Abstract
Study Design
A cross-sectional study.
Objectives
To examine psychometric properties, including internal consistency, construct validity, and test–retest reliability, of the Thai version of the International Spinal Cord Injury (ISCI) Quality of Life Basic Data Set (QoL-BDS).
Setting
Outpatient rehabilitation clinic, urodynamic clinic, and rehabilitation ward at Maharaj Nakorn Chiang Mai Hospital.
Methods
Participants were assigned to complete two assessment tools, the Thai version of QoL-BDS which consisted of three single items on satisfaction with life as a whole, physical health and psychological health, and the Thai version of the World Health Organization Quality of Life instrument (WHOQOL-BREF) completed by face to face interview. After 2 weeks, the participants were evaluated the QoL-BDS again via telephone interviewing to assess test–retest reliability.
Results
One hundred and thirty people with spinal cord injury (SCI) were included in the study. Of all participants, 103 people had a traumatic SCI. The mean (SD) age was 43.0 (13.1) years and the median (IQR) time after SCI was 7.5 (1–14) years. The Thai version of QoL-BDS had good internal consistency (Cronbach’s alpha = 0.89), fair to good construct validity (Spearman’s rank correlation coefficient of 0.43–0.57, p < 0.01) and good to excellent test–retest reliability (Intraclass correlation coefficient of 0.73–0.86).
Conclusions
The Thai version of QoL-BDS had acceptable psychometric properties. As it is concise, QoL-BDS should be encouraged in healthcare providers to investigate QoL in people with SCI, especially in middle-income countries.
Similar content being viewed by others
Introduction
People with spinal cord injury (SCI) usually have impairments of body function, resulting in limitations of activities and participation [1], and in some cases, a reduction of quality of life (QoL) [2]. QoL affects functional statuses and complications of people with SCI, and vice versa [3]. Therefore, it is important to have a valid and reliable tool to assess QoL in people with SCI. Although the World Health Organization Quality of Life-BREF scale (WHOQOL-BREF) is generally used and well-accepted tool to evaluate QoL [4, 5], it contains many questions (26 items) and requires such a long time to complete (10.6–15.3 min) [6], causing unfeasibility for healthcare providers to use in the routine practices especially in low-middle income countries, which have limited personnel and time resources.
In the year 2012, Charlifue and colleagues published the International Spinal Cord Injury Quality of Life Basic Data Set (QoL-BDS) to decrease diversity, discrepancy and create the same standard and direction when assessing QOL in people with SCI [7]. This data set is a part of the International Spinal Cord Injury (ISCI) Data set project which was developed by the International Spinal Cord Society (ISCoS) and the American Spinal Injury Association (ASIA) [8].
QoL-BDS contains of three questions, assessing satisfaction in three aspects of the interviewee’s life, which are the satisfaction of life as a whole, the satisfaction of physical health and the satisfaction of psychological health. Since it contains only three questions, it was expected to take only a few minutes to complete [9], which is more feasible for using in the clinical situation.
Previous studies reported that QoL-BDS questionnaire had an acceptable floor and ceiling effects [9, 10], good internal consistency [9, 10], fair to good construct validity [9, 10], and acceptable test–retest variability [11]. However, all studies were mostly conducted in high-income countries and no single study has investigated the psychometric properties of QoL-BDS in low- or middle-income countries with different socioeconomic contexts. For example, compared with those from high-income countries such as the USA or Netherland, people with SCI in Thailand have shorter post-acute rehabilitation admission, lower medical and social supports from the government [12,13,14].
Therefore, this study aimed to translate QoL-BDS into the Thai version and evaluate its psychometric properties, namely its floor and ceiling effects, internal consistency, construct validity, and test–retest reliability before using this questionnaire to evaluate Thai people living with SCI in routine practice. Also, the authors aim to investigate the QoL status and its associated demographic and SCI-related medical factors to acknowledge the details about QoL in people with SCI in Thailand.
Methods
Developing the Thai version of QoL-BDS
Permission was obtained from Professor F Biering-Sorensen, one of the members of the QoL-BDS developmental committee via electronic mail to translate QoL-BDS into Thai. Then, an initial translation to the Thai language was conducted by two authors who had experience in the rehabilitation of people with SCI (SP and ST).
After that, a back-translation from Thai to English by a linguistic expert, who was blinded to the original English version of QoL-BDS. All translation processes complied with the recommendations for the translation and reliability testing of ISCI Data Sets [15]. The Thai version of the QoL-BDS is in Supplementary Appendix 1.
Participants
The authors included people with chronic (more than 1 year) traumatic and non-traumatic SCI, who attended our outpatient rehabilitation clinic, urodynamic clinic, as well as were admitted for a yearly check-up and going to be discharged from our rehabilitation ward at Maharaj Nakorn Chiang Mai Hospital between August 2017 and 2018 were included.
Other inclusion criteria were age over 18-year old, minimum education of completed elementary school and had an ability to read and understand the Thai language. Having a history of any diseases affecting cognitive function was considered as an exclusion criterion. The sample size was calculated using Bonett and Wright’s formula [16], resulting in the number of participants of 130.
After informed consent and in order to evaluate the validity of QoL-BDS questionnaire, the QoL-BDS and WHOQOL-BREF questionnaires were administered to participants through a face-to-face interview by the same rater on the same day. The interviewer (LS) read the questions out and asked the participants to answer. The participants rated the score of each item of the QoL-BDS and WHOOQOL-BREF by themselves and told their answers to the interviewer for recording. Two weeks later, participants were repeatedly interviewed via telephone by the same author (LS) who read the details of the QoL-BDS questionnaire. The participants rated the score of each item of the QoL-BDS by themselves and told their answers to the interviewer for recording.
Assessment tools
Demographic and SCI-related medical data (i.e., age, sex, duration of injury, level of injury, and AIS) were collected by using the ISCI core data set [17, 18]. QoL data were collected by using QoL-BDS and WHOQOL-BREF; both were in the Thai version. QoL-BDS containes three questions assessing the individual’s satisfaction towards life as a whole, physical health and mental health. The time frame of QoL-BDS covers the past four weeks from the interview. The score of each item ranges from 0 (completely unsatisfied) to 10 (completely satisfied) [7]. WHOQOL-BREF was translated into the Thai version [19]. The psychometric properties of the Thai version have already been tested [19, 20]. WHOQOL-BREF consists of 26 questions evaluating the QoL in the time frame of two weeks before interviewing. Each question has five options, ranging from 1 to 5, in which a higher score represents a higher quality of life. WHOQOL-BREF comprises four components of quality of life; physical part (question No. 2–4, 10–12, and 24), psychological part (question No. 5–9 and 23), social relationship (question No. 13, 14, and 25) and environment (question No. 15–22). Also, question number 1 and 26, which are not included in any component of QoL previously mentioned, indicate overall status of QoL. The social relationships and the environmental component of WHOQOL-BREF were not used since no component from QoL-BDS is related to them.
Analytical methods
Statistical analyses were performed using SPSS version 23.0 for Windows (SPSS Inc., Chicago, IL, USA). A p-value of <0.05 was considered statistically significant. For descriptive statistics, categorical variables were described using percentages of their frequency. Normally distributed numerical variables were presented using arithmetic means and standard deviations (S.D.). Non-normally distributed numerical variables were presented using median and interquartile range (IQR).
- Psychometric properties of QoL-BDS questionnaire
- A floor and a ceiling effect
A floor effect was determined by a percentage of participants who answered with the lowest score (0 for QoL-BDS questionnaire) and a ceiling effect by a percentage of participants who answered with the highest score (10 for QoL-BDS questionnaire). These effects represent a limitation of the questionnaire, which could not furtherly measure more variance in the minimum and maximum scale. In this study, a threshold of 15% was used to determine the significance level of the floor or ceiling effects [21].
- Internal consistency
Cronbach’s alpha coefficient was used to determine the internal consistency of QoL-BDS. Internal consistency was considered “acceptable” if Cronbach’s alpha coefficient was at least 0.70, “good” if at least 0.80, and “excellent” if at least 0.90 [22].
- Construct validity
Construct validity was assessed by determining the concurrent validity between the QoL-BDS and the total score of WHOQOL-BREF. Spearman’s rank correlation coefficient (r) was used to find construct validity between QoL-BDS and WHOQOL-BREF questionnaires since the QoL-BDS questionnaire contained ordinal items.
QoL-BDS consisted of three questions, whereas WHOQOL-BREF consisted of four domains and two questions for the overall status of QoL. Therefore only the components in common to the two questionnaires were used, namely, the satisfaction towards life as a whole question of QoL-BDS and the total overall QoL status domain of WHOQOL-BREF, the satisfaction of physical health question of QoL-BDS and the total score of the physical health domain of WHOQOL-BREF and the satisfaction of psychological health question of QoL-BDS and the total score of the psychological health domain of WHOQOL-BREF. The levels of correlation was determined using the following criteria: r ≥ 0.75, excellent correlation; 0.50 < r < 0.75, good correlation; 0.25 < r < 0.50, fair correlation; r < 0.25, poor correlation or no correlation [22].
- Test–retest reliability
The intraclass correlation coefficient (ICC) was used to find test–retest reliability. The level of correlation comparing ICC between the results of QoL-BDS on the first and the second (after two weeks) assessment was acceptable if the ICC was ≥0.7 [22].
- Factors associated with QoL-BDS scores
Causes of injury were dichotomized into non-traumatic or traumatic SCI. Time since injury was categorized into <10-year, 10–20 year, and >20-year groups. The severity of injury was categorized into four groups according to the advisory guidelines of the International Spinal Cord Society (ISCoS) [17]. They were (1) C1–C4 tetraplegia AIS A, B, C; (2) C5–C8 tetraplegia AIS A, B, C; 3) paraplegia AIS A, B, C; and 4) tetraplegia and paraplegia AIS D.
Differences of parameters among groups were compared using an independent t-test or one-way analysis of variance test (ANOVA) followed by post-hoc least significant difference (LSD) analysis.
Results
Demographic SCI-related medical parameters
One hundred and thirty individuals with SCI were recruited. Ninety-five participants (73%) were males. The mean (SD) age was 43.0 (13.1) years and the median (IQR) time after SCI was 7.5 (1–14) years. Most of the participants were diagnosed as the group A, B, and C paraplegia (64%, n = 83). Demographic and SCI-related medical data were presented in Table 1.
Psychometric properties of QoL-BDS questionnaire
All participants completed the interviews, and were assessed twice with QoL-BDS and once with WHOQOL-BREF. All participants fully answered all the questions of QoL-BDS and WHOQOL-BREF. Table 2 shows the scores including the floor and the ceiling effects on all items of QoL-BDS from the first and the second assessments. The floor and the ceiling effects of QoL-BDS were <15% (3.8% for the floor and 14.6% for the ceiling effect), which was an acceptable level. Focusing on the internal consistency of QoL-BDS, the Cronbach’s alpha coefficient was 0.89, which was at an excellent level.
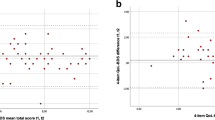
Table 3 shows the construct validity between each group of questions of QoL-BDS and the selected component of WHOQOL-BREF. All correlations were statistically significant (p < 0.05) and were at a moderate to good level, in which the range of Spearman’s rho correlation coefficient was between 0.43 and 0.57. On an analysis of the matched components, a correlation between the satisfaction of psychological health component of QoL-BDS and the overall health component of WHOQOL-BREF had the strongest correlation coefficient (r = 0.57), whereas a correlation between the satisfaction of physical health component of QoL-BDS and the physical health domain of WHOQOL-BREF had the weakest correlation coefficient (r = 0.43).
Table 2 shows the test–retest reliability. The ICC of each question of QoL-BDS between the first and the second interview were at a good to excellent level. They were 0.73 (95% CI of 0.66–0.79) for satisfaction of life as a whole, 0.86 (95% CI of 0.81–0.90) for satisfaction towards physical health and 0.83 (95% CI of 0.83–0.88) for satisfaction towards psychological health.
Factors associated with QoL-BDS scores
Table 4 compares the QoL-BDS score among people with different baseline characteristics. It was found that the people with SCI who were older (age ≥ 50-years old) had significantly lower QoL-BDS scores in the physical and mental health domain than those who was younger (age < 50-years old) (5.7 vs 6.7, p = 0.031 and 6.2 vs 7.2 p = 0.025, respectively; independent t-test). Besides, the people with non-traumatic SCI had significantly lower QoL-BDS in the mental health domain than the people with traumatic SCI (6.6 vs 5.4, p = 0.019, independent t-test). There was also a significant difference in QoL-BDS scores in the mental health domain among participants who had a different duration of injury (p = 0.04, one-way ANOVA). For instance, participants who lived with SCI <10 years had significantly lower QoL-BDS score in the mental health domain than those who lived with SCI between 10 and 20 years and who had SCI for more than 20 years (p = 0.046 and p = 0.033, respectively; post-hoc LSD test). However, no significant difference was found among people with different severity of the injury.
Discussion
This study aimed to test the Thai version of QoL-BDS on its psychometric properties among people with SCI. It revealed acceptable floor and the ceiling effects on the Thai version of QoL-BSD (3.8% and 14.6%, respectively) with noticeable ceiling of 14.6% from the satisfaction with mental health items. A relatively high-ceiling effect indicated that some participants probably had QoL more than the scale of the QoL-BDS questionnaire could measure. This might results from an interview effect whereby participants were more likely to overrate in their responses when being interviewed than if the questionnaire had been self administered. Owing to the necessity to reassess the test–retest reliability via a telephone call, the authors decided to use an interview instead of a self-administrated questionnaire to make our data collecting method consistent. In our study, the floor and ceiling effects were comparable to those from the study by New et al. [10], being considered at an acceptable level (<15%).
The internal consistency of this study was 0.89, at a good level, which was also comparable with the results from the study by New et al. [10] and by Post et al. [9], with the internal consistency of 0.84 and 0.81, respectively. The construct validity determined by correlating the Thai version of QoL-BDS with WHOQOL-BREF was between 0.43 and 0.57, which was at a fair to good level. The previous tudy by New et al. [10] demonstrated that the correlation between QoL-BDS and WHOQOL-BREF was between 0.40 and 0.88, again at a fair to excellent level. The lower range of correlations in this study might be due to a difference in reference questionnaire. In both studies by Post et al. [9] and New et al. [10], a single question in WHO-QOL or WHOQOL-BREF questionnaire was used as a reference, but in this study, the average score of a set of questions from a whole WHOQOL-BREF questionnaire was referenced. Therefore, a comparison was performed between one item of a measurement and a whole set of a measurement which was also a gold standard for evaluating QoL. Despite this incompatibility, it was still noteworthy that the construct validity was still at least in the fair range. It was noted that Post and colleagues had compared QoL-BDS life as a whole with WHOQOL item 1, QOL-BDS physical health with WOQOL item 2, and QOL-BDS mental health with WHOQOL item 26. Another possible cause of the under-expected correlation between QoL-BDS and WHOQOL-BREF was the difference in the period of time when each questionnaire was applied to assess the QoL The QoL-BDS was intended to investigate QoL in the last four weeks whereas the WHOQOL-BREF in the last two weeks. Any event occurring between the last four and two weeks might affect the QoL-BDS score but not the WHOQOL-BREF score.
On a test–retest reliability analysis, it was found that the test–retest reliability of the Thai version of QoL-BDS was between 0.73 and 0.86, which was at an acceptable level. These results were comparable with the results from the study by Post et al. [11] showing the test–retest reliability of 0.66–0.80, which was acceptable. The exact period of time between the first and second assessments of this study and the median time between the first and second assessments in Post’s study was two weeks, which seemed appropriate since it was short enough that people’s symptoms were unlikely to change and long enough that people could not remember their previous answers [22].
The QoL-BDs scores in this study were between 6.4 and 6.9, which were comparable to the results from the study by Post et al. (5.8–6.9) [9] and by New et al. (5.7–6.9) [10]. Previous studies revealed that quality of life in abled-bodied Thais SCI caregivers was not different from those in abled-body Netherlander SCI caregivers [23, 24]. When analyzing on the factors associated with QoL-BDS scores, the authors found that the scores of satisfaction towards physical and mental health of people with SCI who were older than 50-years old were significantly lower than those who were younger than 50-years old, whereas the previous study by New et al. [10] reported no significant correlation between age and QoL-BDS scores. These inconsistent findings might be drawn to the difference in the socioeconomic status of the participants. The people with non-traumatic SCI had significantly lower satisfaction towards physical health scores than people with traumatic SCI, being consistent with results from the study by Migiliorini et al. [2] which might be attributable to the difference in clinical courses between non-traumatic and traumatic SCI. The authors also found that people who lived with SCI <10 years had significantly lower satisfaction towards mental health scores when compared with those >10 years. Due to the fact that having chronic SCI (duration of SCI > 1 year) was one of our inclusion criteria and no recently injured inpatient was included in this study, a weak, but significant, positive correlation was seen between time since the onset of injury and satisfaction towards life as a whole and mental health scores which was consistent with results from the study by New et al. [10]. These results might be caused by a better coping strategy to SCI and SCI-related sequelae over time [25].
No other factor was found to be associated with QoL-BDS scores in this study, although New et al. [10] reported that people who having remunerative work had significantly higher three domains of QoL-BDS scores when compared with those who did not have. However, no data of working status were recorded in this study. The level and severity of the injury were proposed to be a factor determining QoL in people with SCI, but the results were inconsistent [2, 23, 26]. As the assessment tool, QoL-BDS, reflected a subjective, self-report aspect of QoL, it might not be significantly affected by the level and severity of the injury.
There were a few limitations of this study. The exact time it took participants to complete the Thai version of the QoL-BDS questionnaire was not recorded. However, the interviewer (LS) estimated that it took less than five minutes. This was comparable with the estimated time in the study by Post et al. [9] which was 1–3 min. Moreover, although the test–retest reliability was completely assessed, the validity was only partially tested in this study. For instance, comparisons between each item of QoL-BDS and other well-accepted scores such as Hospital Anxiety and Depression Scale (HADS), Mental Health Inventory-5, as well as SCI-Secondary Condition Scale were not performed in terms of construct validity. Besides, further validation studies conducting in low- or middle-income status is still necessary.
The advantage of this study was that the sample size was well-calculated and adequate for determining any significance. It is also the first study investigating all psychometric parameters of the QoL-BDS questionnaire in a single episode. The participants were interviewed by only one interviewer, therefore the results are less susceptible to bias. Importantly, it is the first study evaluating the psychometric properties of QoL-BDS questionnaire to be conducted in a middle-income country. Therefore, given the results of this study show an acceptable validity, reliability, and feasibility of QoL-BDS questionnaire, they should encourage healthcare providers in low- and middle-income countries with limited personnel and time resources to use QoL-BDS in routine practice.
In conclusion, the Thai version of the QoL-BDS questionnaire has good internal consistency, fair to good construct validity and acceptable test–retest validity. Since the QOL-BDS questionnaire is concise and not time consuming to use, it should be promoted for healthcare providers to explore QoL in people with SCI, especially in low- or middle-income countries.
Data archiving
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cieza A, Kirchberger I, Biering-Sorensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the long-term context. Spinal Cord. 2010;48:305–12.
Migliorini CE, New PW, Tonge BJ. Quality of life in adults with spinal cord injury living in the community. Spinal Cord. 2011;49:365–70.
Tulsky DS, Kisala PA, Victorson D, Tate DG, Heinemann AW, Charlifue S, et al. Overview of the Spinal Cord Injury-Quality of Life (SCI-QOL) measurement system. J Spinal Cord Med. 2015;38:257–69.
Hill MR, Noonan VK, Sakakibara BM, Miller WC. SCIRE Research team. Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord. 2010;48:438–50.
Whitehurst DG, Noonan VK, Dvorak MF, Bryan S. A review of preference-based health-related quality of life questionnaires in spinal cord injury research. Spinal Cord. 2012;50:646–54.
Hwang HF, Liang WM, Chiu YN, Lin MR. Suitability of the WHOQOL-BREF for community-dwelling older people in Taiwan. Age Ageing. 2003;32:593–600.
Charlifue S, Post MW, Biering-Sorensen F, Catz A, Dijkers M, Geyh S, et al. International Spinal Cord Injury Quality of Life Basic Data Set. Spinal Cord. 2012;50:672–5.
Biering-Sorensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T, et al. International Spinal Cord Injury Data Sets. Spinal Cord. 2006;44:530–4.
Post MW, Adriaansen JJ, Charlifue S, Biering-Sorensen F, van Asbeck FW. Good validity of the international spinal cord injury quality of life basic data set. Spinal Cord. 2016;54:314–8.
New PW, Tate DG, Forchheimer MB, D’Andrea Greve JM, Parashar D, Post MWM. Preliminary psychometric analyses of the International Spinal Cord Injury Quality of Life Basic Data Set. Spinal Cord. 2019;57:789–95.
Post MWM, Forchheimer MB, Charlifue S, D’Andrea Greve JM, New PW, Tate DG. Reproducibility of the international spinal cord injury quality of life basic data set: an international psychometric study. Spinal Cord. 2019;57:992–8.
Post MW, Nooijen CF, Postma K, Dekkers J, Penninx F, van den Berg-Emons RJ, et al. People with spinal cord injury in the Netherlands. Am J Phys Med Rehabil. 2017;96(2 Suppl 1):S93–5.
Richards C, MacKenzie N, Roberts S, Escorpizo R. People with spinal cord injury in the United States. Am J Phys Med Rehabil. 2017;96(2 Suppl 1):S124–S126.
Kovindha A. People with spinal cord injury in Thailand. Am J Phys Med Rehabil. 2017;96(2 Suppl 1):S120–3.
Biering-Sorensen F, Alexander MS, Burns S, Charlifue S, DeVivo M, Dietz V, et al. Recommendations for translation and reliability testing of International Spinal Cord Injury Data Sets. Spinal Cord. 2011;49:357–60.
Bonett DG, Wright TA. Sample size requirements for estimating pearson, kendall and spearman correlations. Psychometrika. 2000;65:23–8.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International Spinal Cord Injury Core Data Set. Spinal Cord. 2006;44:535–40.
Phungrassami T, Katikarn R, Watanaarepornchai S, Sangtawan D. Quality of life assessment in radiotherapy patients by WHOQOL-BREF-THAI: a feasibility study. J Med Assoc Thai. 2004;87:1459–65.
Sakthong P, Schommer JC, Gross CR, Sakulbumrungsil R, Prasithsirikul W. Psychometric properties of WHOQOL-BREF-THAI in patients with HIV/AIDS. J Med Assoc Thai. 2007;90:2449–60.
McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4:293–307.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42.
Wongsa S, Tongprasert S, Kovindha A. Quality of life of primary caregivers of disabled people with spinal cord injury by using Short Form-36 Questionnaire. J Thai Rehabil Med. 2011;21:28–33.
Lucke KT, Cocia H, Lucke JF. Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res. 2004;13:97–110.
Elfstrom ML, Kreuter M, Ryden A, Persson LO, Sullivan M. Effects of coping on psychological outcome when controlling for background variables: a study of traumatically spinal cord lesioned persons. Spinal Cord. 2002;40:408–15.
Manns PJ, Chad KE. Determining the relation between quality of life, handicap, fitness, and physical activity for persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:1566–71.
Acknowledgements
The authors would like to thank Ms Rodchana Janpueak, a research administrator of Faculty of Medicine, Chiang Mai University, for providing statistical advices, as well as Associate Professor Jakkrit Klaphajone, an associate professor of rehabilitation medicine and an English specialist of Faculty of Medicine, Chiang Mai University, for English proofreading and correction.
Author information
Authors and Affiliations
Contributions
SP designed the research questions, collected and analyzed the data, drafted the manuscript and wrote the final version of the manuscript. LS collected and analyzed the data and drafted the manuscript. TW designed the research questions and commented on the final version of the manuscript. ST designed the research question, collected and analyzed the data and commented on the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand and was in accordance with the current version of the Helsinki Declaration. The study number is REH-2560-04814. The authors certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during all course of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pattanakuhar, S., Suttinoon, L., Wongpakaran, T. et al. The reliability and validity of the International Spinal Cord Injury Quality of Life Basic Data set in people with spinal cord injuries from a middle-income country: a psychometric study of the Thai version. Spinal Cord 58, 1015–1021 (2020). https://doi.org/10.1038/s41393-020-0468-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0468-9
This article is cited by
-
Reciprocal association between pain and quality of life after newly acquired spinal cord injury
Quality of Life Research (2024)
-
Internal consistency and convergent validity of the International Spinal Cord Injury Quality of Life Basic Data Set at discharge from first rehabilitation
Spinal Cord (2022)
-
Longitudinal measurement invariance of the international spinal cord injury quality of life basic data set (SCI-QoL-BDS) during spinal cord injury/disorder inpatient rehabilitation
Quality of Life Research (2022)