Abstract
Study design
Retrospective cohort study.
Objectives
The aim of this study was to assess the time to first detection of multidrug-resistant bacteria (MDRB) in urine culture and identify risk factors associated with the first detection of MDRB (1st MDRB).
Setting
Spinal Care Ward and Department of Microbiology, Regional Hospital Liberec a.s., Liberec, Czech Republic.
Method
We cultured urine samples from patients in the acute phase of spinal cord injury or disorder (SCI/D). Multidrug resistance (MDR) was defined as acquired nonsusceptibility to at least one agent from three or more antimicrobial categories. Multivariate logistic regression was used to assess the association of bladder management, broad-spectrum antibiotic exposure, mechanical ventilation, pressure ulcers, positive urine culture on admission, and other risk factors with 1st MDRB. We used only the first urine culture with MDRB for evaluation.
Results
A total of 655 urine cultures from 246 individuals were evaluated, and 829 isolates were obtained. The MDRB prevalence among all isolates was 40.2%. MDRB was detected in 146 (59.3%) patients for the first time, and 76.0% of these isolates were from patients with asymptomatic bacteriuria. The median time to 1st MDRB was 37 days (95% CI, 33–41). According to multivariate logistic regression, 1st MDRB was associated with bladder management with urethral or suprapubic catheterization (OR: 2.8, 95% CI, 1.1–7.2).
Conclusion
The prevalence of infections caused by MDRB was high among the SCI/D population, with three-quarters from patients with asymptomatic bacteriuria. Bladder management with an indwelling catheter is associated with an increased risk of 1st MDRB.
Similar content being viewed by others
Introduction
Urinary tract infection (UTI) is very common in patients with spinal cord injury or disorder (SCI/D). Positivity on urine culture is reported in 50-75% of patients with symptoms [1]. Due to functional impairment of the lower urinary tract, including disturbed urine transport dynamics and frequent placement of intermittent catheterization or indwelling catheters, UTIs are considered complicated. A frequency of 2.5 UTI events per patient per year have been reported [2], and it has been established that UTI is one of the most common complications of SCI/D patients under long-term treatment [3].
Increasing antibiotic resistance, particularly multidrug resistance (MDR), is rapidly becoming a major public healthcare problem worldwide, especially among inpatients. Individuals with previous SCI/D are frequent and recurrent users of healthcare resources and have higher than normal antibiotic exposure, which increases the risk of infection and colonization with multidrug-resistant bacteria (MDRB), especially gram-negative bacteria.
Infection with MDRB is associated with poor outcomes, increased morbidity and mortality, and a prolonged length of hospital stay [4,5,6,7]. The majority of MDRB-related infections are nosocomial infections. There are several risk factors for infection with MDRB: male sex, injury severity, older age, exposure to broad-spectrum antibiotics and bladder management with urethral catheterization (UC) or suprapubic catheterization (SC) [8,9,10,11].
The prevalence of MDRB and its risk factors have been described. However, data on the time of first MDRB detection after SCI/D are lacking, and there is no accurate information on the proportions of symptomatic UTI (S-UTI) and asymptomatic bacteriuria (ABU) cases caused by MDRB.
Therefore, the aim of this study was to assess the time to first MDRB detection (1st MDRB) in urine culture in the SCI/D patient population, analyze risk factors for 1st MDRB and assess S-UTI and ABU case proportions caused by MDRB.
Methods
Study design and population
This was a retrospective cohort study that assessed the time to 1st MDRB after the onset of SCI/D and analyzed risk factors for 1st MDRB. We included patients hospitalized for SCI/D in the Spinal Care Ward from 1 January 2013 to 31 December 2020. The cohort included only patients with acute-phase SCI/D. The coverage area of the Spinal Care Ward includes 0.5 million people. Detailed characteristics of the cohort are shown in Table 1.
Data sources and definitions
Demographic data (age, sex), date of injury, and admission and discharge dates were obtained from electronic medical records (EMRs). Data on antibiotic treatment for UTI, bladder management, and the presence of risk factors were also obtained from EMRs and used to analyze independent variables associated with 1st MDRB.
All urine culture and isolation data were obtained from the electronic database records of the Department of Microbiology. Urine collection was performed at the time of admission, when clinical symptoms of UTI were observed, if UTI was suspected or for routine control purposes.
Urine culture collection was performed according to institutional standards. In patients with spontaneous voiding (SV), we collected 5 mL of midstream urine. For patients with clean intermittent catheterization (CIC), we collected urine from the catheter. In patients with UC or SC, we collected urine after catheter replacement.
Identification of bacterial isolates was performed by colony morphology, Gram staining and matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF-MS)® (Bruker, Daltonics, Germany). A sample with ≥ 103 colony-forming units (CFU)/mL of primary pathogens was considered positive. For antimicrobial susceptibility testing (AST), we used the antibiotic disc diffusion method according to the guidelines and breakpoints of the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [12].
MDR was defined according to the European Centre for Disease Prevention and Control as acquired nonsusceptibility to at least one agent in three or more antimicrobial categories [13]. Based on this definition, we divided bacterial isolates into multidrug-resistant and nonmultidrug-resistant strains.
Only the first culture of MDRB was used for analysis. We considered urine cultures with polymicrobial isolates showing at least one multidrug-resistant strain as multidrug resistant. The analysis evaluated only urine cultures of patients taken at a time when they were not receiving antibiotic treatment.
S-UTI was defined as a positive urine culture with the presence of clinical symptoms of UTI (dysuria, pain or pressure in the lower abdomen, fever or worsening of incontinence) and antibiotic treatment according to AST.
ABU was defined as a positive urine culture without clinical symptoms of UTI and without antibiotic treatment.
We defined healthcare-related risk factors as conditions occurring after or during SCI/D; these included positive urine culture on admission, intensive care unit (ICU) stay, exposure to broad-spectrum antibiotics administered after SCI/D for indications other than UTI, mechanical ventilation, sepsis associated with SCI/D, SCI/D as part of polytrauma, pressure ulcers, and bladder management.
Study endpoints
-
The primary objective was to evaluate the time from SCI/D onset to 1st MDRB in urine culture.
-
The secondary objective was to evaluate risk factors for 1st MDRB and to assess the proportions of symptomatic UTI and ABU caused by MDRB.
Statistical methods
To describe the continuous variables age and time since injury, we calculated the median and its 95% confidence interval (CI) and quartile values due to the nonnormal distributions of both variables (Kolmogorov–Smirnov test, p value = 0.000).
We used univariate logistic regression to determine which independent explanatory variables (predictors) are related to 1st MDRB as the dependent variable. Subsequently, we used multivariate logistic regression to determine which explanatory variables are predictive of 1st MDRB. We present the results as odds ratios (ORs) with 95% CIs. Survival analysis (Kaplan–Meier plots and the results of both log-rank and Breslow tests) was performed to assess the difference in time to 1st MDRB between the two groups of patients. A 5% significance level was applied for all statistical tests. We used SPSS 18 statistical software for statistical analysis. The term ‘significance’ in this study is used to indicate statistical significance.
Results
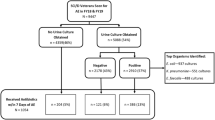
A total of 246 patients with acute-phase SCI/D were evaluated; 829 isolates from 655 positive urine cultures were detected. At the time of admission, 77 (31.3%) patients had a negative urine culture, and 167 (67.9%) patients already had a positive urine culture; results for two patients were unavailable. Of the 829 isolates, 40.2% were MDRB. Of the 655 positive urine cultures, 508 (77.6%) were indicative of ABU and 147 (22.4%) of S-UTI.
1st MDRB occurred in 146 (59.3%) patients: of these, 111 (76.0%) had ABU caused by MDRB, and 35 (24.0%) had S-UTI caused by MDRB. The median time to 1st MDRB was 37 days (95% CI, 33-41). The most common uropathogens at the time of the 1st MDRB were Klebsiella sp., Escherichia coli and Enterococcus faecalis, at 36%, 28% and 12%, respectively.
Based on survival analysis, the median time to 1st MDRB was 35 days (95% CI, 28-42) in the UC or SC bladder management group and 47 days (95% CI, 32–62) in the CIC group. There was a significant difference in the median time to 1st MDRB between the groups (log rank test p-value = 0.012, Breslow test p value = 0.001).
In subanalysis of the ABU group (N = 171), the median time to 1st MDRB was 36 days (95% CI, 30–43). We also observed a significant difference between bladder management with UC or SC and CIC (log rank test p value = 0.014, Breslow test p value = 0.002). Patients with UC or SC experienced colonization with MDRB significantly earlier than those with CIC. The median time to 1st MDRB in the UC or SC group was 31 days (95% CI, 24–38), and that in the CIC group was 51 days (95% CI, 42–60). In the S-UTI subgroup (N = 51), the median time to 1st MDRB was 41 days (95% CI, 33–49). Due to the small number of cases (N = 24) and large proportion of censored cases (67%), data for patients with SV and bladder management with CIC could not be analyzed (Fig. 1).
A Kaplan–Meier plot 1st MDRB for the entire group. A significant difference (log-rank test p-value = 0.012, Breslow test p-value = 0.001) was noted regarding bladder management between the UC or SC and CIC groups. B Analysis of the ABU subgroup. There was also a significant difference regarding bladder management between the UC or SC and CIC groups (log rank test p-value = 0,014, Breslow test p-value = 0,002). C Median time to first S-UTI. It was not possible to analyze CIC and SV bladder management group data due to the small number of cases and large number of censored cases.
We identified risk factors associated with 1st MDRB. Based on univariate logistic regression analysis, ICU stay, use of broad-spectrum antibiotics for indications other than UTI, sepsis, pressure ulcers, sex and bladder management were independent variables with significant relationships with 1st MDRB (Table 2).
We performed multivariate logistic regression using the independent variables included in univariate analysis regardless of whether they had a significant relationship with 1st MDRB (Table 3). Only bladder management with UC or SC was found to be a significant independent predictor of 1st MDRB (OR 2.8, 95% CI, 1.1–7.2, p = 0.038), as determined by the Enter method.
Discussion
The aim of our study was to evaluate the time from onset of SCI/D to 1st MDRB in urine culture and to assess risk factors for 1st MDRB. This is one of the few studies to distinguish between ABU and S-UTI; indeed, recent papers on infection with MDRB in the SCI/D population have not considered this distinction.
In our cohort, the prevalence of MDRB isolates was 40.2%. The cohort exclusively comprised inpatients, with a high proportion of those with indwelling catheters. Comparison of our results with those of others is relatively problematic due to the imprecise definition of MDRB. In our study, we used the current, valid definition of MDR established by the 2011 international expert panel [13]. These guidelines establish epidemiologically significant antibiotic categories for each group of bacteria and define MDR as nonsusceptibility to at least one agent in ≥3 antimicrobial categories. In contrast, most studies conducted before the publication of this consensus statement defined MDR differently; definitions were usually less strict, and accordingly, these studies reported prevalence rates between 22% and 33% [10, 14]. Therefore, comparison with many of these previously published papers is difficult. Fitzpatrick et al. demonstrated an MDRB prevalence of 36.1% among urine isolates, with one-fifth of the cohort being outpatients. The most common uropathogens were E. coli (27%), K. pneumoniae (16%) and Pseudomonas aeruginosa (17.3%), and significant geographic differences in the prevalence of MDRB were also observed [15]. Other studies in the SCI/D population have reported MDRB prevalence rates of 60.7%, 41.36% and 33% [11, 16, 17]. The general trend of an increase in resistant isolates has been found in several studies over the past years [15, 18, 19]. There are also large regional differences in MDRB prevalence and distribution [11, 17].
The median time to 1st MDRB in our cohort was 37 days, and 59.3% of patients harbored MDRB. An almost certain risk of catheter-associated UTI after 28 days of catheterization has been reported [20], and the risk of colonization increases by 3-10% per day when an indwelling catheter is inserted [21]. Nonetheless, results regarding MDRB colonization in the SCI/D population are difficult to compare. Overall, the prevalence of MDRB and other types of resistance varies among hospitals and specialties, and rates are influenced by the patient population, antibiotic policies and established clinical practices. Infection with MDRB increases morbidity and mortality and readmission rates, prolongs the hospital length of stay and has a nonnegligible impact on the cost of treatment [17].
The overall prevalence of ABU in our cohort was high, reaching 77.6%, and the prevalence of ABU in the group with 1st MDRB was 76.0%. The high prevalence of ABU was mainly due to the high proportion of patients with UC or SC. In general, the prevalence of ABU in the SCI/D population varies widely. The overall prevalence of ABU in outpatients with SCI before orthopedic procedures was 30.8% in one study [22]. The prevalence of ABU was 50% in patients with CIC or condom catheters and approached 100% in patients with indwelling catheters. ABU is considered a risk factor for symptomatic UTI [2, 23]. One of the basic measures to prevent the development of MDRB and reduce its prevalence in the SCI/D population is to decrease antibiotic exposure and improve rational antibiotic treatment. Thus, there is consensus that routine antibiotic treatment for ABU is neither necessary nor appropriate [24].
In our cohort, the most common strains were Klebsiella sp. (36%), E. coli (28%) and E. faecalis (12%). Most similar studies report E. coli as the dominant uropathogen in the SCI/D population, with a significantly lower proportion of Klebsiella sp. [11, 15, 25]. One possible reason for the high prevalence of Klebsiella sp. strains in our cohort is the relatively high proportion of patients with indwelling catheters owing to the acute nature of hospitalization in the Spinal Cord Ward. Most patients in the ward had been hospitalized since their injury, and the mean length of stay was 77 days. In contrast with other studies, we did not detect multidrug-resistant Staphylococcus aureus (MRSA) strains in this study [5, 26], and there is a clear trend in the shift from MDR gram-positive cocci to MDR gram-negative bacteria [5].
In the cohort, 19.9% of the patients had polytrauma, 27.2% required mechanical ventilation, 74.0% were admitted to the ICU after an SCI/D event, 10.6% had sepsis, and 10.2% had pressure ulcers. The results of univariate analysis showed ICU stay, use of broad-spectrum antibiotics, sepsis, pressure ulcers, sex, and bladder management with UC or SC to be significant risk factors for 1st MDRB. However, multivariate analysis revealed only one independent predictor, namely, bladder management with UC or SC, which increased the odds of 1st MDRB (OR 2.8, 95% CI 1.1–7.2, p = 0.038) compared with the reference category of SV. Inclusion of the other independent variables did not improve the prediction of 1st MDRB, as there were relationships among the independent variables evaluated in the multivariate analysis. Based on the chi-square test, Cramer’s V and the adjusted residuals, there was a relationship between bladder management and positive urine culture at admission, ICU admission, exposure to broad-spectrum antibiotics, sepsis, polytrauma, and pressure ulcers; Cramer’s V coefficients were 0.25, 0.23, 0.28, 0.19, 0.16 and 0.19, respectively. Furthermore, we detected a relationship between ICU admission and positive urine culture, exposure to broad-spectrum antibiotics, mechanical ventilation, sepsis, polytrauma and sex, with Cramer’s V coefficients of 0.26, 0.39, 0.36, 0.20, 0.25 and 0.15, respectively. Long-term bladder management with UC or SC was a major risk factor for 1st MDRB according to multivariate logistic regression, whereas the influence of the other included predictors decreased.
We speculate that frequent and long-term use of UC or SC is one of the main reasons for the high prevalence of MDRB and the high incidence of nosocomial Klebsiella sp. strains. It is well established that the method of voiding can affect bacterial strains in urine [27]. One of the basic measures for the prevention of MDR should be early catheter removal, and the prophylactic effect of CIC is well known [28]. Another reason may be the frequent use of broad-spectrum antibiotics for indications other than UTI, which also leads to selection of resistant strains. Other studies have reported comparable results [8,9,10, 29]. Bladder stones are also a possible cause of MDRB, though there were no bladder stones in our cohort of acute SCI/D patients.
The definition of significant bacteriuria in the SCI/D population is not uniform. In our study, we used the presence of 103 CFU/mL as the definition of symptomatic bacteriuria. A number of studies have defined significant bacteriuria as ≥103 CFU/mL [30], ≥104 CFU/mL [31] or ≥105 CFU/mL [32, 33]. The use of specific cutoffs for determining significant bacteriuria is usually based on the presumption of urinary sterility. The inconsistency in the definition of significant bacteriuria and the atypical symptoms of UTI in the SCI/D population lead to diagnostic confusion associated with antibiotic overuse, which is one of the reasons for the increasing prevalence of MDRB.
Our study is limited by a number of factors. First, it was a retrospective study from a single center. Although the dataset was quite large, the results need to be validated in a multicenter study. Second, analysis was difficult because there are no criteria for UTI in the SCI/D population; moreover, symptoms of UTI are often not present due to neurological impairment. Third, the results of the study may be modified by other factors, such as regional trends, established clinical practices or local antibiotic policies.
In summary, there was a high prevalence of infection caused by MDRB in our cohort of inpatients with acute-phase SCI/D. The median time to first detection of urogenital tract colonization with MDRB was 37 days (95% CI, 33–41), and three-quarters of cases were patients with asymptomatic bacteriuria. Bladder management with UC or SC was associated with an increased risk and odds of 1st MDRB (OR 2.8) compared with SV. The results of this study emphasize the importance of consistent bladder management; indwelling catheter insertion should be limited to the necessary time, and the early and widespread use of CIC should be considered.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Penders J, Huylenbroeck AA, Everaert K, Van Laere M, Verschraegen. GL. Urinary infections in patients with spinal cord injury. Spinal Cord. 2003;41:549–52.
Esclarin De Ruz A, Garcia Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000;164:1285–9.
Adriaansen JJ, Ruijs LE, van Koppenhagen CF, van Asbeck FW, Snoek GJ, et al. Secondary health conditions and quality of life in persons living with spinal cord injury for at least ten years. J Rehabil Med. 2016;48:853–60.
Rabadi MH, Aston CE. Predictors of mortality in veterans with multiple sclerosis in an outpatient clinic setting. Int J MS Care. 2017;19:265–73.
Waites KB, Canupp KC, Chen Y, DeVivo MJ, Moser SA. Bacteremia after spinal cord injury in initial versus subsequent hospitalizations. J Spinal Cord Med. 2001;24:96–100.
Hsiao CY, Yang HY, Chang CH, Lin HL, Wu CY, et al. Risk factors for development of septic shock in patients with urinary tract infection. Biomed Res Int. 2015;2015:717094.
Welk B, Fuller A, Razvi H, Denstedt J. Renal stone disease in spinal-cord-injured patients. J Endourol. 2012;26:954–9.
Toner L, Papa N, Aliyu SH, Dev H, Lawrentschuk N, et al. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in hospital urinary tract infections: incidence and antibiotic susceptibility profile over 9 years. World J Urol. 2016;34:1031–7.
Ryu KH, Kim YB, Yang SO, Lee JK, Jung TY. Results of urine culture and antimicrobial sensitivity tests according to the voiding method over 10 years in patients with spinal cord injury. Korean J Urol. 2011;52:345–9.
Waites KB, Chen Y, DeVivo MJ, Canupp KC, Moser SA. Antimicrobial resistance in gram-negative bacteria isolated from the urinary tract in community-residing persons with spinal cord injury. Arch Phys Med Rehabil. 2000;81:764–9.
Evans CT, Fitzpatrick MA, Jones MM, Burns SP, Poggensee L, et al. Prevalence and factors associated with multidrug-resistant gram-negative organisms in patients with spinal cord injury. Infect Control Hosp Epidemiol. 2017;38:1464–71.
(EU-CAST), E.C.o.A.S.t. Clinical breakpoints - breakpoints and guidance. 2020 2.11.2020; Available from: https://www.eucast.org/ast_of_bacteria/.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Mylotte JM, Kahler L, Graham R, Young L, Goodnough S. Prospective surveillance for antibiotic-resistant organisms in patients with spinal cord injury admitted to an acute rehabilitation unit. Am J Infect Control. 2000;28:291–7.
Fitzpatrick MA, Suda KJ, Safdar N, Burns SP, Jones MM, et al. Changes in bacterial epidemiology and antibiotic resistance among veterans with spinal cord injury/disorder over the past 9 years. J Spinal Cord Med. 2018;41:199–207.
Suda KJ, Patel UC, Sabzwari R, Cao L, Ramanathan S, et al. Bacterial susceptibility patterns in patients with spinal cord injury and disorder (SCI/D): An opportunity for customized stewardship tools. Spinal Cord. 2016;54:1001–9.
Ramanathan S, Fitzpatrick MA, Suda KJ, Burns SP, Jones MM, et al. Multidrug-resistant gram-negative organisms and association with 1-year mortality, readmission, and length of stay in Veterans with spinal cord injuries and disorders. Spinal Cord. 2020;58:596–608.
Forster CS, Courter J, Jackson EC, Mortensen JE, Haslam DB. Frequency of multidrug-resistant organisms cultured from urine of children undergoing clean intermittent catheterization. J Pediatr Infect Dis Soc. 2017;6:332–8.
Fan NC, Chen HH, Chen CL, Ou LS, Lin TY, et al. Rise of community-onset urinary tract infection caused by extended-spectrum β-lactamase-producing Escherichia coli in children. J Microbiol Immunol Infect. 2014;47:399–405.
Mota ÉC, Oliveira AC. Catheter-associated urinary tract infection: Why do not we control this adverse event? Rev Esc Enferm USP. 2019;53:e03452.
Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146:719–23.
Fitzpatrick MA, Suda KJ, Burns SP, Poggensee L, Ramanathan S, et al. Pre-operative screening for asymptomatic bacteriuria and associations with post-operative outcomes in patients with spinal cord injury. J Spinal Cord Med. 2019;42:255–9.
Afsar SI, Yemisci OU, Cosar SN, Cetin N. Compliance with clean intermittent catheterization in spinal cord injury patients: a long-term follow-up study. Spinal Cord. 2013;51:645–9.
Cardenas DD, Hooton TM. Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76:272–80.
Mortazavi-Tabatabaei SAR, Ghaderkhani J, Nazari A, Sayehmiri K, Sayehmiri F, et al. Pattern of antibacterial resistance in urinary tract infections: A systematic review and meta-analysis. Int J Prev Med. 2019;10:169.
Girard R, Mazoyer MA, Plauchu MM, Rode G. High prevalence of nosocomial infections in rehabilitation units accounted for by urinary tract infections in patients with spinal cord injury. J Hosp Infect. 2006;62:473–9.
Trautner BW, Darouiche RO. Prevention of urinary tract infection in patients with spinal cord injury. J Spinal Cord Med. 2002;25:277–83.
Wyndaele JJ, Brauner A, Geerlings SE, Bela K, Peter T, et al. Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int. 2012;110:E910–7.
Kang MS, Lee BS, Lee HJ, Hwang SW, Han ZA. Prevalence of and risk factors for multidrug-resistant bacteria in urine cultures of spinal cord injury patients. Ann Rehabil Med. 2015;39:686–95.
Wyndaele JJ. The encrustation and blockage of longterm indwelling catheters. Spinal Cord. 2010;48:783.
Dedeić-Ljubović A, Hukić M. Catheter-related urinary tract infection in patients suffering from spinal cord injuries. Bosn J Basic Med Sci. 2009;9:2–9.
Faarvang KL, Müller P, Lomberg B, Biering-Sørensen F. Screening for bacteriuria in patients with spinal cord lesion: Dipstick test, microscopic examination and urine culture. Spinal Cord. 2000;38:106–8.
García Leoni ME, Esclarín De Ruz A. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect. 2003;9:780–5.
Acknowledgements
The authors would like to thank Hana Kolářová, Ph.D. for assistance with data processing and statistical evaluation.
Funding
This work was supported by funding from the Scientific Board of Krajská nemocnice Liberec, a.s.
Author information
Authors and Affiliations
Contributions
Study concept and design: VŠ, VP. Data analysis and interpretation: VŠ, HK. Microbiology expertise: DF. Manuscript preparation: VŠ, VP. Manuscript review: VŠ, JM. All authors read and approved the final manuscript. All authors consent to the publication of the manuscript in Spinal Cord.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the relevant Institutional Review Boards. We certify that all applicable institutional and governmental regulations concerning the ethical use of human subjects data were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Šámal, V., Paldus, V., Fáčková, D. et al. Multidrug-resistant bacteria in urine culture among patients with spinal cord injury and disorder: Time to first detection and analysis of risk factors. Spinal Cord 60, 733–738 (2022). https://doi.org/10.1038/s41393-022-00774-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00774-1
This article is cited by
-
Indwelling catheter vs intermittent catheterization: is there a difference in UTI susceptibility?
BMC Infectious Diseases (2023)