Abstract
Study design
Longitudinal study in adults (n = 27; 19–40 years old) with tetraplegic or paraplegic spinal cord injury (SCI).
Objectives
Determine physiological adaptations and generalizable fitness effects of 6 months of whole-body exercise training using volitional arm and functional electrical stimulation (FES) leg rowing.
Setting
Outpatient hospital-based exercise facility and laboratory.
Methods
Participants enrolled in hybrid FES-row training (FESRT) and performed peak exercise tests with arms-only (AO; baseline and 6 months) and FES rowing (baseline, 3, 6 months).
Results
Participants demonstrated increased aerobic capacity (VO2peak) after FESRT (p < 0.001, np2 = 0.56) that tended to be higher when assessed with FES than AO rowing tests (0.15 ± 0.20 vs. 0.04 ± 0.22 L/min; p = 0.10). Changes in FES and AO VO2peak were significantly correlated (r = 0.55; p < 0.01), and 11 individuals demonstrated improvements (>6%) on both test formats. Younger age was the only difference between those who showed generalization of training effects and those who did not (mean age 26.6 ± 5.6 vs. 32.0 ± 5.7 years; p < 0.05) but changes in FES VO2peak correlated to time since injury in individuals <2 years post-SCI (r = −0.51, p < 0.01, n = 24). Lastly, VO2peak improvements were greater during the first 3 months vs. months 4–6 (+7.0% vs. +3.9%; p < 0.01) which suggests early training adaptations during FESRT.
Conclusions
Gains in aerobic capacity after whole-body FESRT are better reflected during FES-row testing format. They relate to high-intensity exercise and appear early during training, but they may not generalize to equivalent increases in AO exercise in all individuals with SCI.
Similar content being viewed by others
Introduction
Individuals with spinal cord injury (SCI) encounter an increased risk for cardiovascular disease and secondary health complications that is driven by physiological restrictions [1, 2]. Indeed, individuals with SCI have significantly lower aerobic capacity than able-bodied adults [3,4,5] since paralyzed muscles in SCI are unable to contribute to exercise and therefore to oxygen consumption. This limits muscle and cardiovascular engagement with daily activities, which are not vigorous enough stimuli to maintain fitness and decrease risk for cardiovascular disease [6]. The beneficial and protective cardiovascular health effects of aerobic exercise require training at sufficient intensity and volume [7,8,9]. In fact, moderate to vigorous intensity training that engages muscle mass beyond what is typically used is necessary to increase peak aerobic capacity (VO2peak) [10, 11] and decrease cardiovascular risk in those with SCI [12].
One manner for those with SCI to exercise at high intensities is by incorporating paralyzed muscle. Hybrid functional electrical stimulation (FES) exercise activates both voluntary upper-body and electrically stimulated lower-body musculature, and is a previously reported technique to overcome the physiological limitations of arms-only (AO) or FES legs-only exercise [13,14,15]. Hybrid FES exercise results in training adaptations that surpass those of arm crank exercise or FES-exercise alone [15,16,17,18]. For example, a review of SCI exercise training studies found that higher gains in VO2peak resulted from hybrid FES-row training (FESRT) when compared with hybrid FES cycling and simultaneous arm crank or FES cycling alone [2]. Furthermore, previous study showed that FESRT led to greater peak aerobic capacity compared with AO rowing [15]. Moreover, FESRT can circumvent physiological limitations of paralyzed muscle that otherwise restrict aerobic exercise, and allows increases in aerobic capacity among adults with neurological level of injury as high as C4 [19]. For wheelchair users with SCI, whole-body hybrid FESRT could avoid excess musculature strain of upper body-only exercise [20] and allows longer and more intense training sessions by incorporating lower body musculature [2]. However, it is not known whether improvements in aerobic capacity during FESRT generalize to greater aerobic capacity in upper-body exercise performance. Increases in VO2peak that result from exercise training are due to adaptations either centrally (i.e., increased maximal cardiac output) or peripherally (increased a-VO2 difference due to changes in trained skeletal muscle). Hence, an increase in aerobic capacity with one form of exercise may translate to increases with other forms of aerobic exercise. A generalization of improved aerobic capacity to upper-body exercise could decrease fatigue and physical strain during daily activities [21], increase community mobility [22], and hence have a great impact on independence for individuals with SCI.
Based on the training principles of specificity and overload, cardiorespiratory training adaptations are specific to those muscles or system exercised and occur when training is more intense than activities an individual did prior to training [23,24,25]. Given that the FESRT exercise stimulus involves volitional arm movements and facilitates high cardiorespiratory demands by incorporating electrically stimulated lower body movements, we investigated whether training the legs in nonambulatory individuals translated to increased AO exercise capacity. Hence, our study objective was to determine whether cardiorespiratory changes after FESRT would generalize to changes in fitness for AO exercise, by discriminating the contribution of the legs to changes in cardiorespiratory fitness. In the case of SCI and FESRT, if the adaptations were primarily peripheral, there may be no within-person increases in AO VO2peak tests (i.e., the stimulated legs account for the increase in aerobic capacity with FESRT). If adaptations were central, an increase in AO VO2peak might be observed due to greater maximal cardiac output (which is due to greater maximal stroke volume). This pre-post time series study examined changes in peak aerobic capacity (VO2peak) using two distinct testing methods: AO and FES tests on the rowing ergometer in the same individuals [15]. Between the tests, all participants performed 6 months of FESRT.
Methods
Participants
Inclusion criteria for eligible participants were age 18–40 years, and a time since SCI (TSI) of at least 3 months, and performed 6 months of FESRT. All participants had at least partially preserved arm function to row and had quadriceps and hamstring contractile responses to electrical stimulation. Participants gave their informed consent. This study was based at an outpatient hospital exercise facility and laboratory and part of the clinical trial #NCT02139436. This trial was amended to include individuals who were more chronically injured than in the original submission, and this study only analyzes data from those who performed FESRT. The original study and amendment were approved by the Spaulding Rehabilitation Network Institutional Review Board.
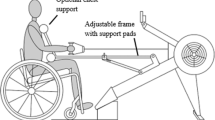
Rowing ergometer set-up
As previously described, Model D Indoor Rowers (Concept2 Inc., Morrisville, VT) were adapted for people with SCI (Paddlesport Training Systems/Vermont Waterways, Inc., Hardwick, VT) [15]. In AO row testing, the rowing seat was locked into place to isolate pull chain displacement for upper-body movements. For FES-row testing, electrodes were placed over the motor points of the quadriceps and hamstring muscles and attached to the electrical stimulator (Odstock 4 Channel Stimulator Kit, Odstock Medical Limited Inc, Salisbury, United Kingdom). To produce rowing strokes, participants synchronized electrical stimulation timing through a button on the rower handle. FESRT stimulator parameters were 300 ms pulse width and 40 Hz frequency without ramp, and stimulation intensity was increased to a maximum of 110 mA.
Measurement
Despite distinct set-up, the same measurement procedures were used during AO and FES rowing VO2peak tests. All participants were evaluated with AO and FES tests in a random order at baseline and after 6 months of FESRT within 1 week of each other. For FES rowing VO2peak, tests were also completed after 3 months of training. Baseline testing was conducted once participants could complete continuous FES rowing for ≥10 min. Individuals refrained from consuming food for 2 h prior and caffeine and alcohol for 24 h prior to testing, and from engaging in vigorous physical activity for 48 h prior. Peak aerobic capacity was determined from on-line computer-assisted open circuit spirometry (TrueOne 2400, Parvo Medics Inc, Sandy, UT). During graded aerobic capacity tests, ventilation, expired oxygen (O2), and carbon dioxide (CO2) were measured to determine VO2, CO2 production, and respiratory exchange ratio (RER; VCO2/VO2). Expired O2 and CO2 gas fractions were measured with a paramagnetic O2 and infrared CO2 analyzers. Throughout the tests, minute ventilation (VE) was measured via a pneumotachograph (Model 3813, Hans Rudolph Inc, Shawnee, KS), and heart rate (HR; beats/min) was measured with the Suunto memory belt (Suunto Inc, Vantaa, Finland).
Criteria of maximality
Aerobic capacity testing was individualized to the workload (Watts) and progression specific to each participant [15]. Workload was increased every 1–2 min until volitional exhaustion with a total testing time between 8 and 12 min [15, 19, 26]. To ensure attainment of peak exercise, at least three of the following criteria were met: (1) 85% of age predicted maximal HR (220—age), (2) RER > 1.1, (3) plateau in oxygen consumption despite increasing workload, (4) blood lactate of >8 mmol/L via finger prick (Lactate Plus Meter; Nova Biomedical, Waltham, MA) 60–90 s immediately upon aerobic capacity test completion, (5) rating of perceived exertion >17 on the Borg scale of 6–20, and, for FES test only, (6) precipitous decline in power >20 W despite maximal leg stimulation [15].
FESRT
All participants performed the same exercise training program within the outpatient hospital exercise facility for 6 months. The hybrid-adapted rowing training protocol included three FESRT sessions per week, ≥20 min duration per session, and an intensity progression from 60–70 to 75–90% of HRpeak over 6 months; the training session duration and intensity progression were individualized within these parameters and dependent on both previous and within-session performance.
Data analysis
Peak values (VO2peak, VEpeak, RERpeak, or HRpeak) were determined as the highest value obtained from 30-s rolling averages during the graded exercise tests. Univariate normality assumption and homogeneity of variances were verified with the Skewness/Kurtosis test and the Levene’s tests, respectively. Variables that violated homogeneity of variances assumptions were converted to logarithmic values. A two-way repeated measure analysis of variance (RMANOVA) with Holm–Sidak correction was used to determine the change in aerobic capacity (as well as for VEpeak, RERpeak, HRpeak, workload, and lactate) by test format (AO, FES), over time (0, 6 months) and the interaction between time and test. In addition, a one-way RMANOVA was applied to compare the magnitude of changes in FES rowing VO2peak over time (0, 3, and 6 months). The relationship between changes in VO2peak during AO vs. FES, as well as correlations between changes in VO2peak and participant characteristics (age, injury level, time since injury (TSI) and completeness of injury), were examined using Pearson correlation coefficients. For TSI, we kept a homogeneous range of subacute injury (TSI from 0.3 to 2.0 years, n = 24) and excluded three subjects with chronic injury (respectively 6, 8, and 19 years after injury). Partial eta-squared (np2) was calculated to determine the effect size. Reliability of VO2peak has a coefficient of variation of 4.7–5.7% with the TrueOne 2400 [27], so at least 6% increase in VO2peak (L/minute) in both AO and FES tests was considered an indicator of improved fitness. Based on this indication (≥6% increase vs. all others), we completed sub-analyses of demographic and training characteristics of the two groups with two-sample t-tests with unequal variance (for normally distributed variables) and two-sample Kolmogorov–Smirnov exact tests (for those not normally distributed). Analyses were completed using Stata 15 (Statacorp, College Station, Texas).
Results
Participants
Thirty-four participants were enrolled and completed 6 months of FESRT with baseline and 6-month VO2peak tests. Five of these participants did not complete both testing before and after training and two did not meet criteria for valid VO2peak tests and were excluded. The remaining 27 individuals were included in analyses below.
Median TSI was 1.2 years (0.4–19.5) and the mean age was 29.8 (6.2) years (Table 1). The most common International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) neurological level of motor was C7 (18.5%), and the ISNCSCI upper extremity motor score (UEMS) of 50 was most prevalent in the sample (30%, Table 1). More than half the participants had American Spinal Injury Association Impairment Score of A (55.6%), followed by B and C (each 22.2%). All but one participant were male. Average baseline VO2peak was low, reaching 18.4 (6.5) mL/kg/min with FES (i.e., 5.3 metabolic equivalent of a task [METs]) and 14.7 (6.0) mL/kg/min with AO (4.2 METs).
Training adaptations by test format
As expected when incorporating the lower body musculature into exercise, VO2peak (L/min) was higher during FES rather than AO row tests (np2 = 0.56, p < 0.001; Table 2). Participants demonstrated increased aerobic capacity (VO2peak) after FESRT (p < 0.001), and changes tended to be greater when assessed with FES than with AO rowing tests (0.15 [0.20] vs. 0.04 [0.22] L/min, np2 = 0.03, p = 0.10; Fig. 1). In addition, improvements in VEpeak were higher with FES compared with AO testing (p < 0.05). On average, increased VEpeak was observed between FES rowing tests (p < 0.05), whereas ventilation did not change between AO row tests. There was a general tendency of higher peak workload (p < 0.001) and peak lactate (p < 0.001) during FES testing compared with AO testing, but without significant differences by test over time (Table 2). No changes were found for peak HR in either testing condition.
Individual values and box plot (median, 10th, 25th, 75th, and 90th percentiles with error bar) of peak aerobic capacity (VO2peak) during a maximal incremental exercise using arms-only row testing (left panel) or FES-row testing (right panel), before and after 6 months of FES-row training. The p = 0.10 value represents the difference in change of VO2peak by test format.
Generalization of changes during FESRT
Changes in VO2peak during AO correlated with those during FES-row tests (r = 0.55; p < 0.01; Fig. 2). The 11 participants who improved VO2peak by at least 6% (see “Methods”) on both tests had an average change of 0.27 (0.18) L/min on FES and 0.24 (0.16) L/min on AO row tests. Nevertheless, there was only a partial generalization of training effects for eight individuals who improved VO2peak on FES but not on AO row tests. Those who did not increase VO2peak on both tests had an average change of 0.07 (0.18) L/min on FES and −0.09 (0.13) L/min on AO row tests.
Individuals who increased aerobic capacity on both FES and AO tests were significantly younger than those who showed no generalization of training effects (26.6 [5.6] vs. 32.0 [5.7] years; p = 0.02). Furthermore, changes in FES VO2peak inversely correlated to TSI in individuals <2 years post-SCI (r = −0.51, p < 0.01, n = 24) suggesting that those with the best response to FESRT had a shorter TSI. However, no clinical factors (neurological level of injury, UEMS, AIS, TSI) significantly differed between participants with improved AO and FES VO2peak and those without generalized aerobic fitness gains. Furthermore, we found compliance and engagement in training were similar between the groups: no difference was found in average training frequency (session/week), HR, or session duration (p > 0.30). Participants completed an average of 1.7 (0.5) sessions per week, which is 57% of the prescribed 3 sessions/week, that were 22.2 (6.7) min in duration. Average training HR was 119.4 (19.2) beats/min, which was 63% [10] of age-adjusted HRpeak and 81% [7] of baseline HRpeak.
Lastly, 25 of the 27 participants completed 3-month FES-row tests so this study examined the progression of aerobic capacity over time in FES condition only. There was a significant effect of time on VO2peak (F(2,48) = 6.8; p = 0.0025; Fig. 3), with average improvements of 7.0% between baseline and 3 months (p = 0.02) vs. 3.9% over months 4 through 6 (p = 0.001).
Significant improvements in FES VO2peak occurred between baseline and 3 months (7.0%; p = 0.02) and over months 4 through 6 (3.9%; p = 0.001). Nevertheless, increases in FES VO2peak were greater during the first 3 months of training than in months 3–6 (p = 0.0025), which suggests most of the physiological adaptations appear early in training.
Discussion
Whole-body hybrid FESRT led to significant improvements in aerobic capacity among individuals with SCI when evaluated during FES-row testing. These findings have potential notable cardiorespiratory health benefits. However, under half of participants had aerobic capacity gains that generalized to work done by the upper body only. Hence, only a subgroup of participants could potentially transfer the benefits from FESRT to daily AO (wheelchair-based) activities and this generalization seemed more likely to occur in younger subjects. Greater capacity to reach higher-intensity exercise, higher maximal cardiac output, and greater preservation of upper-body muscle mass in younger individuals are potential key reasons for generalization of the gains. Lastly, increases in FES VO2peak were greater during the first 3 months of training than in the second 3 months, suggesting that most of the physiological adaptations appear early in training.
Improvements in cardiorespiratory fitness prevent worsening physical health and physical dependence. For example, greater aerobic capacity decreases the risk for all-cause and cardiovascular disease mortality independent of age, ethnicity, and health conditions in able-bodied adults [14, 28,29,30,31]. Specifically, a 3 ml/kg/min improvement in aerobic capacity relates to a 15% drop in all-cause and a 19% decrease in cardiovascular disease mortality [32, 33]. Study participants experienced even higher average improvements in their aerobic capacity after FESRT suggesting that they accrued health benefits. Importantly for individuals with SCI, greater fitness is also related to improved mood [34], higher functional independence [35, 36], and lower physical strain during daily activities [21].
The small tendency of greater improvement in VO2peak when assessed with FES-row testing compared with AO row testing underlines the cardiorespiratory benefit of engaging greater muscle mass with FESRT, or in other words, the generalizable fitness effects of FESRT. Though we did not measure cardiac output or muscle composition and cannot conclude the origin of physiological training adaptations, the greater improvement in peak ventilation with FES compared with AO suggests that the addition of the legs led to higher cardiorespiratory engagement in this condition of training and testing. In contrast, the lower-intensity AO test may have precluded observation of ventilatory changes because the cardiorespiratory system was not engaged sufficiently and fewer muscles were activated. If the change in FES aerobic capacity was due solely to central cardiorespiratory improvements, more participants would have shown equivalent improvements on the AO row tests. A study of changes in VO2peak after robotic body weight supported treadmill training found similar partial generalization to VO2peak during arm-only cycling (+8.5%, p = 0.25) [37]. In the absence of specific upper-body training, researchers attributed this change to possible central cardiorespiratory adaptations. In comparison, the present study trained the arms during FESRT and it is possible that upper-body muscular adaptations, peripheral in origin, contributed to improvements in AO VO2peak.
Improvements in aerobic capacity were greater among younger participants. This finding suggests that a few additional years within a decade of life could limit the cardiorespiratory adaptations of FESRT for some individuals with SCI. Younger individuals are potentially more active and have greater upper-body muscle mass, whereas a decline in muscle mass often accompanies aging and the adoption of a more sedentary lifestyle [38]. Such a small difference of 6 years may not be clinically relevant in able-bodied aging but could have implications for upper-body muscle structure and function among adults with SCI and subsequent consequences on aerobic capacity gains. Furthermore, within 2 years of SCI the changes in aerobic capacity were greater in those who began FESRT sooner. Though inferences are limited by our small heterogeneous sample, this relationship nevertheless emphasizes a cardiorespiratory merit to whole-body exercise training that begins shortly after SCI.
Lastly, aerobic capacity gains were greatest in the first 3 months of training. It is possible that participants reached a plateau in aerobic capacity after 3 months of FESRT and encountered physiological barriers, due to muscle [39], cardiac [40], or to ventilatory limits [1, 26, 40]. For example, Qui and colleagues previously reported that after several months of FES rowing, training-related increases in peak aerobic capacity were markedly dependent on peak ventilation in those with high-level SCI [26]. Improvements in muscle metabolism and/or cardiovascular function after FESRT may outstrip the pulmonary system’s ability to generate greater ventilation, and Vivodtzev and colleagues showed that ventilatory support can reverse both VEpeak and VO2peak limitations in these individuals [41].
In conclusion, gains in aerobic capacity after whole-body FESRT are better reflected when the testing includes FES in individuals with SCI. Aerobic capacity improvements (+10%) were likely incited by leg activity and cardiorespiratory adaptations that can occur within 3 months of FESRT. Such improvement in aerobic capacity may lead to considerable implications for cardiovascular health. However, gains in aerobic capacity after FESRT may not generalize to equivalent increases in AO exercise for all participants. Younger adults, potentially because of better preserved upper-body muscle function and/or cardiorespiratory function, may be more prone to have generalization of FESRT benefits.
Data availability
Part of the dataset generated during and analyzed in this study is not publicly available because it is still being analyzed, but the data can be made available from the senior author on reasonable request.
References
Battikha M, Sa L, Porter A, Taylor JA. Relationship between pulmonary function and exercise capacity in individuals with spinal cord injury. Am J Phys Med Rehabil. 2014;93:413–21.
Hettinga DM, Andrews BJ. Oxygen consumption during functional electrical stimulation-assisted exercise in persons with spinal cord injury: implications for fitness and health. Sports Med. 2008;38:825–38.
Hooker SP, Greenwood JD, Hatae DT, Husson RP, Matthiesen TL, Waters AR. Oxygen uptake and heart rate relationship in persons with spinal cord injury. Med Sci Sports Exerc. 1993;25:1115–9.
Van Loan MD, McCluer S, Loftin JM, Boileau RA. Comparison of physiological responses to maximal arm exercise among able-bodied, paraplegics and quadriplegics. Paraplegia. 1987;25:397–405.
Vinet A, Le Gallais D, Bernard PL, Poulain M, Varray A, Mercier J, et al. Aerobic metabolism and cardioventilatory responses in paraplegic athletes during an incremental wheelchair exercise. Eur J Appl Physiol Occup Physiol. 1997;76:455–61.
Hoffman MD. Cardiorespiratory fitness and training in quadriplegics and paraplegics. Sports Med. 1986;3:312–30.
Stanton R, Reaburn P. Exercise and the treatment of depression: a review of the exercise program variables. J Sci Med Sport. 2014;17:177–82.
Totosy de Zepetnek JO, Pelletier CA, Hicks AL, MacDonald MJ. Following the physical activity guidelines for adults with spinal cord injury for 16 weeks does not improve vascular health: a Randomized Controlled Trial. Arch Phys Med Rehabil. 2015;96:1566–75.
van der Scheer JW, de Groot S, Tepper M, Faber W, Veeger DH, van der Woude LH. Low-intensity wheelchair training in inactive people with long-term spinal cord injury: a randomized controlled trial on fitness, wheelchair skill performance and physical activity levels. J Rehabil Med. 2016;48:33–42.
Hicks AL, Martin Ginis KA, Pelletier CA, Ditor DS, Foulon B, Wolfe DL. The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord. 2011;49:1103–27.
Hasnan N, Mohamad Saadon NS, Hamzaid NA, Teoh MX, Ahmadi S, Davis GM. Muscle oxygenation during hybrid arm and functional electrical stimulation-evoked leg cycling after spinal cord injury. Medicine. 2018;97:e12922.
Nightingale TE, Metcalfe RS, Vollaard NB, Bilzon JL. Exercise guidelines to promote cardiometabolic health in spinal cord injured humans: time to raise the intensity? Arch Phys Med Rehabil. 2017;98:1693–704.
Deley G, Denuziller J, Babault N. Functional electrical stimulation: cardiorespiratory adaptations and applications for training in paraplegia. Sports Med. 2015;45:71–82.
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
Taylor JA, Picard G, Widrick JJ. Aerobic capacity with hybrid FES rowing in spinal cord injury: comparison with arms-only exercise and preliminary findings with regular training. PM R 2011;3:817–24.
Brurok B, Helgerud J, Karlsen T, Leivseth G, Hoff J. Effect of aerobic high-intensity hybrid training on stroke volume and peak oxygen consumption in men with spinal cord injury. Am J Phys Med Rehabil. 2011;90:407–14.
Gibbons RS, Stock CG, Andrews BJ, Gall A, Shave RE. The effect of FES-rowing training on cardiac structure and function: pilot studies in people with spinal cord injury. Spinal Cord. 2016;54:822–9.
Jung DW, Park DS, Lee BS, Kim M. Development of a motor driven rowing machine with automatic functional electrical stimulation controller for individuals with paraplegia; a preliminary study. Ann Rehabil Med. 2012;36:379–85.
Taylor JA, Picard G, Porter A, Morse LR, Pronovost MF, Deley G. Hybrid functional electrical stimulation exercise training alters the relationship between spinal cord injury level and aerobic capacity. Arch Phys Med Rehabil. 2014;95:2172–9.
Olenik LM, Laskin JJ, Burnham R, Wheeler GD, Steadward RD. Efficacy of rowing, backward wheeling and isolated scapular retractor exercise as remedial strength activities for wheelchair users: application of electromyography. Paraplegia. 1995;33:148–52.
Dallmeijer AJ, Hopman MT, van As HH, van der Woude LH. Physical capacity and physical strain in persons with tetraplegia; the role of sport activity. Spinal Cord. 1996;34:729–35.
Bresnahan JJ, Farkas GJ, Clasey JL, Yates JW, Gater DR. Arm crank ergometry improves cardiovascular disease risk factors and community mobility independent of body composition in high motor complete spinal cord injury. J Spinal Cord Med. 2018;42:1–21.
Franklin BA. Aerobic exercise training programs for the upper body. Med Sci Sports Exerc. 1989;21(5 Suppl):S141–8.
Pechar GS, McArdle WD, Katch FI, Magel JR, DeLuca J. Specificity of cardiorespiratory adaptation to bicycle and treadmill training. J Appl Physiol. 1974;36:753–6.
Hoffman J. Physiological aspects of sport training and performance. 2nd ed. Champaign, IL: Human Kinetics; 2014.
Qiu S, Alzhab S, Picard G, Taylor JA. Ventilation limits aerobic capacity after functional electrical stimulation row training in high spinal cord injury. Med Sci Sports Exerc. 2016;48:1111–8.
Crouter SE, Antczak A, Hudak JR, DellaValle DM, Haas JD. Accuracy and reliability of the ParvoMedics TrueOne 2400 and MedGraphics VO2000 metabolic systems. Eur J Appl Physiol. 2006;98:139–51.
Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328:533–7.
Blair SN, Kohl HW, 3rd, Jr Paffenbarger RS, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262:2395–401.
Kokkinos P, Myers J, Kokkinos JP, Pittaras A, Narayan P, Manolis A, et al. Exercise capacity and mortality in black and white men. Circulation. 2008;117:614–22.
Mora S, Redberg RF, Cui Y, Whiteman MK, Flaws JA, Sharrett AR, et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: a 20-year follow-up of the lipid research clinics prevalence study. JAMA. 2003;290:1600–7.
Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124:2483–90.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35.
Akkurt H, Karapolat HU, Kirazli Y, Kose T. The effects of upper extremity aerobic exercise in patients with spinal cord injury: a randomized controlled study. Eur J Phys Rehabil Med. 2017;53:219–27.
Noreau L, Shephard RJ, Simard C, Pare G, Pomerleau P. Relationship of impairment and functional ability to habitual activity and fitness following spinal cord injury. Int J Rehabil Res. 1993;16:265–75.
Hjeltnes N, Jansen T. Physical endurance capacity, functional status and medical complications in spinal cord injured subjects with long-standing lesions. Paraplegia. 1990;28:428–32.
Gorman PH, Scott W, York H, Theyagaraj M, Price-Miller N, McQuaid J, et al. Robotically assisted treadmill exercise training for improving peak fitness in chronic motor incomplete spinal cord injury: a randomized controlled trial. J Spinal Cord Med. 2016;39:32–44.
McGregor RA, Cameron-Smith D, Poppitt SD. It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev Healthspan. 2014;3:9.
Simmons OL, Kressler J, Nash MS. Reference fitness values in the untrained spinal cord injury population. Arch Phys Med Rehabil. 2014;95:2272–8.
Brizuela G, Sinz S, Aranda R, Martinez-Navarro I. The effect of arm-crank exercise training on power output, spirometric and cardiac function and level of autonomy in persons with tetraplegia. Eur J Sport Sci. 2019:1–9. https://doi.org/10.1080/17461391.2019.1674927.
Vivodtzev I, Picard G, Cepeda FX, Taylor JA. Acute ventilatory support during whole-body hybrid rowing in patients with high-level spinal cord injury: a Randomized Controlled Crossover Trial. Chest. 2019;157:1230–40.
Acknowledgements
The authors would like to acknowledge the generous support of our funding agencies, the study participants, and the staff at the Exercise for Persons with Disabilities program.
Funding
This study was supported by the Craig H. Neilsen Foundation (542007), the National Institutes of Health (R01HL117037), National Institute on Disability, Independent Living, and Rehabilitation Research (90SI5021), and the Gordon Center for the Cure and Treatment of Paralysis.
Author information
Authors and Affiliations
Contributions
HWM was responsible for study conceptualization, data analysis and interpretation, and writing and revising the manuscript. GP was responsible for data acquisition and conducting exercise tests, and he supervised FESRT. JAT was responsible for study conceptualization, data interpretation, and revising the manuscript. IV was responsible for study conceptualization, data analysis and interpretation, and writing and revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mercier, H.W., Picard, G., Taylor, J.A. et al. Gains in aerobic capacity with whole-body functional electrical stimulation row training and generalization to arms-only exercise after spinal cord injury. Spinal Cord 59, 74–81 (2021). https://doi.org/10.1038/s41393-020-0527-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0527-2