Abstract
Study design
Protocol for a pragmatic randomized controlled trial (the Exercise guideline Promotion and Implementation in Chronic SCI [EPIC-SCI] Trial).
Primary objectives
To test if home-/community-based exercise, prescribed according to the international SCI exercise guidelines, significantly reduces chronic bodily pain in adults with SCI.
Secondary objectives
To investigate: (1) the effects of exercise on musculoskeletal and neuropathic chronic pain; (2) if reduced inflammation and increased descending inhibitory control are viable pathways by which exercise reduces pain; (3) the effects of chronic pain reductions on subjective well-being; and (4) efficiency of a home-/community-based exercise intervention.
Setting
Exercise in home-/community-based settings; assessments in university-based laboratories in British Columbia, Canada.
Method
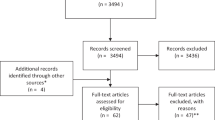
Eighty-four adults with chronic SCI, reporting chronic musculoskeletal or neuropathic pain, and not meeting the current SCI exercise guidelines, will be recruited and randomized to a 6-month Exercise or Wait-List Control condition. Exercise will occur in home/community settings and will be supported through behavioral counseling. All measures will be taken at baseline, 3-months and 6-months. Analyses will consist of linear mixed effect models, multiple regression analyses and a cost–utility analysis. The economic evaluation will examine the incremental costs and health benefits generated by the intervention compared with usual care.
Ethics and dissemination
The University of British Columbia Clinical Research Ethics Board approved the protocol (#H19–01650). Using an integrated knowledge translation approach, stakeholders will be engaged throughout the trial and will co-create and disseminate evidence-based recommendations and messages regarding the use of exercise to manage SCI chronic pain.
Trial registration
ClinicalTrials.gov identifier NCT04160858.
Similar content being viewed by others
Introduction
At least 60% of people with a spinal cord injury (SCI) live in chronic pain [1], due to damage to the somatosensory nervous system (i.e., neuropathic pain), as well as overuse of the upper body (i.e., musculoskeletal [MSK] pain [2]). Post-SCI chronic pain is so damaging to physical functioning and subjective well-being [3, 4] that many consider the pain to be more debilitating than the SCI itself [5]. Pharmaceuticals are the recommended front-line treatment for post-SCI chronic pain, but have many negative side effects and provide only limited relief [6]. The personal, social and economic burdens of unmanaged post-SCI chronic pain speak to the critical need for research to develop better treatments.
Exercise may be a viable treatment. People with SCI report exercising to manage chronic pain [7]. SCI RCTs have reported significant chronic bodily pain reduction as a secondary outcome [8, 9] and reductions in MSK shoulder pain as a primary outcome [9,10,11]. Furthermore, results from two quasi-experimental studies suggest exercise might provide relief from SCI neuropathic pain [12, 13]. However, the effects of exercise on chronic pain, as a primary outcome, have yet to be tested in an adequately-powered RCT of SCI chronic pain experiencers, using a standardized exercise prescription, under real-world conditions.
Exercise prescriptions used in SCI RCTs have been inconsistent and often arbitrary [14]. The recent publication of International Scientific SCI Exercise Guidelines (a guideline to improve fitness and another to improve cardiometabolic health [CMH]) has provided standardized evidence-based exercise guidelines that can be used in research [15]. In SCI RCTs, exercising according to the fitness guideline significantly reduced chronic bodily pain [8] while exercising according to the CMH guideline decreased inflammation levels [16]. Decreased inflammation is a pathway by which exercise may reduce chronic SCI bodily pain, specifically through its effects on MSK and neuropathic pain [17, 18]. Exercise may also increase descending inhibitory autonomic control, potentially reducing chronic bodily pain [19]. No SCI exercise training study has tested these potential pathways of pain reduction.
SCI exercise training studies have been criticized for their low pragmatic value [20]. For research to support real-world interventions, it must be conducted with representative samples and settings. Accordingly, we designed a pragmatic RCT with the primary objective of testing if home-/community-based exercise, prescribed according to the SCI guidelines [15], significantly reduces chronic bodily pain in adults with SCI (the Exercise guideline Promotion and Implementation in Chronic SCI [EPIC-SCI] Trial). Secondary objectives are to investigate: (1) differential effects of exercise on chronic MSK and neuropathic pain; (2) reduced inflammation and increased descending inhibitory control as pathways by which exercise reduces pain; (3) effects of exercise-induced chronic pain reductions on subjective well-being; and (4) the efficiency of a home-/community-based exercise intervention compared with a usual care group.
Methods
Design
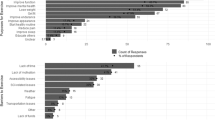
EPIC-SCI is a two-arm, single-blinded (i.e., assessors and analysts blinded to allocation), pragmatic RCT with a 6-month intervention period. After baseline assessments, participants will be randomly allocated to 6 months of exercise (“Exercise”) or a wait-list (“Control”) using a 1:1 ratio. Follow-up assessments will occur in both groups after 3 and 6 months. The RCT is designed to maximize pragmatism, as quantified by PRagmatic Explanatory Continuum Indicator Summary (PRECIS)-2 scores (Fig. 1 and Supplement 1), while providing insight on mechanisms that may explain intervention effects. The RCT was formulated using integrated knowledge translation principles (i.e., the exercise prescription [15, 21], behavioral intervention [22] and testing protocol were co-created with >150 people with SCI and >50 SCI clinicians) and is reported according to the SPIRIT Statement (Supplement 2).
Scoring each domain is done using a 5-point Likert scale: (1) Very explanatory; (2) Rather explanatory; (3) Equally pragmatic and explanatory; (4) Rather pragmatic; (5) Very pragmatic. See Supplementary File 1 for the rationale for each score.
Setting
EPIC-SCI takes place at the Vancouver and Okanagan campuses of the University of British Columbia (UBC) in Canada. Participants will visit one of these sites for outcome assessments. Participants may exercise in their homes, gyms and/or community centers.
Inclusion and exclusion criteria
Table 1 presents the inclusion and exclusion criteria.
Eligibility screening and informed consent
A research coordinator will administer a study eligibility checklist to screen interested individuals. Eligible individuals will receive detailed study information and the informed consent form (Supplement 3) to review, sign and return to the coordinator.
Intervention
The Exercise condition intervention is a personalized exercise prescription based on the international scientific SCI exercise guidelines and messaged according to the Canadian SCI community physical activity guideline (www.sciguidelines.com) [21]. All participants will start with instructions from a fitness trainer to complete 20 min of aerobic exercise, two times/week, at 70% of their heart rate reserve (or a Borg CR-10 rating of 6 if level of injury precludes using HRR), plus three sets of 10 repetitions of strengthening exercises for each major functioning muscle group at 50–80% of the estimated 1 rep-max [23], two times/week. Target heart rate, strengthening exercises and loads will be determined at baseline and 3-month fitness testing. Participants may break up the exercise as needed (e.g., two 10-min bouts) and work up to 20 min of continuous exercise. Participants will be instructed to gradually increase aerobic exercise to 30 min, three times/week, progressing at their own rate.
Exercise implementation will be supported by certified fitness trainers and exercise counsellors with SCI-specific training and experience. The trainer will visit each participant in their preferred exercise location in weeks 1 and 13 for instruction on how to do the prescribed exercise, how to self-monitor exercise intensity, and to check exercise progression. Pragmatically, the visits compare with free personal training sessions given to new gym members. Over the 6-month intervention period, the trained exercise counsellor will make one 15-min phone/videoconference contact/week with Exercise participants to check health and safety, adherence and exercise progression, and deliver a theory- and evidence-based behavioral intervention [22, 24]. Personalized behavior change techniques, which are guided by Schwarzer’s Health Action Process Approach model, will be applied according to individual needs and preferences. Additional intervention details are described elsewhere (see Supplement 4 and OSF). Pragmatically, this intervention compares with free, individualized telephone information services provided in British Columbia (Canada) by Physical Activity Services at HealthLink BC and SCI British Columbia’s SCI InfoLine.
Control participants will not get an exercise prescription. To mimic usual care, they will be asked to continue their usual activities for the next 6 months. After the waitlist period, Controls will receive the same services as Exercisers.
Primary outcome measure
Supplement 5 includes a referenced summary of the study measures. To meet journal guidelines, references have been excluded here. The primary outcome measure is the two-item SF-36 Pain subscale measuring bodily pain severity and interference during the past 4 weeks, assessed at 3 and 6-months follow-up. Item scores are combined into a single composite score (0–100 scale); lower scores indicate greater pain. SF-36 Pain was chosen as the primary outcome because, aligning with principles of a pragmatic RCT, it is commonly used in SCI clinical settings [25] and captures pain factors (interference and severity/intensity) reported by people with SCI to impact quality of life [26]. It is SCI experts’ #1 recommended measure for a minimum pain dataset and for clinical trials [27], has shown acceptable reliability and validity in SCI samples [28] and sensitivity to change in SCI exercise RCTs [8, 9]. Normative data are available from Canada and abroad.
Secondary outcome measures
MSK and neuropathic pain
The International SCI Pain Basic Data Set v2.0, will measure overall interference of MSK and neuropathic pain, and intensity of each specific pain location and type (up to three pain problems). It has shown acceptable reliability and validity in clinical and research settings. Neuropathic versus MSK pain will be discriminated using Douleur Neuropathique 4 questions (DN4) which have shown acceptable psychometrics in SCI [29]. Pain coping strategies will be assessed using the seven-item Coping Strategies Questionnaire (CSQ).
Inflammation and inhibitory control
Fasting plasma concentrations of cytokines interleukin (IL)-6 and tumour necrosis factor (TNF)-α will be measured. Although other cytokines and immune system markers may also indicate low-grade inflammation, these have not been consistently linked to both pain and exercise in SCI. To limit Type 1 errors, we will focus on IL-6 and TNF-α. To measure inhibitory control of pain, conditioned pain modulation testing will be used. This technique has been validated for use in SCI individuals [30, 31] and measures the ‘pain inhibiting pain’ effect, i.e., the extent to which the application of a painful conditioning stimulus changes the perceived painfulness of a test stimulus. Inhibitory control is calculated as the change in pain ratings for the test stimulus, from before to after application of the conditioning stimulus (bigger decreases in pain ratings indicate better inhibitory control/pain modulation).
Subjective well-being (SWB)
SWB correlates of pain [13, 32] will be measured using the Perceived Stress Scale, SCI-QOL measures of Positive Affect and Well-Being, and Satisfaction with Social Roles and Activities, Diener’s Satisfaction with Life Scale and the SF-36 Vitality scale measure of fatigue.
Economic evaluation measures
The 5-level version of the EuroQol-5D (EQ-5D-5L) will be administered and used to calculate a health state utility value. The ICECAP-A (ICEpop CAPability Measure for Adults) will be used to assess wellbeing. A health resource utilization questionnaire will be used to quantify health care system-related costs during the study period.
Inflammation fidelity checks
A white-blood-cell count will be performed on each sample to check/control for acute infection that may influence inflammatory markers.
Intervention fidelity checks
The exercise counsellor will ask participants, during each weekly call, to report their previous week’s exercise activities using a modified version of the Leisure Time Physical Activity Questionnaire SCI that separately captures strength and aerobic exercise. Adherence (%) to the SCI exercise guidelines over the course of the intervention will be calculated. Participants will complete the Measure of Experiential Aspects of Participation (MeEAP) at 3- and 6-month follow-ups to assess the quality of their exercise experiences. If participants adhere to the guidelines, improvements in fitness and cardiometabolic health outcomes are expected [14, 15]. Therefore, changes in cardiorespiratory fitness and muscle strength will be checked using a progressive arm crank test and maximum upper-body strength tests, respectively. Anticipated effects on CMH will be checked through fasting glucose, insulin and lipid profiles.
To support the fitness trainer and exercise counselor’s protocol fidelity, both will complete checklists/reports during each session. All counselling sessions will be audio-recorded and a random sub-sample will be analyzed using State Space Grids, a dynamic systems methodology, to characterize counselors’ delivery of, and clients’ responses to, behavior change techniques. Bi-monthly, the PI and a research assistant will review random samples of checklists and recordings, and make real-time observations of fitness-trainer sessions. If protocol deviations occur, the PI will provide corrective feedback.
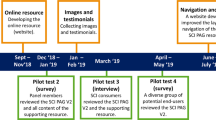
Measurements
Demographic, medication and health information will be collected at the baseline testing session. Baseline, 3- and 6-month testing will include questionnaires, blood sampling and fitness testing completed in a single day, at the relevant site. Figure 2 provides the timeline.
t1 = baseline; t2 = 3 months; t3 = 6 months. *Control group will receive the same intervention as the Exercise group after t3. MSK musculoskeletal; **The intervention fidelity checks include (1) participants’ adherence to the SCI exercise guidelines, assessed throughout the intervention period; (2) changes in participants’ cardiorespiratory fitness, muscle strength and cardiometabolic health, assessed at 3-months and 6-moths; (3) fitness trainer’s and counsellor’s adherence to the intervention protocol assessed throughout the intervention period using checklists, recordings and observations.
Questionnaires
The International SCI Pain Basic Data Set v2.0 and DN4 will be administered in interview format, as per protocol recommendations. All other questionnaires will be administered using a computer tablet interface.
Conditioned Pain Modulation (CPM)
To limit distraction biases, CPM testing will use a sequential, rather than parallel paradigm (i.e., presentation of the ‘conditioned’ test stimulus immediately after the conditioning stimulus). The test stimulus will be delivered via pressure algometer (contact area 1 cm2; Algomed Computerized Algometry; Medoc AMS) applied to the upper trapezius muscle (area with preserved sensory function). Three slowly increasing stimulus intensities will be applied (0.5 kg/s, corresponding to approximately 50 kPa/s). Participants will be instructed to say “now” immediately when pain is perceived, over and above the perception of pressure [33]. Pain threshold will be calculated as the mean response to the three applications (in kPA). One practice application will precede the series. After a 5-minute rest, the conditioning stimulus will be delivered by immersing the hand (contralateral) up to the bony prominences of the wrist, in a cold-water bath kept at 12 °C for 60 s [34] (measured by a calibrated quicksilver thermometer [0–100 °C with accuracy of ±1 °C] [34]). Immediately after, the test stimulus protocol will be repeated. Change in mean test stimulus pain ratings (before versus after cold-water immersion) will be calculated.
Blood sample
A fasting blood sample (>12 h) will be taken from the antecubital vein. IL-6 and TNF-α will be measured by V-plex assay (MSD Inc.); fasting glucose will be measured on an automated analyzer using the hexokinase method and insulin by ELISA (Crystal Chem Inc.) with homeostasis model assessment of insulin resistance (HOMA-IR) calculated [35]. Triglycerides, total cholesterol and HDL-cholesterol will be assessed by automated analyzer with LDL-cholesterol calculated.
Peak aerobic exercise capacity testing
Peak oxygen uptake and peak power output will be assessed in all participants, regardless of ambulatory status [36], using a Lode arm crank ergometer (Groningen, the Netherlands) and metabolic cart (TrueOne® 2400, ParvoMedics, Utah). Peak oxygen uptake will be verified using the following criteria: RER > 1.10, Borg ratings of perceived exertion (6–20 scale) > 17, a plateau in VO2 response despite increases in power output, and/or volitional exhaustion [36]. Strength will be assessed with 4–12 repetition maximum bench press and seated row tests [23] using HUR strength equipment (Kokkola, Finland). Participants’ one-repetition maximum will be estimated using procedures described elsewhere [23].
Sample size
Using between-factors repeated measures, G*Power estimates N = 70 provides 80% power (alpha = 0.05) to detect d = 0.34 between the Exercise and Control conditions for the primary outcome of SF-36 Pain. d = 0.34 is the between-groups difference in SF-36 Pain reported by Hicks et al. [8] after 6 months of lab-based exercise with participants completing M = 82.5% of prescribed exercise sessions. Budgeting for 20% loss to follow-up, we will recruit a sample of n = 84.
Statistical methods
Linear mixed effect models will test for differences in change over time between the two conditions, adjusting for potential covariates, to be determined prior to analysis. Analyses will be based on intention-to-treat, including all participants with baseline and 6-month data. Multiple imputation will replace missing data. Multiple regression analyses will test whether changes in inflammation and inhibitory control explain significant variance in pain changes after adjusting for potential covariates. A per-protocol analysis (i.e., participants with ≥80% exercise prescription adherence [8]) will be conducted and results compared to intention-to-treat in sensitivity analysis. Descriptive statistics and effect sizes will be calculated separately for males and females, men and women, paraplegics and tetraplegics, and complete and incomplete injuries. The economic evaluation will examine the efficiency of a 6-month home-/community-based exercise program compared with usual care. The outcome of our cost–utility analysis is the incremental cost–utility ratio (ICUR): ICUR = ∆Cost/∆ Quality Adjusted Life Years (QALYs). QALYs (measured using health state utility values estimated from the EQ-5D-5L) represent time spent in given health states [37].
Recruitment
Participants will be recruited from the Vancouver and Okanagan Valley areas via emails to previous study participants and advertising through community partners, social media and word-of-mouth.
Allocation
After a participant’s baseline testing session, the site coordinator will contact an external research coordinator. She will use a password-protected allocation website (programmed by an independent institute) to produce an audit trail recording date and time of randomization, participant letter code and study identification number and treatment allocation. Participants will be stratified by gender. The SAS PLAN procedure will computer-generate allocation sequences using random block sizes (details revealed once data published). The site coordinator will access the randomization report on the password-protected website and communicate the group allocation to the participant.
Blinding
Methods to protect against bias include keeping outcome assessors and data analysts blinded to group allocation (i.e., participants and groups identifiable by number only). When participants arrive at the lab for testing, they will be instructed not to reveal their allocated condition. Similar to usual care settings, it is impossible to blind participants, the fitness trainer or counsellor.
Compliance and retention
Compliance challenges include the many exercise barriers faced by people with SCI. Adherence will be supported by weekly exercise counseling sessions and home-based exercise specifically designed to alleviate barriers. Compliance to testing will be supported by remuneration for each lab visit. Participants choosing to stop exercising will be asked to continue with testing sessions, as per intention-to-treat principles. A possible compliance challenge for Controls is dissatisfaction with group allocation. We will emphasize that the same intervention and supports will be provided after the waitlist period, an approach supporting 100% retention of Controls in our pilot RCT [24]. Staff protocol compliance will be supported through pre-set scripts and checklists, and fidelity checks (Supplement 4).
Adverse events
Participants will be asked to report to study staff, any adverse events resulting from study participation. During each exercise counselling and testing session, participants will be asked about musculoskeletal injury or discomfort. All adverse events will be recorded by study staff.
Data management
All participant data will be entered on REDCap, a secure web-based application designed to support data capture for research studies, and uploaded weekly to UBC TeamShare (see Data Safety). Blood will be stored in a −80c freezer prior to analysis. Five years after publication, all human samples will be disposed of as per UBC policy.
Data monitoring
The data safety and monitoring committee consists of a scientist and physiatrist with content expertise, and a statistician/trials methodologist, external to the trial. This committee will monitor trial progress, adherence and safety. Trial reports will be generated by a statistician unassociated with the study, and will remain confidential to the committee until the trial is ended. All committee recommendations will be shared with the PI. A trial steering committee (chaired by the PI and including site operations managers, a community liaison with lived experience with SCI, and a physiatrist) will monitor daily operations.
Data safety
All data will be stored on UBC’s TeamShare Storage Service, a secure, password-protected interface only accessible to users with UBC credentials. All project computers and tablets are password-protected. Only the PI and one Co-I have access to directly identifiable information. The trial dataset, purged of directly identifying information, will be made available to all Co-Is and selected researchers/students.
Ethics and dissemination
The UBC Clinical Research Ethics Board approved the protocol. Dissemination/KT strategies will be determined with stakeholders and tailored to specific audiences (e.g., articles on SCI organization websites, professional workshops, online training modules). Scientific audiences will be reached through publications in discipline-relevant journals, describing findings in accordance with relevant reporting standards. Authorship follows ICMJE guidelines. Project documentation (e.g., manuals, standardized operating procedures) and coded, non-identifiable participant outcome data will be shared through DOI-supported open science frameworks.
In summary, the EPIC-SCI pragmatic RCT will provide essential data on the effectiveness of exercise, prescribed according to international SCI guidelines and implemented in real-world settings, to alleviate chronic pain in adults with SCI. The trial will also shed light on the pathways, psychosocial and economic outcomes of exercise-induced changes in SCI pain. EPIC-SCI has the potential to provide information to improve pain treatment and, in turn, to improve the lives of hundreds of thousands of people living with chronic SCI pain.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed. De-identified data will be made available upon publication of the datasets, using an open-source web application that supports DOI (e.g., Open Science Framework, Dataverse).
Change history
15 July 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41393-020-0519-2
References
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J pain (Lond, Engl). 2015;19:5–14.
Finnerup NB, Baastrup C. Spinal cord injury pain: mechanisms and management. Curr pain headache Rep. 2012;16:207–16.
Mann R, Schaefer C, Sadosky A, Bergstrom F, Baik R, Parsons B, et al. Burden of spinal cord injuryrelated neuropathic pain in the United States: retrospective chart review and cross-sectional survey. Spinal Cord. 2013;51:564–70.
Tran J, Dorstyn DS, Burke AL. Psychosocial aspects of spinal cord injury pain: a meta-analysis. Spinal Cord. 2016;54:640–8.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Guy SD, Mehta S, Casalino A, Côté I, Kras-Dupuis A, Moulin DE et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: recommendations for treatment. Spinal Cord. 2016; 54;S14–23.
Henwood P, Ellis JA. Chronic neuropathic pain in spinal cord injury: the patient’s perspective. Pain Res Manag. 2004;9:39–45.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J, et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord. 2003;41:34–43.
Mulroy SJ, et al. Strengthening and optimal movements for painful shoulders (STOMPS) in chronic spinal cord injury: a randomized controlled trial. Phys Ther. 2011;91:305–24.
Curtis KA, Tyner TM, Zachary L, Lentell G, Brink D, Didyk T, et al. Effect of a standard exercise protocol on shoulder pain in long-term wheelchair users. Spinal Cord. 1999;37:421–9.
Middaugh S, et al. EMG biofeedback and exercise for treatment of cervical and shoulder pain in individuals with a spinal cord injury: a pilot study. Top Spinal Cord Inj Rehabil. 2013;19:311–23.
Norrbrink C, Lindberg T, Wahman K, Bjerkefors A. Effects of an exercise programme on musculoskeletal and neuropathic pain after spinal cord injury-results from a seated double-poling ergometer study. Spinal Cord. 2012;50:457–61.
Todd KR, Martin Ginis KA. An examination of diurnal variations in neuropathic pain and affect, on exercise and non-exercise days, in adults with spinal cord injury. Spinal Cord Ser Cases. 2018;4:94.
van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey V, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: An update and a new guideline. Spinal Cord. 2018;56:308–21.
Rosety-Rodriguez M, Camacho A, Rosety I, Fornieles G, Rosety MA, Diaz AJ, et al. Low-grade systemic inflammation and leptin levels were improved by arm cranking exercise in adults with chronic spinal cord injury. Arch Phys Med Rehabilitation. 2014;95:297–302.
Zhang JM, An J. Cytokines, inflammation and pain. Int Anesthesiol Clin. 2007;45:27–37.
Leung L, Cahill CM. TNF-α and neuropathic pain: a review. J Neuroinflammation. 2010;7:27.
Naugle KM, Ohlman T, Naugle KE, Riley ZA, Keith NR. Physical activity behavior predicts endogenous pain modulation in older adults. Pain. 2017;158:383–90.
Burke SM, Tomasone JR, Scime NV, Ma JK, Harden SM, Wolfe DL, et al. Physical activity self-management interventions for adults with spinal cord injury: part 2 – exploring the generalizability of findings from research to practice. Psychol Sport Exerc. 2018;37:286–95.
Hoekstra F, McBride CB, Borisoff J, Fetterly M-J, Ginis S, Latimer-Cheung AE et al. Translating the international scientific spinal cord injury exercise guidelines into community and clinical practice guidelines: a Canadian evidence-informed resource. Spinal Cord. 2020: https://doi.org/10.1038/s41393-019-0410-1.
Ma JK, Cheifetz O, Todd KR, Chebaro C, Phang SH, Shaw RB et al. Co-development of a physiotherapist-delivered physical activity intervention for adults with spinal cord injury. Spinal Cord. 2020: https://doi.org/10.1038/s41393-020-0422-x.
Ribeiro Neto F, Guanais P, Dornelas E, Coutinho ACB, Costa RRG. Validity of one-repetition maximum predictive equations in men with spinal cord injury. Spinal Cord. 2017;55:950–6.
Ma JK, West CR, Martin Ginis KA. The effects of a patient and provider co-developed, behavioral physical activity intervention on physical activity, psychosocial predictors, and fitness in individuals with spinal cord injury: a randomized controlled trial. Sports Med. 2019;49:1117–31.
Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International Spinal Cord Injury Pain Classification: part I. Background and description. Spinal Cord. 2012;50:413–7.
Putzke JD, Richards JS, Hicken BL, DeVivo MJ. Interference due to pain following spinal cord injury: important predictors and impact on quality of life. Pain. 2002;100:231–42.
Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB, et al. Pain after spinal cord injury: an evidence-based review for clinical practice and research. Report of the National Institute on Disability and Rehabilitation Research Spinal Cord Injury Measures meeting. J Spinal Cord Med. 2007;30:421–40.
Hill MR, Noonan VK, Sakakibara BM, Miller WC. Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord. 2010;48:438–50.
Hallstrom H, Norrbrink C. Screening tools for neuropathic pain: can they be of use in individuals with spinal cord injury? Pain. 2011;152:772–9.
Albu S, Gomez-Soriano J, Avila-Martin G, Taylor J. Deficient conditioned pain modulation after spinal cord injury correlates with clinical spontaneous pain measures. Pain. 2015;156:260–72.
Gruener H, Zeilig G, Laufer Y, Blumen N, Defrin R. Differential pain modulation properties in central neuropathic pain after spinal cord injury. Pain. 2016;157:1415–24.
Martin Ginis KA, Latimer AE, McKecknie K, Ditor DS, McCartney N, Hicks AL, et al. Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabilitation Psychol. 2003;48:157–64.
Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006;123:231–43.
Yarnitsky D, Arendt-Nielsen L, Bouhassira D, Edwards RR, Fillingim RB, Granot M, et al. Recommendations on terminology and practice of psychophysical DNIC testing. Eur J pain (Lond, Engl). 2010;14:339.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Eerden S, Dekker R, Hettinga FJ. Maximal and submaximal aerobic tests for wheelchair-dependent persons with spinal cord injury: a systematic review to summarize and identify useful applications for clinical rehabilitation. Disabil Rehabil. 2018;40:497–521.
Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials, 1st edn, New York: Oxford University Press; 2007.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160:19–27.
Chen Y, Heinemann AW. Current research outcomes from the spinal cord injury model systems. Arch Phys Med Rehabil. 2016;97:1607–9.
Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1774–81.
Acknowledgements
We would like to acknowledge the support of research coordinator Adrienne Sinden in preparing the manuscript. We would like to acknowledge Joan Úbeda-Colomer, Emily Giroux, and Miranda Dinwoodie for their support in preparing supplementary files.
Funding
The Project Grant Program (Spring 2019) of the Canadian Institutes of Health Research (CIHR) funded this project (Grant # PJT-165903) https://cihr-irsc.gc.ca. CIHR had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
KMG, JWvdS and KRD drafted sections of this manuscript. FH compiled all OSF and supplementary materials, and checked the manuscript for conformity to SPIRIT reporting guidelines. All other authors (JCD, SG, MEK, JLKK, JPL, JS, AT, CRW) substantially contributed to the conception or design of this study and drafted sections of this paper or reviewed it critically for important intellectual content. All authors approved the final version of this manuscript for publication; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
MEK has received consulting fees from Biogen and participated in Advisory Boards and/or Satellite Symposia of Biogen Inc. for studies related to Multiple Sclerosis. All other authors declare they have no conflict of interest.
Ethics
This study protocol has been approved by the Clinical Research Ethics Board (CREB) of the University of British Columbia. All participants will provide written informed consent before taking part in the study (also see “Eligibility screening and informed consent” above). The CREB will review any protocol modifications, followed by updating the trial registration. Protocol and informed consent modifications will be made available using Open Science Framework (https://osf.io/). Informed consents will be revisited with enrolled participants if protocol modifications occur. The CREB will review any requests for use of data in an ancillary study beyond the scope of this RCT that are not covered by the original ethics application.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Martin Ginis, K.A., van der Scheer, J.W., Todd, K.R. et al. A pragmatic randomized controlled trial testing the effects of the international scientific SCI exercise guidelines on SCI chronic pain: protocol for the EPIC-SCI trial. Spinal Cord 58, 746–754 (2020). https://doi.org/10.1038/s41393-020-0478-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0478-7
This article is cited by
-
The effects of active upper-limb versus passive lower-limb exercise on quality of life among individuals with motor-complete spinal cord injury
Spinal Cord (2022)
-
The effects of a high-fat/high-carbohydrate meal on leukocyte populations in adults with chronic spinal cord injury
Spinal Cord Series and Cases (2021)
-
Commentary on “A pragmatic randomized controlled trial testing the effects of the international scientific SCI exercise guidelines on SCI chronic pain: protocol for the EPIC-SCI trial”
Spinal Cord (2020)