Abstract
Study design
Retrospective cross-sectional epidemiological study.
Objectives
Previous studies have quantified longitudinal psychological morbidity in individuals with spinal cord injury (SCI) relative to uninjured individuals. However, there is limited information regarding how lifestyle and socioeconomic factors are associated with mental health conditions in individuals with SCI. This study aims to quantify and compare mental health and suicidal thoughts in people with and without SCI, and examine the associations between mental health, suicidal thoughts, sex, age, lifestyle, and socioeconomic factors.
Setting
Canada.
Methods
The 2010 Canadian Community Health Survey (n > 40,000) was used, which includes several measures assessing mental health and suicidal thoughts. Bivariate and multivariate logistic regressions were performed and odds ratios with corresponding 95% confidence intervals were estimated. Sensitivity analyses were performed to evaluate the effect of covariates on reported effect sizes.
Results
People with SCI had higher odds of having mood (3.6) and anxiety disorders (2.5), suicidal thoughts (2.3), self-perceived stress (1.9), and depression (4.4); in addition to lower odds of having good self-perceived mental health (0.24) and satisfaction with life (0.25). These differences persisted after adjusting for age, sex, lifestyle, and socioeconomic factors. Lower household income, fruit and vegetable consumption, and physical activity levels, and increased smoking use were associated with poorer mental health in individuals with SCI.
Conclusions
Mental health is poorer in those with SCI when compared with the general population. Those with SCI exhibit a unique profile of lifestyle and socioeconomic factors that are associated with poorer mental health and increased suicidal thoughts.
Similar content being viewed by others
Introduction
Mental health is a major public health issue that affects people with disability disproportionately [1]. Comorbidity of poor mental health affects the diagnosis, treatment, and prognosis of several physical health conditions, leading to an inequitable provision of health services for those with mental disorders [2]. In fact, mental health conditions contribute to over a quarter of the disability-adjusted life-years attributed to non-communicable diseases [2].
Spinal cord injury (SCI) is a disabling condition; however, it is unclear how much comorbid mental health conditions contribute to the challenges faced by this population. A survey from Australia found that nearly half of the SCI cohort in Victoria experienced mental disorders such as depression, anxiety, chronic stress, or post-traumatic stress disorder [3]. Other studies have shown that people with SCI have associated long-term psychosocial consequences such as suicide and depression [4, 5]. However, the relative burden of these mental health conditions is unclear as previous studies have largely examined their impact within individuals with SCI without comparing to the general population [6,7,8].
An additional limitation to the current literature on mental health in the SCI population is a failure to consider lifestyle and socioeconomic factors that associate with both SCI and mental health conditions. These include alcohol consumption, diet, income, education, race, and physical activity levels [9,10,11,12,13,14]. Differential associations exist between these factors and outcomes in the general population [15,16,17], which may allow tailored interventions to SCI. However, direct comparisons of these populations to date have not considered lifestyle and socioeconomic factors [18]. Having this population-level evidence regarding mental health is imperative for managing healthcare resources, directing future research, and adapting treatment plans for people with SCI.
To address these limitations, this study used data from the Canadian Community Health Survey (CCHS) to compare the prevalence of mental health conditions among individuals with SCI and the general population, as well as the influence of lifestyle and socioeconomic factors.
Methods
Data source
This study used data from the CCHS 2010 Annual Component [19]. The CCHS is a comprehensive national cross-sectional survey conducted by Statistics Canada which provides data on interviews conducted on individuals aged 12 years and older residing in households across all Canadian provinces and territories. Those living on reserves or Crown lands, full-time members of the Canadian armed forces, and those living in institutions (i.e., prisons, hospitals, universities) are excluded from the survey. Outcomes were grouped into two categories: core content, which involves sections of the CCHS that were answered by all participating provinces and territories, and optional content, which are sections that provinces chose to exclude in their questionnaires. The Tri-Council Policy Statement on Ethical Conduct for Research Involving Humans states that the use of publicly available information, such as Statistics Canada data, is exempt from review by institutional research ethics boards, as it is publicly available and does not contain any identifiers. This policy was confirmed by the University of Calgary Conjoint Health Research Ethics Board.
Exposure and outcomes
SCI status was determined by the following question: “Do you have a neurologic condition caused by spinal cord injury?”. The primary outcome variables of interest in this analysis were self-reported mood disorders such as depression, anxiety disorders, suicidal thoughts, self-perceived mental health, self-perceived stress, and general satisfaction with life. Although depression is pooled within mood disorders in the CCHS, it was also analyzed separately as SCI is associated with increased risk of de novo depression rather than mood disorders characterized by mania/hypomania [20, 21]. All variables with the exception of depression and suicidal ideation are under CCHS core content [19]. Optional content includes depression (answered by P.E.I., Quebec, Saskatchewan, Alberta, B.C., N.W.T., and Nunavut, corresponding to 46.8% of total sample) and suicidal thoughts (answered by N.L., Alberta, B.C., and Nunavut, corresponding to 23.3% of total sample) [19].
An individual could answer “Yes” or “No” to the following questions to assess the status of select outcomes: “Do you have a mood disorder such as depression, bipolar disorder, mania or dysthymia?”, “Do you have an anxiety disorder such as a phobia, obsessive-compulsive disorder or a panic disorder?”, “Have you ever seriously considered committing suicide or taking your own life?”.
The following prompt was used to assess self-perceived stress: “Thinking about the amount of stress in your life, would you say that most days are:”. Individuals who responded “…not at all stressful?” or “…not very stressful?” were categorized as having no stress, while those who responded “…a bit stressful?”, “…quite a bit stressful?”, or “…extremely stressful?” were categorized as having stress. The following prompt was used to assess self-perceived mental health: “In general, would you say your mental health is:”. Individuals who responded with “…poor” or “…fair” were categorized as having low self-perceived mental health, while those who responded “…good”, “…very good”, or “…excellent” were categorized as having high self-perceived mental health. One or more variables for general satisfaction with life and depression were grouped into derived variables [22]. For general satisfaction with life, individuals who were classified as “very dissatisfied” or “dissatisfied” were categorized as having low satisfaction with life, while those who were classified as “neither satisfied nor dissatisfied”, “satisfied”, or “very satisfied” were categorized as having high satisfaction with life. For depression, individuals who were classified as having “felt depressed for 2 weeks or more last year” were categorized as having depression, while those who were classified as “did not feel depressed or did not lose interest in things for two weeks last year, or did so only mildly” were categorized as having no depression. Details on dichotomization are provided in Supplementary Table 1. Individuals received the following reminder in the survey: “Remember, we’re interested in conditions diagnosed by a health professional.”
Confounders
Confounders analyzed in this study included age and sex, as they are known risk factors for both traumatic and non-traumatic SCI [23]. Sensitivity analyses were performed to examine the effect of additional self-report covariates (body mass index [BMI], and lifestyle and socioeconomic factors such as physical activity, fruit and vegetable consumption, smoking status, alcohol consumption, household income, educational attainment, and racial identity) on the reported effect sizes.
BMI was categorized based on whether individuals were less than the median BMI of all included respondents, or greater than or equal to the median BMI. Individuals who were classified as “active”, “moderately active”, “regular practice of leisure time activities”, or “occasional practice of leisure time activities” were categorized as having high physical activity, while those who were classified as “inactive” or “infrequent practice of leisure time activities” were categorized as having low physical activity. Individuals who indicated that they consumed fruits and vegetables at least five times per day were categorized as having high fruit and vegetable consumption, while those who indicated otherwise were categorized as having low fruit and vegetable consumption. Individuals who indicated that they have smoked at least one whole cigarette in their lifetime were categorized as being smokers, while those who indicated that they have never smoked a whole cigarette were categorized as non-smokers. Individuals who indicated that they have consumed at least one alcoholic drink in the last 12 months were categorized as drinkers, while those who indicated that they have not consumed an alcoholic drink in the last 12 months were categorized as non-drinkers. Individuals who indicated some post-secondary education or completion of a post-secondary degree/diploma were categorized as having high educational attainment, while those without post-secondary education were categorized as having low educational attainment. For racial identity, individuals were categorized as either White or Non-white. Details on dichotomization are provided in Supplementary Tables 2, 3.
Exclusion criteria
Only individuals with valid responses for the primary explanatory variable, outcome variables, and covariates were included in the analysis. Non-respondents (i.e., “don’t know”, “refusal”, and “not stated”) were excluded. Details on dichotomization and sample characteristics are provided in Supplementary Table 4.
Statistical analysis
Logistic regression models were used to assess the relationships between the main explanatory variable (SCI) and the outcome variables. Logistic regression models were generated for each outcome independently using the “glm” (generalized linear model) function with the family “binomial()” in the R package “stats”. Initially, bi-variable logistic regression models with SCI status as the main explanatory variable were used to generate unadjusted odds ratios (ORs). The models were then adjusted for age, sex, and BMI (aOR1) along with lifestyle and socioeconomic factors (aOR2) using multivariable logistic regression to generate adjusted odds ratios. Using the results from these logistic models, both unadjusted and adjusted ORs with corresponding 95% confidence intervals (CIs) are presented. Statistical significance was defined as p value ≤ 0.05. This analysis accounted for the CCHS sampling design (i.e., clustering and stratification) by using probability weighting provided by Statistics Canada. R (R Core Team, 2017) was used for all statistical analyses.
Results
Overall sample characteristics
After removing non-respondents, each outcome measure in the CCHS was completed by the following number of participants: mood disorders (n = 45,691), anxiety disorders (n = 45,689), suicidal thoughts (n = 10,639), self-perceived mental health (n = 45,694), stress (n = 45,659), general satisfaction with life (n = 45,551), and depression (n = 21,398). A similar proportion of males and females completed the survey; however, there were slightly more females (~53%) than males (~47%) included in most outcome measurements (Tables 1, 2). The overall sample had a median age range of 45-54 years and a median body mass index (BMI) of ~25.5 kg/m2 (Tables 1, 2).
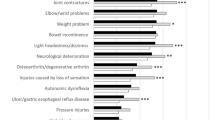
Individuals with SCI have elevated odds of experiencing mood disorders compared with individuals without SCI. The prevalence of mood disorders in individuals without SCI was 7.6%, and 25% in those with SCI (Table 1). The unadjusted OR of self-reporting mood disorders for individuals with SCI was 4.4 (95% CI, 3.1–6.0; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 4.6 (95% CI, 3.3–6.4; Table 3). Controlling for all the covariates decreased the OR to 3.6 (95% CI, 2.5–5.1; Table 3). Covariates that were significantly associated with mood disorders in those with SCI include higher BMI (2.0, 95% CI, 1.2–3.6), lower alcohol consumption (0.46, 95% CI, 0.26–0.82), lower income (3.1, 95% CI, 1.7–5.9), and lower physical activity (0.38, 95% CI, 0.21–0.66) (Fig. 1).
Individuals with SCI have elevated odds of experiencing depression compared with individuals without SCI. The prevalence of experiencing depression in individuals without SCI was 8.6%, and 27% in those with SCI (Table 1). The unadjusted OR of self-reporting depression for individuals with SCI was 4.0 (95% CI, 2.3–6.4; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 5.3 (95% CI, 3.1–8.8; Table 3). Controlling for all the covariates decreased the OR to 4.4 (95% CI, 2.5–7.4; Table 3). Covariates that were significantly associated with depression in those with SCI include older age (8.5, 95% CI, 2.9–33), lower BMI (0.37, 95% CI, 0.16–0.86), lower smoking use (0.27, 95% CI, 0.09–0.71), higher fruit and vegetable consumption (2.8, 95% CI, 1.2– 6.8), lower income (0.33, 95% CI, 0.13–0.81), and higher physical activity (3.7, 95% CI, 1.6–8.9) (Fig. 1).
Individuals with SCI have elevated odds of experiencing anxiety disorders compared with individuals without SCI. The prevalence of anxiety disorders in individuals without SCI was 5.6%, and 17% in those with SCI (Table 1). The unadjusted OR of self-reporting anxiety disorders for individuals with SCI was 2.9 (95% CI, 1.9–4.2; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 3.3 (95% CI, 2.1–4.9; Table 3). Controlling for all the covariates decreased the OR to 2.5 (95% CI, 1.6–3.8; Table 3). Covariates that were significantly associated with anxiety disorders in those with SCI include higher smoking use (6.7, 95% CI, 2.7–21), lower income (7.0, 95% CI, 3.3–15), and lower physical activity (0.47, 95% CI, 0.24–0.90) (Fig. 1).
Individuals with SCI have elevated odds of experiencing suicidal thoughts compared with individuals without SCI. The prevalence of suicidal thoughts in individuals without SCI was 10%, and 21% in those with SCI (Table 1). The unadjusted OR of self-reporting suicidal thoughts for individuals with SCI was 2.7 (95% CI, 1.4–4.9; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 3.0 (95% CI, 1.5–5.4; Table 3). Controlling for all the covariates decreased the OR to 2.3 (95% CI, 1.2–4.3; Table 3). Covariates that were significantly associated with suicidal thoughts in those with SCI include higher smoking use (14, 95% CI, 4.1–81), lower fruit and vegetable consumption (0.25, 95% CI, 0.87–0.63), lower income (2.9, 95% CI, 1.0–8.4), and lower physical activity (0.24, 95% CI, 0.09–0.60) (Fig. 1).
Individuals with SCI have elevated odds of experiencing stress compared with individuals without SCI. The prevalence of experiencing stress in individuals without SCI was 61%, and 74% in those with SCI (Table 2). The unadjusted OR of self-reporting stress for individuals with SCI was 1.6 (95% CI, 1.2–2.2; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 2.0 (95% CI, 1.4–2.8; Table 3). Controlling for all the covariates slightly decreased the OR to 1.9 (95% CI, 1.4–2.7; Table 3). Covariates that were significantly associated with increased stress in those with SCI include older age (7.4, 95% CI, 2.3–30 (Fig. 1).
Individuals with SCI have decreased odds of experiencing good self-perceived mental health compared with individuals without SCI. The prevalence of poor self-perceived mental health in individuals without SCI was 5.8%, and 21% in those with SCI (Table 2). The unadjusted OR of self-reporting good self-perceived mental health for individuals with SCI was 0.17 (95% CI, 0.12–0.24; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 0.17 (95% CI, 0.13–0.25; Table 3). Controlling for all the covariates increased the OR to 0.24 (95% CI,: 0.17–0.35; Table 3). Covariates that were significantly associated with poor self-perceived mental health in those with SCI include older age (7.4, 95% CI, 2.3–30) (Fig. 1).
Individuals with SCI have decreased odds of experiencing good satisfaction with life compared with individuals without SCI. The prevalence of experiencing poor satisfaction with life in individuals without SCI was 2.8%, and 14% in those with SCI (Table 2). The unadjusted OR of self-reporting good satisfaction with life for individuals with SCI was 0.14 (95% CI, 0.09–0.20; Table 3). Controlling for age, sex, and BMI slightly increased the OR to 0.15 (95% CI, 0.11–0.23; Table 3). Controlling for all the covariates increased the OR to 0.25 (95% CI, 0.17–0.39; Table 3). Covariates that were significantly associated with decreased satisfaction with life in those with SCI include lower alcohol consumption (0.35, 95% CI, 0.17–0.71) (Fig. 1).
Discussion
This study showed that SCI is associated with reduced mental health and increased suicidal thoughts. This result persisted after adjustment for age, sex, BMI, and various lifestyle and socioeconomic factors. Specifically, those with SCI had an increased likelihood of experiencing stress, anxiety disorders, mood disorders, suicidal thoughts, and depression. Additionally, SCI is associated with reduced self-perceived mental health and general satisfaction with life. For context, these ORs are similar for the relationship between several neurological conditions (e.g., migraine, traumatic brain injury, spina bifida, stroke, dystonia, and epilepsy) and experiencing depression [24].
Poor mental health in people with SCI may be the result of several factors, such as poor structural social relationships, financial strain and low life satisfaction [4, 15]. Previous studies have shown that approximately half of people with SCI experience some sort of mental health disorder and that SCI is associated with long-term psychosocial consequences such as suicidal thoughts and behaviors [3,4,5]. Others have shown high prevalence rates of depression and anxiety disorders, as well as poor subjective well-being in people with SCI [4]. A recent study on a large sample of individuals in the United States with private insurance benefits has shown that people with SCI have a significantly higher risk for developing anxiety disorders, adjustment reactions, depressive disorders, psychogenic pain, dementia, drug dependence, and psychological multimorbidity compared with the general population [18]. However, this study did not examine the influence of important factors such as physical activity levels and dietary factors (i.e., fruit and vegetable consumption) on mental health outcomes [18]. Moreover, these studies did not consider the associations between lifestyle and socioeconomic factors and mental health [6,7,8]. Here, we provide additional support for these findings on a population-scale with control individuals and adjustments for critical confounding variables.
From our data, a unique profile of lifestyle and socioeconomic factors within the SCI population demonstrated associations with poorer mental health. Low income, fruit and vegetable consumption, and physical activity levels, as well as increased smoking, were associated with reduced mental health in the SCI population (Fig. 1). Conversely, higher income, eating more fruits and vegetables, and engaging in more physical activity, as well as not smoking were associated with better mental health in those with SCI. Although a direct causal relationship cannot be determined from our data, targeting specific demographics within the SCI population, such as those with poor physical activity levels and high smoking use, could be an effective measure in improving and promoting their mental health. Our findings indicate that improving physical activity, diet, and reducing smoking are linked to better mental health outcomes in those with SCI. These behaviors are associated with improved health across numerous domains and are already recommended for the SCI population [25]. Interventional studies testing if improving physical activity, diet, and reducing smoking improves mental health outcomes in those with SCI are justified to further establish this association. Moreover, key research designs, such as additional longitudinal studies, will be needed to understand the existence of a causal relationship between SCI and mental health, and whether this relationship can withstand interventions. Our findings also suggest that the care of SCI patients should be adapted to include psychiatric specialists to conduct regular psychological consultations and manage patient care. Unfortunately, accessibility for healthcare services, especially from specialists, drastically decreases following SCI, resulting in few patients receiving their required treatments and services [18].
Limitations to the current study include the nature of cross-sectional data and self-report. Regarding self-report specifically, respondents may have difficulties regarding sensitive topics such as suicidal thoughts; however, any misclassification would likely be non-differential by SCI/non-SCI status. We also do not know if respondents experienced mental disorders or poor mental health before, or after, their spinal injury. Additionally, the CCHS does not include information on injury level or severity, which may impact the prevalence of mental health conditions that SCI patients may experience [26,27,28]. BMI is also measured differently in those with SCI [29], which may contain inaccuracies that would otherwise not be considered in a non-SCI patient. The outcome results for mood disorders and depression may also contain overlap since depression is considered to be a mood disorder in the CCHS analysis [19]. Moreover, the CCHS does not include information regarding the treatment that respondents may have been receiving for their health conditions. Because of this, the present analysis did not assess the degree of treatment that respondents were receiving for their SCI, comorbidities, or mental health problems, which would impact the degree of self-perceived mental health outcomes and the reported frequency of mental disorders. Lastly, this study evaluated the population-level odds of suicide and other mental health issues in people with SCI in Canada, which is considered a relatively high-income country. These results may not be globally generalizable as these outcomes and their associated determinants tend to differ between high and low/middle-income countries [30].
Conclusion
There remains a need for research into casual relationships between SCI and mental health, and investigation into the effectiveness of interventions to address mental health in this population. Such studies could offer useful knowledge into the etiology and treatment of mental health disorders following a traumatic injury such as SCI. While this study simply offers a correlative analysis between SCI and mental health, several useful conclusions can be made. This study reveals that, on a population-scale, people with SCI are associated with poorer mental health and increased suicidal thoughts when compared to the general population, even when controlling for lifestyle and socioeconomic factors. Those with SCI also exhibit a unique profile of lifestyle and socioeconomic factors that are associated with these outcomes. Therefore, specific socioeconomic groups within the SCI population, such as those with lower income, fruit and vegetable consumption, and physical activity levels, and higher smoking, may benefit most from targeted interventions. Overall, further research on the mental health of people with SCI has the potential to significantly improve the quality of life of one of the most disadvantaged populations in our modern world.
Data availability
The data that support the findings of this study are available from the corresponding author, AAP, upon reasonable request.
References
Bahm A, Forchuk C. Interlocking oppressions: the effect of a comorbid physical disability on perceived stigma and discrimination among mental health consumers in Canada. Health Soc Care Community. 2009;17:63–70.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77.
Migliorini C, Tonge B, Taleporos G. Spinal cord injury and mental health. Aust N. Z J Psychiatry. 2008;42:309–14.
Post MW, van Leeuwen CM. Psychosocial issues in spinal cord injury: a review. Spinal Cord. 2012;50:382–9.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47:108–14.
Surveillance and Epidemiology Division, Public Health Agency of Canada; CCDSS Mental Illness Working Group; CCDSS Science Committee; CCDSS Technical Working Group. Report summary—mental illness in Canada, 2015. Health Promot Chronic Dis Prev Can. 2015;35:95–6.
McRae L, O’Donnell S, Loukine L, Rancourt N, Pelletier C. Report summary - mood and anxiety disorders in Canada, 2016. Health Promot Chronic Dis Prev Can. 2016;36:314–5.
Navaneelan T. Health at a glance. Suicide rates: an overview. Ottawa: Statistics Canada; 2015. Cat no 82-624-X. www.statcan.gc.ca/pub/82-624-x/2012001/article/11696-eng.htm. Accessed 18 Sep 2021.
Chekroud SR, Gueorguieva R, Zheutlin AB, Paulus M, Krumholz HM, Krystal JH, et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiatry. 2018;5:739–46.
Plurphanswat N, Kaestner R, Rodu B. The effect of smoking on mental health. Am J Health Behav. 2017;41:471–83.
Pearson C, Janz T, Ali J. Mental and substance abuse disorders in Canada. Statistics Canada, Ottawa. https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.htm. Accessed 18 Sep 2021.
McMartin SE, Jacka FN, Colman I. The association between fruit and vegetable consumption and mental health disorders: evidence from five waves of a national survey of Canadians. Prev Med. 2013;56:225–30.
Caron J, Liu A. A descriptive study of the prevalence of psychological distress and mental disorders in the Canadian population: comparison between low-income and non-low-income populations. Chronic Dis Can. 2010;30:84–94.
Chiu M, Amartey A, Wang X, Kurdyak P. Ethnic Differences in mental health status and service utilization: a population-based study in Ontario, Canada. Can J Psychiatry. 2018;63:481–91.
Zürcher C, Tough H, Fekete C. Mental health in individuals with spinal cord injury: the role of socioeconomic conditions and social relationships. PLoS One. 2019;14:e0206069.
Walters JL, Buchholz AC, Martin Ginis KA, SHAPE-SCI Research Group. Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord. 2009;47:318–22.
Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: risk factors and correlates. Arch Phys Med Rehabil. 2004;85:1837–47.
Peterson MD, Kamdar N, Chiodo A, Tate DG. Psychological morbidity and chronic disease among adults with traumatic spinal cord injuries: a longitudinal cohort study of privately insured beneficiaries. Mayo Clin Proc. 2020;95:920–8.
Canadian Community Health Survey (CCHS): Annual Component—2010 Questionnaire [Internet]. Ottawa: Statistics Canada. 406 p. https://www23.statcan.gc.ca/imdb-bmdi/pub/instrument/3226_Q1_V7-eng.pdf. Accessed 18 Sep 2021.
Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil. 2015;96:133–40.
Fann JR, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N, et al. Depression after spinal cord injury: comorbidities, mental health service use, and adequacy of treatment. Arch Phys Med Rehabil. 2011;92:352–60.
Canadian Community Health Survey (CCHS): Annual Component, 2009-2010: Derived Variable (DV) Specifications [Internet]. Ottawa: Statistics Canada. 156 p. Available from: https://www23.statcan.gc.ca/imdb-bmdi/pub/document/3226_D71_T9_V1-eng.pdf. Accessed 18 Sep 2021.
Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology 2012;38:219–26.
Bulloch AG, Fiest KM, Williams JV, Lavorato DH, Berzins SA, Jetté N, et al. Depression—a common disorder across a broad spectrum of neurological conditions: a cross-sectional nationally representative survey. Gen Hosp Psychiatry. 2015;37:507–12.
Phillips AA, Krassioukov AV. Contemporary cardiovascular concerns after spinal cord injury: mechanisms, maladaptations, and management. J Neurotrauma. 2015;32:1927–42.
Squair JW, Dhaliwal R, Cragg JJ, Charbonneau R, Grant C, Phillips AA. National survey of bladder and gastrointestinal dysfunction in people with spinal cord injury. J Neurotrauma. 2019;36:2011–9.
Bilello JF, Davis JW, Cunningham MA, Groom TF, Lemaster D, Sue LP. Cervical spinal cord injury and the need for cardiovascular intervention. Arch Surg. 2003;138:1127–9.
Furlan JC, Fehlings MG. Cardiovascular complications after acute spinal cord injury: pathophysiology, diagnosis, and management. Neurosurg Focus. 2008;25:E13.
Ravensbergen HR, Lear SA, Claydon VE. Waist circumference is the best index for obesity-related cardiovascular disease risk in individuals with spinal cord injury. J Neurotrauma. 2014;31:292–300.
Maselko J. Social epidemiology and global mental health: expanding the evidence from high-income to low- and middle-income countries. Curr Epidemiol Rep. 2017;4:166–73.
Acknowledgements
The Phillips Lab is supported by the Wings for Life Foundation, Compute Canada, Natural Sciences and Engineering Research Council, the Canadian Institutes of Health Research, Alberta Innovates Health Solutions, Brain Canada, Campus Alberta Neuroscience, the Libin Cardiovascular Institute of Alberta, the Hotchkiss Brain Institute, and PRAXIS.
Author information
Authors and Affiliations
Contributions
RDS and JES analyzed the data. RDS, JES, and AAP wrote the first draft of the paper. JES, JWS, and AAP designed, conceptualized, and supervised the study. All authors interpreted the data, revised the manuscript for intellectual content, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sanguinetti, R.D., Soriano, J.E., Squair, J.W. et al. National survey of mental health and suicidal thoughts in people with spinal cord injury. Spinal Cord 60, 444–450 (2022). https://doi.org/10.1038/s41393-022-00783-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00783-0