Abstract
Study design
Development and validation of fracture classification system.
Objective
To develop and validate a Simplified Classification System (SCS) for Thoraco-Lumbar (TL) fractures (SCS – TL fractures).
Setting
Tertiary Spinal Injuries Centre, New Delhi, India
Methods
Based on the International Spinal Cord Society Spine Trauma Study Group (ISCoS STSG, n = 23) experts’ clinical consensus conducted by the senior author and on his own experience, the Denis classification for TL fractures was modified to develop a SCS-TL fractures that could guide the management. After Face and Content validation, Construct validation was done in two stages. First stage analyzed if management of 30 cases of TL fractures, as suggested by the SCS - TL fractures and ISCoS STSG (n = 9) as well as other (n = 5) experts, matched. Second stage was a one year prospective study analyzing if the management suggested matched the management actually carried out by different spine surgeons (n = 10) working at a single institution.
Results
In the first stage there was 100% agreement for management (conservative or surgical) as proposed by experts and that suggested by the proposed classification for TL fractures whereas for surgical approach there was 88% agreement. In the second stage, there was 100% agreement for the management as well as surgical approach as carried out at our centre and that proposed by the SCS for TL fractures.
Conclusions
The proposed SCS-TL fractures helps in classifying and in decision making for management of TL fractures. The next phase of validation would involve multicentric reliability studies and prospective application of the SCS- TL fractures.
Similar content being viewed by others
Introduction
Numerous variables like morphology of the fracture, injury mechanism, anatomical factors responsible for fracture stability and neurology of the patient secondary to the injury have been used to propose classification systems intended to describe thoracolumbar spine injuries. But the quest for an ideal classification system is yet to be fulfilled. Initial classifications had been based on injury’s mechanism or morphology as understood from plain radiographs or CT, ignoring the ligamentous contribution to the fracture stability and failing to consider underlying neurologic involvement. Others have been complex and difficult to use in the daily practice. Each of them contends to be better than the earlier ones but subsequent studies have outlined their limitations [1, 2].
An ideal classification system for spinal injuries, as described by Middendorp et al., should be able to characterize all the clinically significant injuries with minimum subcategories and in an alfa numeric coding. It should include prognostic factors and have a high inter observer reliability when used by both experienced and inexperienced physicians [3].
Even though there exist numerous classification systems for thoraco-lumbar spine injuries only some of them have been validated systemically. Mechanistic classifications proposed by Boehler and Allen –Ferguson did not gain enough acceptance [4, 5]. Later the three column concept proposed by Denis, though not systemically validated, got huge acceptance and has been commonly used due to its simplicity. However, it doesn’t account for all morphological patterns of TL fractures, doesn’t consider the neurological status due to the injury of the patient and also doesn’t guide the fracture management. Later Mc Afee [6] classified thoracolumbar fractures based on mechanism and morphology without considering neurology and fracture stability in to consideration. The AO-Magerl (ArbeitsgemeinschaftfürOsteosynthesefragen) classification was more inclusive since it recognized a wider pattern of fractures including 55 subtypes using the 3-3-3 AO principle. However the resultant complexity limited its usage in daily practice [7]. Moreover, it also does not consider the neurological status due to the injury, a critical determinant for surgical decision making [8]. This AO-Magerl system was later modified by reducing the number of subcategories, but the classification still didn’t consider neurology and modifiers. This was again remodified recently in to the latest classification, reducing the number of fracture morphological subcategories further and introducing neurology and modifiers. However it is still under validation and the way this new system guides the management has not yet been published [9, 10].
As per one survey involving the Spine Trauma Study Group of ISCoS and other international spine experts, the existing spine trauma classification systems lacked the required objectives for an ideal system. The survey revealed that the Thoracolumbar Injury Classification and Severity Score (TLICS) was more often used (47.50%, n = 19). The experts’ response for practical implementability in daily practice was more uniformly distributed among TLICS, AO and Denis classifications (31%, 23% and 37.5%, respectively). The experts, however, felt that the existing classification systems did not account for all the desired objectives and the reliability for residents was a prime concern [11].
Realizing the need of simple classification systems for thoracolumbar spine which could easily be used by the ordinary physician, effectively characterize the injuries which are clinically relevant and guide treatment, we proposed a new classification system. The purpose of this article is to introduce this new classification system as well as the practical treatment strategy which it proposes and describe its validation.
Materials and methods
The study for development and validation of the classification system was conducted in various steps which have been outlined below.
Various experts other than the authors, as mentioned under the acknowledgement head of the manuscript subsequently, were involved in the various steps of the study. Only experts who had an established practice which was exclusively or substantially spine were involved in the study. This was established through questions incorporated in the survey.
Identification of the deficiencies in the existing classification systems and the need for a new classification system for TL fractures
The senior author had conducted a survey amongst the ISCoS STSG as well as other spine experts globally. The deficiencies in the existing classification systems for TL fractures and the need of an ideal classification system for TL fractures was identified [11].
Development of the classification system
The survey above had suggested that practical implementability in daily practice is the most expedient feature of any such new classification system and the Denis System scored the most in this regard though it had limitations.
Based on experts’ (ISCoS STSG, n = 23) clinical consensus conducted by the senior author and his own experience, the Denis classification system was modified to increase its comprehensiveness. Other parameters influencing management, as per the opinion of experts in the survey, were integrated in the modified classification system. Another study was carried out by the senior author to formulate clinical consensus management algorithms (under publication). On issues where there was low agreement (<70%), the process of Delphi consensus was used. This was used for outlining the treatment plan for each category.
Validation of the new simplified classification system
The methods devised by Audige et al. to validate a classification system were followed for this step of the study [12].
Face and content validity of the new simplified classification system was done by circulation and discussion through email amongst the members of the ISCoS STSG (n = 7) and other experts (n = 5) and incorporation of the relevant suggested changes.
After approval from Institutional Ethics committee, construct validation of the classification was then carried out in two stages [12].
The first stage involved sending through survey monkey to 23 renowned spine surgeons of ISCoS STSG, anonymized and delinked clinic-radiological data (including relevant X-ray, CT scan, MRI and information regarding age, mode of injury, neurology and presence of any modifiers) of 30 case studies of TL fractures along with the questionnaire related to the management. Reviewers were requested to opine regarding their management strategy for each case. The management suggested by the new classification was then analyzed and compared with the management as had been suggested by the 14 experts who responded to the survey.
The second part of the study involved evaluating prospectively, the cases of TL fractures presenting to Indian Spinal Injuries Centre over one year and analyzing how similar was the management as proposed by the new classification system as compared to the management actually followed by 10 different consultant spine surgeons of the same Centre.
Statistical analysis
The simplest tool or percentage agreement was used as a test to measure inter rater reliability or consistency.
Results
-
1.
The components of the Simplified Classification System (SCS- TL fractures).
The four key components of the SCS- TL fractures include:
-
a.
Injury Morphology as determined by the plain radiographs with or without CT and/or MRI.
-
b.
Injury Stability (indicating the severity of bony and ligamentous injury).
-
c.
Neurological status of the patient.
-
d.
Modifiers.
-
a.
Morphological categories (modification of the Denis classification [13]).
Thoracolumbar Fractures (T1 – L2).
-
Compression
-
Burst
-
Chance
-
Fracture dislocation
-
Isolated spinous process/transverse process/pars/ facet fractures.
-
Others:
-
Hyperextension injury
-
Mixed morphological injury (Chance fracture with a burst component or Fracture dislocation with a burst component)
-
The first five morphological categories are as described in the original classification system proposed by Denis. The new categories added in order to make the categories comprehensive are as follows:
Hyperextension injury
These are unique fractures representing < 3% of fractures. The entire spine fails due to tensile force. The fracture line begins from the anterior aspect of the vertebra/disc and travels posteriorly. They are commonly seen in ankylosed spine (ankylosing spondylitis/diffuse idiopathic skeletal hyperostosis). The fractures can involve all three columns. The fracture plane is variable. Imaging findings can range from subtle findings of widening of the intervertebral disc space or distraction of the vertebral body fragments to dislocation with translation in sagittal plane [14] (Fig. 1).
Mixed morphological injury
Chance fractures or fracture dislocations can sometimes be associated with a burst component or a compression fracture. These will be considered under mixed morphological injuries (Fig. 2).
-
b.
Injury stability
a AP plain radiograph, b Lateral plain radiograph, c MRI mid sagittal showing fracture at the level of T6-T7 vertebrae, d CT mid sagittal cut showing the burst component at the level of T6-T7 vertebrae, black marker indicating involvement of posterior column, e Axial cut showing retropulsed fragment causing canal compromise.
TL fractures are classified according to stability as under:
-
STABLE: S
-
UNSTABLE: US
Parameters considered in judging fracture stability (indicating the severity of bony and ligamentous injury) are as under:
-
All fractures with neurological deficit are generally considered to be unstable.
-
Fracture dislocations, Chance fractures and Hyperextension injuries are considered to be unstable irrespective of the neurological status.
-
PLC disruption is considered to result in instability in compression and burst fractures. It is assessed by MRI and also be plain radiographs. The features of instability in neutral or dynamic X-rays include [15]:
-
Loss of more than or equal to 50% of vertebral height.
-
>/= 30 degrees of kyphosis.
-
Inter-spinous widening.
Stable injuries, as assessed by MRI and also on static radiographs by above criteria, could be confirmed with dynamic X rays. Dynamic X rays are done under supervision with adequate pain relief in patients with no neurological deficit and with compression or burst fractures with no defined parameters of instability on static radiographs.
-
c.
Neurological status of the patient
All SACI are classified with respect to neurology according to ISNCSCI [16] as under:
-
No neurological deficit: N0
-
Incomplete neurological deficit (AIS B, C, D, Incomplete cauda equina): N1
-
Complete neurological deficit (AIS A, complete cauda equina): N2
-
d.
Modifiers
Modifiers play a key role in planning the surgical procedure like the need for a staged procedure in polytrauma with ISS > 15, a long segment fixation in ankylosing disorders or the use of cement augmentation for instrumentation in osteoporosis. The modifiers of the SACI management are as under:
M0 – no modifier
M1 – polytrauma
M2 – ankylosing disorders
M3 – > 75 years
M4 – Osteoporosis
M5 – Poor general condition
M6 – Contiguous vertebral injuries
-
2.
Procedure of classifying the TL fractures using SCS- TL fractures.
The five steps of classifying any TL fracture as per the SCS- TL fractures (Flowchart 1-Appendix I) include:
-
a.
Identification of the Spinal segments involved in the injury.
-
b.
Assessment of the neurological picture of the patient secondary to the injury: if there is neurological involvement the injury is considered unstable and surgery is indicated. Chance fractures, Hyperextension injuries and Fracture- dislocations are considered unstable irrespective of the neurological status.
-
c.
Establishment of the injury morphology based on the radiographs with or without CT and/or MRI.
-
d.
Analyzing the stability of the injury - If the morphology is suggestive of a burst or compression fracture, the neurology is intact and there is no instability on static radiographs as per the criteria mentioned before, dynamic radiographs are performed under supervision after obtaining adequate pain relief. However, if MRI is available, the stability can be assessed by the intactness of posterior ligamentous complex (especially supraspinous ligament intactness on T2 MRI) [17].
-
e.
Identifying the presence of any modifiers that may alter the treatment strategy.
-
3.
Deciding the treatment plan using SCS- TL fractures.
Approaches for management of TL fractures are described below (also depicted in Table 1):
Compression fractures
-
C N0 S: Conservative (Fig. 3) (However, surgical management is indicated if there is an
Fig. 3: Plain radiographs showing compression fractures of L1 vertebrae. unacceptable increase of kyphosis on follow-up).
-
C N0/N1/N2 US: posterior stabilization.
Burst fractures
-
B N0 S: Conservative (However, surgical management is indicated if there is an un acceptable increase of kyphosis on follow-up).
-
B N0 US: Posterior/ Anterior stabilization or Conservative.
-
B N1 US: Posterior/Anterior stabilization + /− decompression (Fig. 4).
Fig. 4: Plain radiographs preoperative and postoperative images of Burst L2 fracture. a Plain AP image showing fracture L2 vertebrae. b Plain Lateral image showing fractured unstable L2 vertebrae. c Plain postoperative AP image. The fracture was managed with indirect decompression and short segment posterior stabilization with intermediate screws in fractured L2 vertebrae. d Plain post-operative Lateral image. Lordosis with indirect decompression is achieved with short segment instrumentation.
-
B N2 US: Posterior/Anterior stabilization
-
Anterior augmentation is to be decided by McCormack-Gaines load-sharing classification [18].
Chance injuries (CH NO/NI/N2 US)
-
Through the disc – posterior/anterior stabilization.
-
Through the vertebra – posterior stabilization or conservative management with bed rest for 6 weeks (however, percutaneous or open posterior stabilization is indicated if there is a loss of reduction or increase in kyphosis on follow up) (Fig. 5).
Fig. 5: Plain radiographs Preoperative and postoperative and CT of a L2 transosseous chance fracture. a Plain AP image showing fracture at L2 vertebrae with increased interpedicular distance. b Plain lateral image showing burst fracture in L2 vertebrae. c Mid sagittal cut showing transosseous chance fracture involving all the three columns. d Plain AP postoperative image showing short segment posterior stabilization with a transverse connector with intermediate screw on the right side in L2 vertebrae, e Postoperative lateral image showing lordosis in fractured segment.
-
Combined bony as well as ligamentous chance with normal alignment – option of posterior stabilization or conservative management.
Fracture dislocations (FD N0/N1/N2 US)
All fracture dislocations are unstable and need posterior reduction, short segment (one level above and one level below with screw in fractured vertebra) stabilization if there is good hold of all the screws, else long segment stabilization (more than one level above and below the fractured vertebra) & fusion; if significant anterior column deficiency consider anterior reconstruction using McCormack-Gaines load-sharing classification (Fig. 6).
a Plain AP image with the marker showing discontinuity at T11-T12 levels in an ankylosed spine. b Lateral plain image with the marker showing fractured ossification at T11-T12 levels in an ankylosed spine. c Mid sagittal CT image with the marker showing opening up of disc space at T11-T12 levels (hyper-extension injury), d Postoperative plain AP image. The fracture was managed by posterior reduction and stabilization (T10-L1). e Postoperative plain lateral image.
Hyperextension injury (HE N0/N1/N2 US)
Posterior stabilization + /− anterior fusion, if there is a significant anterior void (Fig. 7).
Mixed morphological injury
Treatment is decided by the most unstable injury, however, other morphology has a bearing on treatment. For e.g., in a fracture dislocation with a burst component, treatment is decided by fracture dislocation but anterior augmentation may be required if Gaines score ≥ 7 (Fig. 8).
a Plain AP preoperative image showing fracture T6-T7 levels. b Plain lateral image showing fractured T6-T7 level. c Mid sagittal MRI showing burst fracture involving all the three columns with cord compression. d Mid sagittal CT showing mixed pattern of injury, chance fracture is associated with burst component of T6. e Axial CT image with marker showing retropulsed fragment causing canal compromise with burst vertebral body. f Postoperative plain AP image. The fracture was managed by posterior stabilization with intermediate screws. g Postoperative lateral image.
Others (spinous process and transverse process fractures)
They are inherently stable injuries and managed conservatively.
-
4.
Validation
Face and content validity
This was done through circulation by email amongst members of ISCoS Spine Trauma Study Group (n = 7) and other experts (n = 5).
Construct validation
First stage
A total of 30 case scenarios of thoracolumbar spine fractures used for this stage consisted of 9 burst fractures, 8 fracture dislocations, 7 chance injuries and 6 compression fractures.
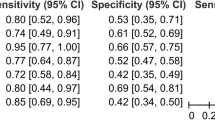
On analysis of treatment recommendations, in the first stage there was 100% agreement for management (conservative or surgical) as proposed by experts and that suggested by the proposed classification for TL fractures whereas for surgical approachthere was 88% agreement.
The subcategory wise agreement with regard to surgical approach was as under:
Burst fractures: 76%
Chance injuries: 85%
Compression fractures: 93%
Fracture dislocations: 98%
Second stage
95 thoracolumbar spine fracture cases reported to our centre (ISIC) in the study period. The details of patient demographics, neurology and subtype of fracture as per the proposed classification has been enclosed as Table 2. The subcategory wise break up was as under:
Fracture dislocation - 29
Burst - 32
Compression - 4
Chance injuries - 24
Mixed morphology - 2
Hyperextension - 4
Management and surgical approach of all cases (100%) as performed was similar to the management prescribed by the proposed classification.
Discussion
The SCS- TL fractures is an attempt at a new simple classification system for thoracolumbar spine injuries which could easily be used by the ordinary physician, effectively characterize the injuries which are clinically relevant and guide treatment. The need for such a classification had been brought out by a survey on classification systems conducted by the senior author in 2013 involving 42 experts, 16 of Spine Trauma Study Group of ISCoS and 26 others [11]. The survey revealed that as per the majority of the global spine experts (71%), practical implementability in the daily practice is the most expedient feature of any such new classification system as one of the commonest uses of the classification systems may be for the junior residents/fellows to liase with the consultant about the spine injury type of the patient presenting to the emergency department. This could explain the re-shifting of the experts to the usage of the traditional classification systems. This rethink had emphasized the usefulness of the traditional systems and thus we have explored the option of suitably modifying traditional classification systems to develop a newer classification system.
Treatment guidance, modifiers, reliability and comprehensiveness are the other important features to be considered while designing a new classification system [11]. Thus we started deliberating on which traditional classification system would be most suitable for modification to develop a new classification system.
Even though the initial AO-Magerl thoracolumbar injury classification system identifies a wide pattern of fractures, including > 50 subtypes, its complexity has yielded a poor inter and intra observer agreement [7, 19]. Moreover, the AO-Magerl system does not consider the patient’s neurologic status, a critical determinant of surgical decision making [20]. Later it was modified reducing the subcategories in describing fracture morphology but it still did not include neurology and also didn’t guide management [10]. Recently the AO system was further re-modified reducing the number of subcategories further and adding neurology and modifiers to the classification system. Though this new AO system claims to overcome its previous limitations, this system is under validation [9, 21]. For thoraco-lumbar fractures even the validatedclassification of Thoracolumbar Injury Classification and Severity score (TLICS) has its limitations. There are only few studies by experts who were not a part of its development and most of the published data is not of sound scientific evidence (i.e., retrospective studies) [22]. Though reliability (as compared to AO as well as Denis classifications) and prospective application of TLICS has been done, a direct collation with other classification systems is required to elucidate the efficacy of the TLICS [19, 23]. Moreover, certain injury patterns are difficult to classify and score using TLICS and the reproducibility and feasibility of evaluating posterior ligamentous complex (PLC) integrity utilizing MRI has also been challenged [24, 25].
The Denis classification for thoracolumbar spine injuries is not comprehensive enough to consider all fracture types, doesn’t provide prognostic information and does not consider neurological status of the patient secondary to the injury and thus doesn’t adequately guide TL fracture decision making. The native idea of instability has been over-deciphered to state that it exists if two of the three columns are damaged, thus requiring surgical stabilization in such cases. On the contrary, few studies have depicted that non-surgical management of two column injuries may achieve an acceptable outcome [26]. However in the survey done by the senior author, this classification system had a good acceptance and experts felt that it is comfortably reproduced due of its simplicity [11]. It was felt to be the most practically implementable in daily practice. This was the most desirable feature of an ideal classification system as per the experts in the survey [11]. Hence we decided to modify the Denis classification.
The Denis classification tends to describe the morphologic characteristics of the injury and no attempt had been made to define the parameters of stability and neurologic involvement. Neurologic deterioration following vertebral fracture is in itself an indicator of instability. In the proposed classification, the authors have made the classification system comprehensive by adding 2 more morphological categories, emphasized on the neurology, defined the parameters of stability and incorporated modifiers.
For classifying and managing the TL fractures as per SCS- TL fractures, ideally plain radiographs as well as MRI and/or CT are recommended in all cases. However, plain radiographs may be sufficient in classifying the TL fractures using SCS- TL fractures in a majority of cases. In situations when the radiographic quality is poor to visualize the injured spinal segments (upper thoracic and junctional regions), MRI/CT is required for classification and deciding the management. CT is also required for cases with burst component to decide on the need for an anterior augmentation procedure if a short segment stabilization is planned [18].
Modifiers have been introduced in the proposed classification as they are known to influence decision making for management. In burst fractures with polytrauma or in patients with poor general condition, the decision to augment the anterior column can be staged [27]. Ankylosing disorders are predisposed to a different injury type and often require special considerations. Because of concentration of forces at the fracture site and reduced bone mineral density, either long posterior or circumferential fixation with or without cement augmentation is recommended [28,29,30]. In old age, co morbidities or poor general condition may warrant staged surgeries. Osteoporotic compression fractures which are apparently stable on neutral radiographs might be unstable as evident from dynamic X rays [31]. Fixation must be strong enough to withstand substantial loading in the setting of preexisting osteoporosis. This can be achieved by better triangulation of screws, increased points of fixation by longer constructs, circumferential fixation, use of other instrumentation devices like sub laminar wires, pedicle or transverse process hooks and/ or use of more crosslinks. Apart from that, use of hydroxyapatite screws and cement augmentation has also gained popularity [32, 33]. Presence of contiguous fractures may alter the surgical plan depending on the specific case scenario.
In the first stage of validation of our study, there was 100% and 88% agreement between the experts and the proposed classification for recommendation of management as well as surgical approach respectively. A substantial component of the 12% disagreement in surgical approach recommendation was that of management of burst fractures. This could be due to the differences in opinion with regard to the requirement for anterior column augmentation as some experts favored no augmentation even when the McCormack Gaines score was higher than 7. This is supported by literature as some recent studies have questioned the need of anterior augmentation in such cases [34, 35]. In the absence of a clear cut directive from evidence the decision to augment or not is left on the surgeon in consultation with the patient. The agreement between experts and the classification system for the treatment recommendation could not be compared with other existing classification systems. This has not been discussed for TLICS and the AO Thoraco lumbar injury classification by the authors in their original reports [19, 22].
Patient’s neurological status is crucial for an overall assessment of the patient’s functional status and the final prognosis [22]. It has been found out to be one of the most crucial factors in surgical decision making [22]. The SCS- TL fractures also highlighted the importance of considering the patient’s neurology in making the recommendation for treatment. This has also been highlighted in other classification systems like TLICS where neurology is an integral part of the classification that guides the management [22]. Given its critical importance, the neurological modifier is an important component of this classification proposal and guides the need for operative intervention.
The fact that the classification can be done with x-rays in the majority of cases is another strength of the classification system. Most patients in emerging countries don’t have access to or can’t afford a CT/MRI. The value added by these investigations especially in some special considerations can’t be questioned, but the affordability and accessibility of the masses needs to be also considered. Since the reproducibility of evaluating posterior ligamentous complex (PLC) integrity using MRI and the affordability/accessibility of MRI in emerging nations has been questioned, we relied on neutral and dynamic plain radiograph features to confirm stability for compression as well burst fractures [36, 37]. The dynamic radiographs need to be performed under medical supervision after obtaining adequate pain relief to overcome the muscle spasm associated with acute trauma [38]. If adequate motion is not reproduced on dynamic radiographs of TL spine, the stability of the fracture could be evaluated by MRI. MRI/CT is mandatory for classifying as per this classification system only in limited special conditions. Even though MRI is done ideally to evaluate all patients with neurological deficit, it is not mandatory for classification and thereby for deciding management, except in special conditions. The simplified classification can thus not only effectively help in classifying the TL fractures but also guide clinical decisions in their management in all scenarios including the resource constrained patients in the developing countries.
Limitations of the study include the relatively small number of cases in the survey. The classification system can be done just with plain radiographs in the huge majority of resource constraint cases who can’t afford/don’t have access to MRI/CT, but a criticism could be that pure ligamentous injuries are likely to be missed. These patients would not have got an MRI done anyway and the classification system provides an option of classifying their injuries irrespectively by specifying dynamic X rays for suspected unstable injuries. Another limitation is that if adequate movement of the involved spine cannot be obtained on dynamic radiographs even after adequate analgesia, one has to depend on MRI to rule out ligamentous injury. However, where available and affordable, a MRI is advocated by the system. The classification system, however, needs further validation. A study is being conducted on prospective application of the classification system to all patients of thoracolumbar fractures managed by senior author. This and reliability studies including clinicians in different settings as well as with diverse experience are necessary to complete the process of validation.
Conclusions
The proposed classification system for TL fractures is simple, thus increasing the likelihood of practical implementation in day-to-day clinical practice with good reliability and minimal variability irrespective of physician experience. It should effectively help in comprehensively classifying the thoracolumbar spinal injuries. Since it accounts for neurological status as well as fracture stability and incorporates other modifiers influencing treatment it should effectively guide clinical decision making for management, even in resource constrained population in the emerging countries.
Data archiving
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Mirza SK, Mirza AJ, Chapman JR, Anderson PA. Classifications of thoracic and lumbar fractures: rationale and supporting data. J Am Acad Orthop Surg. 2002;10:364–77.
Patel AA, Vaccaro AR. Thoracolumbar spine trauma classification. J Am Acad Orthop Surg. 2010;18:63–71.
Van Middendorp JJ, Audigé L, Hanson B, Chapman JR, Hosman AJF. What should an ideal spinal injury classification system consist of? A methodological review and conceptual proposal for future classifications. Eur Spine J. 2010;19:1238–49.
Griffiths DL. The treatment of fractures. J Bone Jt Surg Br. 1957;39-B:608–8.
Ferguson RL, Allen BL. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res. 1984;189:77–88.
McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP.The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases a new classification.J Bone Joint Surg Am. 1983;65:461–73.
Magerl F, Aebi M, Gertzbein S, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar spine injuries. Eur Spine J. 1994;3:1–2.
Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harris M, Hedlund R, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209–15.
Kepler CK, Vaccaro AR, Schroeder GD, Koerner JD, Vialle LR, Aarabi B, et al. The thoracolumbar aospine injury score. Glob Spine J. 2016;6:329–34.
Reinhold M, Audigé L, Schnake KJ, Bellabarba C, Dai LY, Oner FC. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013;22:2184–201.
Chhabra HS, Kaul R, Kanagaraju V. Do we have an ideal classification system for thoracolumbar and subaxial cervical spine injuries: what is the expert’s perspective? Spinal Cord. 2015;53:42–8.
Audigé L, Bhandari M, Hanson B, Kellam J. A concept for the validation of fracture classifications. J Orthop Trauma. 2005;19:401–6.
Denis F. The three column spine and its significance in injury classification of acute thoracolumbar spinal injuries. Spine (Philos Pa 1976). 1983;8:8–9.
Denis F, Burkus JK. Shear fracture-dislocations of the thoracic and lumbar spine associated with forceful hyperextension (lumberjack paraplegia). Spine (Philos Pa 1976). 1992;17:156–61.
McAfee PC, Yuan HA, Lasda NA. The unstable burst fracture. Spine (Philos Pa 1976). 1982;7:365–73.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Pizones J, Izquierdo E, Sánchez-Mariscal F, Zúñiga L, Álvarez P, Gómez-Rice A. Sequential damage assessment of the different components of the posterior ligamentous complex after magnetic resonance imaging interpretation. Spine (Philos Pa 1976). 2012;37:E662–7.
McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Philos Pa 1976). 1994;19:1741–4.
Oner FC, Ramos LMP, Simmermacher RKJ, Kingma PTD, Diekerhof CH, Dhert WJA, et al. Classification of thoracic and lumbar spine fractures: problems of reproducibility. A study of 53 patients using CT and MRI. Eur Spine J. 2002;11:235–45.
Joaquim AF, Fernandes YB, Cavalcante RAC, Fragoso RM, Honorato DC, Patel AA. Evaluation of the thoracolumbar injury classification system in thoracic and lumbar spinal trauma. Spine (Philos Pa 1976). 2011;36:33–6.
Schnake KJ, Schroeder GD, Vaccaro AR. AOSpine Classification Syst (Subaxial, Thoracolumbar). J Orthop Trauma. 2017;31:14–23.
Vaccaro AR, Lehman RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Philos Pa 1976). 2005;30:2325–33.
Joaquim AF, Ghizoni E, Tedeschi H, Batista UC, Patel AA. Clinical results of patients with thoracolumbar spine trauma treated according to the Thoracolumbar Injury Classification and Severity Score. J Neurosurg Spine. 2014;20:562–7.
Whang PG, Vaccaro AR, Poelstra KA, Patel AA, Anderson DG, Albert TJ, et al. The influence of fracture mechanism and morphology on the reliability and validity of two novel thoracolumbar injury classification systems. Spine (Philos Pa 1976). 2007;32:791–5.
Rihn JA, Yang N, Fisher C, Saravanja D, Smith H, Morrison WB, et al. Using magnetic resonance imaging to accurately assess injury to the posterior ligamentous complex of the spine: a prospective comparison of the surgeon and radiologist. J Neurosurg Spine. 2010;12:391–6.
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, et al. AOSpine thoracolumbar spine injury classification system. Spine (Philos Pa 1976). 2013;38:2028–37.
Schmidt OI, Gahr RH, Gosse A, Heyde CE. ATLS® and damage control in spine trauma. World J Emerg Surg. 2009;4:9.
Longo UG, Loppini M, Petrillo S, Berton A, Maffulli N, Denaro V. Management of cervical fractures in ankylosing spondylitis: Anterior, posterior or combined approach? Br Med Bull. 2015;115:57–66.
Werner BC, Samartzis D, Shen FH. Spinal fractures in patients with ankylosing spondylitis. J Am Acad Orthop Surg. 2016;24:241–9.
Taggard DA, Traynelis VC. Management of cervical spinal fractures in ankylosing spondylitis with posterior fixation. Spine (Philos Pa 1976). 2000;25:2035–9.
Chen YJ, Lo DF, Chang CH, Chen HT, Hsu HC. The value of dynamic radiographs in diagnosing painful vertebrae in osteoporotic compression fractures. Am J Neuroradiol. 2011;32:121–4.
Glassman SD, Alegre GM. Adult spinal deformity in the osteoporotic spine: options and pitfalls. Instr Course Lect. 2003;52:579–88.
Clark CR, White AA. Fracture of the dens: a multicenter study. J Bone Jt Surg. 1985;67-A:1340–8.
Bartanusz V, Harris J, Moldavsky M, Cai Y, Bucklen B. Short segment spinal instrumentation with index vertebra pedicle screw placement for pathologies involving the anterior and middle vertebral column is as effective as long segment stabilization with cage reconstruction: a biomechanical study. Spine (Philos Pa 1976). 2015;40:1729–36.
Pellisé F, Barastegui D, Hernandez-Fernandez A, Barrera-Ochoa S, Bagó J, Issa-Benítez D, et al. Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures. Spine J. 2015;15:1796–803.
Lee GY, Lee JW, Choi SW, Lim HJ, Sun HY, Kang Y, et al. MRI inter-reader and intra-reader reliabilities for assessing injury morphology and posterior ligamentous complex integrity of the spine according to the thoracolumbar injury classification system and severity score. Korean J Radio. 2015;16:889–98.
McLane HC, Berkowitz AL, Patenaude BN, McKenzie ED, Wolper E, Wahlster S, et al. Availability, accessibility, and affordability of neurodiagnostic tests in 37 countries. Neurology. 2015;85:1614–22.
Insko EK, Gracias VH, Gupta R, Goettler CE, Gaieski DF, Dalinka MK. Utility of flexion and extension radiographs of the cervical spine in the acute evaluation of blunt trauma. J Trauma. 2002;53:426–9.
Acknowledgements
The following are experts, other than authors, who contributed to various studies and steps which were used for the development and validation of the classification system and we acknowledge gratefully their contribution: “Do we have an ideal classification system for thoracolumbar and subaxial cervical spine injuries: what is the expert’s perspective?”—Dr HS Chhabra, Dr Alex Vaccaro, Dr Rainer Abel, Dr Rahul Kaul, Dr Vijaynath Kanagaraju, Dr Krishna Prasad Paudel, Dr Sangan Patil, Dr Vikas Tandon, Dr Bimal Kumar Pandey, Dr Ankur Nanda, Dr Darshan Gautam, Dr Premik B Nagad, Dr K Venugopal Menon, Dr Rajagopalan, Dr Amrithlal Albert Mascarenhas, Dr Amish Sanghvi, Dr ML Bansal, Dr P Sarat Chandra, Dr. GD Sundararaj, Dr Sanjay Behari, Dr ATM Abdur Razzak, Dr Byapak Paudel, Dr SL Yadav, Prof. VP Sharma, Dr Saumyajit Basu, Prof. Roop Singh, Dr Abhay Nene, Dr Nishit Patel, Dr Gururaj Sangodimath, Dr Rupinder Pal Singh Chahal, Dr Bhavuk Garg, Dr Rabindra L Pradhan, Dr Sagun Tuli, Dr Kalidutta Das, Dr Nishit Patel, Dr Vivek Mittal. “Experts’ consensus algorithm for the management of Thoracolumbar fractures”—Dr HS Chhabra, Dr Raghavendra V, Dr P Karthik Yelamarthy, Dr Patrick Kluger, Dr Alex Vaccaro, Dr Scott Paquette, Dr Ajoy Shetty, Dr Ankur Nanda, Dr Bibhudendu Mohapatra, Dr Gururaj Sangodimath, Dr Kalidutta Das, Dr Nishit Patel, Dr Rajat Mahajan, Dr Saumjyajit Basu, Dr Vikas Tandon. Construct Validity Phase 2—Dr Kalidutta Das, Dr Bibhudendu Mohapatra, Dr Ankur Nanda, Dr Gururaj M Sangondimath, Dr Murari Lal Bansal, Dr Rajat Mahajan, Dr Nishit Patel, Dr Vikas Tandon, Dr Abhishek Srivastava, Dr HS Chhabra. We acknowledge also the contribution of Chris of Paper True Pte. Ltd for English language editing of the manuscript. We acknowledge the contribution of Ms Meenakshi Mohan in the compilation and submission of the manuscript and coordinating amongst co-authors in this regard. No funding has been availed for this manuscript.
Author information
Authors and Affiliations
Contributions
CHS conceived the classification system, contributed in designing the study, performing the literature review, performing the validation of the classification and writing the manuscript. MS has contributed in designing the study, performing the literature review, performing the validation of the classification and writing the manuscript. YK has contributed in designing the study, performing the literature review, performing the validation of the classification and writing the manuscript. EH has contributed in content validation of the classification system and substantively revising the manuscript. TF has contributed in content validation of the classification system and substantively revising the manuscript. AR has contributed in content validation of the classification system and substantively revising the manuscript. HM has contributed in content validation of the classification system and substantively revising the manuscript. TS has contributed in content validation of the classification system and substantively revising the manuscript. YS has contributed in content validation of the classification system and substantively revising the manuscript. HF has contributed in content validation of the classification system and substantively revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chhabra, H.S., Yelamarthy, P.K.K., Moolya, S.N. et al. Development and validation of a simplified thoracolumbar spine fracture classification system. Spinal Cord 59, 1268–1277 (2021). https://doi.org/10.1038/s41393-021-00706-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00706-5