracken MB, Shepard MJ, Holford TR, Leo-Summers L, Aldrich EF, Fazl M, et al. Administration of methylprednisolone for 24 or 48 h or tirilazad mesylate for 48 h in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277:1597–604.
Burns AS, Ditunno JF. Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine. 2001;26:S137–45.
van Middendorp JJ, Pouw MH, Hayes KC, Williams R, Chhabra HS, Putz C, et al. Diagnostic criteria of traumatic central cord syndrome. Part 2: a questionnaire survey among spine specialists. Spinal Cord. 2010;48:657–63.
Song J, Mizuno J, Nakagawa H, Inoue T. Surgery for acute subaxial traumatic central cord syndrome without fracture or dislocation. J Clin Neurosci. 2005;12:438–43.
Uribe J, Green BA, Vanni S, Moza K, Guest JD, Levi AD. Acute traumatic central cord syndrome-experience using surgical decompression with open-door expansile cervical laminoplasty. Surg Neurol. 2005;63:505–10. discussion 510
Badhiwala JH, Wilson JR, Witiw CD, Harrop JS, Vaccaro AR, Aarabi B, et al. The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol. 2021;20:117–26.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS. et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE. 2012;7:e32037
Chikuda H, Koyama Y, Matsubayashi Y, Ogata T, Ohtsu H, Sugita S, et al. Effect of early vs delayed surgical treatment on motor recovery in incomplete cervical spinal cord injury with preexisting cervical stenosis: a randomized clinical trial. JAMA Netw Open. 2021;4:e2133604.
Acknowledgements
The authors acknowledge the contributions of the members of the 33 participating institutions in the assistance with data collection. The authors thank Naoki Miyazaki, MPH, Kengo Nagahima, PhD, and Noriyuki Ishida, MPH for their help with the statistical analyses in the study.
Author information
Authors and Affiliations
Contributions
SN and KW designed the research. SN analyzed the data. SN and KW wrote the paper. SN, KT, JY, HK, NY, TS, HN, NS, TF, FE, AY, AY, HN, TY, TH, YT, RH, HS, YI, SI, MU, HT, MS, KH, YO, KK, YH, NS, KK, HU, HS, KN, KM, HT, KT, ES, KK, YI, ET, HF, TY and MI performed data collection. KA, GI, TK, SK, TF, KW, SO, and SI supervised the study. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study received ethical approval from the institutional review board of the representative facility (Keio University School of Medicine, No. 20200233). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nori, S., Watanabe, K., Takeda, K. et al. Does surgery improve neurological outcomes in older individuals with cervical spinal cord injury without bone injury? A multicenter study. Spinal Cord 60, 895–902 (2022). https://doi.org/10.1038/s41393-022-00818-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00818-6