Abstract
Study design
Outcome measure item generation and reduction.
Objectives
To develop a patient reported outcome measure (PROM) addressing the impact of neurogenic bowel dysfunction (NBD) on individuals living with traumatic or nontraumatic spinal cord injury (SCI).
Setting
Tertiary rehabilitation center in Toronto, Canada.
Methods
A PROM based on the International Classification of Functioning, Disability and Health (ICF) framework was developed using the following steps: (a) item generation, (b) item refinement through iterative review, (c) completion of items by individuals living with SCI and NBD followed by cognitive interviewing, and (d) further item refinement, item reduction, and construction of the preliminary PROM.
Results
Following initial item generation and iterative review, the investigative team agreed on 55 initial items. Cognitive interviewing, additional revisions, and item reduction yielded an instrument comprised of 35 items; while ensuring at least two items were retained for each of the 16 previously identified challenges of living with NBD following the onset of a SCI. Scoring for the preliminary PROM ranges from 0 to 140.
Conclusions
A preliminary PROM informed by the ICF for assessing the impact of NBD post-SCI has been devised, which can be used to inform clinicians and decision-makers on optimal ways to treat this serious secondary health complication. Future work will assess the validity and clinimetric properties of the PROM.
Similar content being viewed by others
Introduction
Among the many secondary complications following traumatic and nontraumatic spinal cord injury (SCI), those related to neurogenic bowel dysfunction (NBD) are particularly common and have a profound impact on health, well-being, and social participation [1,2,3,4,5,6,7]. Coggrave et al. reported that 98% of community-dwelling individuals with SCI reported at least one bowel-related problem [5]. Specific sequelae of NBD following SCI include impaired gastrointestinal motility and prolonged bowel transit time, loss of continence, increased time requirements for bowel care, pain, and detrimental effects on emotional well-being (e.g., loss of dignity). In studies of individuals living with a SCI, 40–60% of participants report that NBD adversely affects day-to-day activities, lifestyle, and quality of life (QoL) [1,2,3,4,5]. Bowel incontinence specifically has been reported to be the greatest source of social discomfort following SCI [6], and persons with SCI rate the recovery of bowel and bladder function as a priority for cure above issues such as walking or pain management [1, 7]. Despite its prevalence and importance, NBD has been understudied and a recent Cochrane Review concluded, “there is still remarkably little research on this common and, to patients, very significant issue…” [8].
Prior phenomenological (qualitative) studies from the perspective of affected stakeholders (individuals with SCI and support providers) have documented that the impact of NBD on function and participation in societal activities and roles is dependent on a complex interaction between the health condition, the environment, and personal factors [9, 10]. When organized according to the World Health Organization International Classification of Functioning, Disability and Health (ICF), identified concerns fall into the domains of ‘body functions and structures’, ‘activity’, ‘participation’, as well as contextual factors such as ‘environmental factors’ and ‘personal factors’. A recent study found that the impact of NBD on the ‘personal factors’ and ‘environmental factors’ domains (e.g., loss of privacy, lack of independence, emotional distress, economic costs) exceeded its impact on ICF domains such as ‘body functions and structures’ (e.g., loss of volitional control, transit times) [11]. Despite the above, to date clinicians and researchers have largely directed their efforts at addressing the impact of NBD on the ‘body functions and structures’ domain of the ICF.
Future efforts to improve the management of NBD will need to focus increasingly on ICF domains outside of ‘body functions and structures’. It is therefore essential that outcome measures capture the impact of NBD comprehensively and from a broad perspective. Accordingly, the need to improve research in bowel and bladder dysfunction, through the development and validation of appropriate outcome measures for NBD, is a recognized priority in the field [12, 13]. Despite this, there are few condition-specific (neurogenic bowel) outcome measures with established reliability and validity [14]. In addition, none are constructed using the ICF framework as a theoretical foundation.
The purpose of the current study therefore was to develop a patient reported outcome measure (PROM) that comprehensively captures the impact of NBD on QoL among individuals living with SCI by encompassing all ICF domains.
Methods
Guiding principles (theoretical framework)
The investigative team conducted a prior study of individuals with lived experience, which identified concerns related to living with traumatic or nontraumatic SCI and NBD [9]. Concerns spanned the ICF continuum and impacted all domains. To address this, a PROM was developed to provide comprehensive coverage of identified concerns and their accompanying ICF domains using the following steps: (a) item generation, (b) item refinement through iterative review, (c) completion of items by individuals living with SCI and NBD followed by cognitive interviewing, and (d) further item refinement, item reduction, and construction of the preliminary PROM. The research was reviewed and approved by the University Health Network Research Ethics Board. Informed consent was obtained for all study participants.
Item generation
Consistent with recommendations from previously published guidelines for the development of PROMs [15,16,17], a comprehensive bank of candidate items was generated for potential inclusion in a NBD PROM. Items were refined to meet the following criteria: (1) written to elicit responses from predefined response options on a five-point Likert scale; (2) framed using past tense and reported using a 4 week time frame; and (3) written at a sixth-grade reading level.
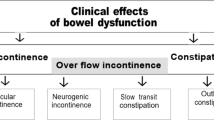
Initial items were derived using content from our prior study which addressed NBD from the perspective of individuals living with SCI [9]. In that study, 16 themes related to the challenges of living with NBD following SCI were identified and categorized within the ICF framework (Fig. 1). Interview excerpts highlighting specific challenges were extracted and used to formulate preliminary items for inclusion in the PROM. Four hundred fifty six excerpts informed the development of the initial 138 items. The items were then categorized according to the 16 previously reported themes [9]. The items were then reviewed by the investigative team and culled to 90 preferred items while ensuring appropriate coverage of each of the 16 themes. The investigative team was comprised of two experienced clinical investigators, a psychosocial researcher, a research associate, and an individual with SCI.
To ensure comprehensive coverage of relevant content areas, we also reviewed the now defunct GI-PRO database [18], as well as outcome measures specific to NBD following SCI including the International SCI Bowel Function Extended Data Set [19], the NBD Score (NBDS) [20] and the SCI-QoL Bowel Management Difficulties (SCI-QoL BMD) item bank [21]. The GI-PRO database was an online library of published English-language gastrointestinal PROMs developed to assist clinicians and investigators. Individual items from all of the above were then consolidated into a database consisting of 1327 items. Following the removal of duplicate items, 1104 distinct items remained. The remaining items were deconstructed into keywords addressing different aspects of NBD, and synonymous terms were merged. Items addressing treatments (specific medications, medical devices, surgeries) or the presence of unrelated medical conditions (e.g. Crohn’s disease, prolapse, diverticulitis) were not used. The content areas represented by keywords were then used to generate 43 distinct items to supplement the 90 items from the initial phase.
The resulting 133 items were then reviewed by the investigative team for item relevance, clarity, and categorization, with the goal of achieving a consensus on a diversity of items while ensuring adequate coverage of the 16 previously identified challenges related to living with NBD following SCI. Items were culled if they were out of scope, similar to other items, multidimensional, or difficult to score within a four week period. Following multiple iterations and consensus building, the 133 items were refined, reworded, and reduced to 55 items. The 55 retained items ensured that each of the 16 challenges had at least three representative items with the exception of diet and travel (for which the committee agreed only two items provided sufficient coverage).
Cognitive interviewing, item refinement/reduction, and PROM construction
The 55 items were then subjected to cognitive interviewing. Cognitive interviewing is an approach to identify problematic items and inform rewording or other required revisions. The methods described by Willis [22, 23] and the PROMIS project [15] were employed to assess how participants process and respond to questions. The interviewer employed a retrospective verbal probing technique. Using this approach, five individuals living with traumatic or nontraumatic SCI and NBD completed a paper and pencil questionnaire and were subsequently probed for the reasoning behind question interpretation and answering. Participants were previous University Health Network-Toronto Rehabilitation Institute (UHN-TRI) patients who agreed to be contacted for the purpose of research studies. Probes were open-ended and attempted to identify sources of error including reading (interpretation), instructions, clarity, assumptions, knowledge/memory, sensitivity/bias, and response categories.
Following transcription of interviews, each questionnaire item was appended with participant responses and sent to the investigative team. Based on review and assessment of the participant responses, minor changes in item phrasing were incorporated when needed. Problematic items were deleted from the item bank. Through this process, the 55 items were further reduced to 35 items while ensuring at least two items were retained for each of the 16 challenges. Item removal was due to similarity to other items (12 items), varied interpretation from participants (6 items), addressed a very specific symptom (1 item), and poor suitability for a 4 week time frame (1 item). The 35 items that emerged formed the preliminary instrument.
Questionnaire (PROM) completion
One hundred thirty eight participants were recruited to complete the preliminary instrument using an existing database of patients from UHN-TRI’s spinal cord rehabilitation program who had previously expressed an interest in participating in research. Participant inclusion criteria included [1] diagnosis of traumatic or nontraumatic SCI of any severity and duration and [2] the ability to speak and understand English. While information on injury severity (e.g., American Spinal Injury Association Impairment Scale grade) is not available, individuals in the research database are representative of individuals who have received care at our tertiary regional rehabilitation center. The rehabilitation center serves a large geographic catchment area.
Potential study subjects were mailed a description of the study along with an invitation to participate. Due to the high prevalence of NBD among individuals with SCI [2, 5] and the desire to capture individuals along the entire continuum of injury severity, no explicit criterion for NBD was included. Initial contact was via electronic mail (n = 289) or physical mail (n = 662). Interested participants were offered the opportunity to complete the preliminary PROM online or alternatively by mailed hard copy. To limit questionnaire completion to invited participants with confirmed traumatic or nontraumatic SCI, potential participants were provided invitation codes that required validation prior to questionnaire completion.
Statistical analysis
To maximize data retention, missing responses were imputed with the median response for the item (total five data points imputed). One participant responded to all the questionnaire items with the same response and was excluded from the analysis. The level of injury was ascertained using questions which clarified anatomical areas with clinical weakness, including hand, arm, trunk, and leg weakness (cervical), trunk and leg weakness (thoracic), leg weakness (lumbar), bowel and bladder dysfunction only (sacral). Participants were categorized as tetraplegic if they endorsed cervical involvement; otherwise, they were categorized as paraplegic. SCI-PROBE scores (ICF domains and individual items) were compared across demographic and injury-related variables and analyzed for significant differences using the Mann–Whitney test with Bonferroni correction. Spearman correlation coefficients were calculated to assess the relationships between variables. Statistical analyses were completed using SAS 9.2 (SAS Institute Inc., Cary, NC).
Results
The development process yielded a novel PROM, the Spinal Cord Injury Patient Reported Outcome Measure of Bowel Function and Evacuation (SCI-PROBE) (see Supplementary materials). The SCI-PROBE is comprised of 35 items and provides representative coverage of the five ICF domains—(1) activity, (2), body function and structures (3), environmental factors (4), participation, and (5) personal factors; as well as previously identified challenges related to living with NBD following SCI. Items of the SCI-PROBE employ a five-point Likert scale (0–4), with higher ratings representing higher impact. Two ‘satisfaction’ questions are scored inversely due to the higher ratings representing lower impacts. Five items related to intimate relationships, vocation, and caregiver assistance incorporate a ‘not applicable’ option; scored 0 (no impact). The SCI-PROBE has a minimum score of 0 and a maximum score of 140. Subscales for each ICF domain were also calculated.
Scoring characteristics and distribution
Following development, 138 participants completed the PROM; 30 in paper format and 108 online. Cohort demographics are summarized in Table 1. Participants had an average age of 56.9 ± 17.1 years and were predominantly male (62%) with traumatic etiology (65%) and paraplegia (62%). Using mobility aides as a proxy for injury severity and accompanying impairments, the use of specific aides was as follows: 19.6% no aides, 24.6% cane(s), 5.8% crutches/walking poles, 9.4% walker, 29.0% manual wheelchair, 8% power wheelchair, and 3.6% not specified.
The median composite SCI-PROBE score was 40 (IQR 27–64, range 4–112). Scores for individual items are summarized in Table 2. All individual items had score ranges from 0 to 4. Median composite scores were similar for men (median 38, IQR 26–63) and women (median 45, IQR 29–64) (p > 0.05). There were no significant gender differences for individual items or ICF domains. Median composite scores were similar for traumatic (median 41, IQR 32–67) and nontraumatic etiologies (median 34, IQR 18.5–62) (p > 0.05). Similarly, there were no significant etiology differences observed for individual items or ICF subscales. There was a very weak inverse relationship with age (ρ = −0.20; p = 0.02). Composite SCI-PROBE scores were similar for persons with tetraplegia (median = 38, IQR 32–68) and paraplegia (median 44, IQR 23–62) (p > 0.05) (Fig. 2). Individuals with tetraplegia scored higher for the ‘dependent’ variable (median 1, IQR 0–3) compared to individuals with paraplegia (median 0, IQR 0–0) (p = 0.0008).
To explore the relationship between impairment severity and the SCI-PROBE, mobility was used as a proxy and ambulators (no aids, canes, poles, walkers; n = 82) were compared to wheelchair users (manual, power; n = 51) (Table 3). While there were no significant differences for composite SCI-PROBE scores between ambulators (median 38, IQR 24–63) and wheelchair users (median 48, IQR 35–68) (p = 0.076), significant differences were observed for the ‘environmental factors’ ICF domain with wheelchair users exhibiting higher impact scores (median 3, IQR 2–7) compared to ambulators (median 1, IQR 0–3) (p = 0.0008). Individual items also demonstrated significant differences between wheelchair users and ambulators. For the ‘dependent’ variable, wheelchair users demonstrated a higher impact score (median 1, IQR 0–4) than ambulators (median 0, IQR 0–0) (p < 0.0001). Compared to ambulators, wheelchair users also had higher scores for the ‘CaregiverTime’ (median 0, IQR 0–2 vs. median 0, IQR 0–0) (p < 0.0001) and ‘CaregiverGood’ (median 0, IQR 0–2 vs. median 0, IQR 0–0) variables (p = 0.0002) respectively. Wheelchair users also had higher impact scores for the ‘NeedtoPlan’ variable compared to ambulators (median 2, IQR 1–4 vs. median 1, IQR 0–2) (p = 0.0014). Decreased ‘Premonition’ had a greater impact on ambulators (median 4, IQR 3–4) compared to wheelchair users (median 3, IQR 0–4) (p = 0.0003).
Discussion
When assessing the impact of NBD following SCI, as well as evaluating the efficacy of NBD interventions, it is important to take into account the issues and concerns of affected stakeholders. These concerns span the ICF domains of ‘body functions and structures’, ‘activity’, ‘participation’, ‘environmental factors’ and ‘personal factors’ [9, 10]. In response, the investigative team developed the SCI-PROBE; a novel PROM which was conceptualized and developed to comprehensively capture the impact of NBD following SCI across the ICF continuum. As recommended for PROM development, qualitative interviewing was performed as a first step [24]. Initial item construction was then guided by feedback solicited directly from impacted stakeholders using qualitative (phenomenological) interviews [9, 10]. Phenomenology is intended to describe phenomena as experienced by the individual.
Pilot completion of the SCI-PROBE by a cohort of individuals with traumatic and nontraumatic SCI (n = 138) revealed a representative and broad range of composite scores (Fig. 2). No significant differences in SCI-PROBE composite scores were found for neurological level, gender, or etiology. A weak inverse relationship was observed with age. As expected, the severity of impairments contributed to the impact of NBD following SCI. Individuals with tetraplegia and wheelchair users both demonstrated greater dependence for bowel care. Compared to ambulators, wheelchair users were also impacted to a greater degree by available caregiver time and quality. Wheelchairs users also had a greater requirement to plan for bowel care. Conversely, impaired premonition impacted ambulators to a greater degree.
Compared to the SCI-PROBE, alternative outcome measures largely capture the impact of NBD on the ‘body functions and structures’ domain of the ICF (e.g., loss of volitional control, transit times). Given the importance of comprehensive ICF coverage, this comparatively narrow focus is an important limitation. Pires et al. recently studied the impact of NBD after SCI using the ICF [11]. As opposed to ‘body functions and structures’ domain, the greatest impact was in fact in the ‘personal’ and ‘environmental’ domains, with 47% of the patients reporting loss of privacy, 45% requiring assistance for bowel management, 45% reporting feelings of frustration, anxiety, of depression, and 39% endorsing increased economic costs. Additional studies have reported similar findings. Up to half of individuals with SCI are dependent on others for toileting [2]. In a study of individuals with SCI who had undergone stomal surgery (ileostomy or colostomy), 15% of participants undertook the procedure due to difficulties in procuring appropriate bowel care at home [25].
Impactful interventions will therefore likely expand beyond traditional medical interventions and include policy and societal change. Potential examples include the increased availability, reliability, and effectiveness of supports (e.g., personal support workers, caregivers), flexible work and education schedules that accommodate bowel requirements, and subsidizing the cost of required medical supplies and equipment. The above has implications for health care providers, policy makers, and researchers. Accordingly, outcomes need to capture the impact of NBD across ICF domains. A comprehensive PROM will facilitate the future evaluation of clinical interventions intended to reduce the impact of NBD on individuals living with SCI.
Recent reviews have summarized the relative limitations of current outcome measures for bowel dysfunction [14, 18, 26]. Methodological quality of outcome measures has generally been rated poor [18], with few having established reliability or validity for SCI [14]. In addition, the majority are not condition specific. Measures such as the NBDS are SCI-specific but focus predominantly on the ‘body functions and structures’ domain of the ICF [20]. The NBDS is also targeted to health care professionals and researchers; and has been incorporated into the International SCI Bowel Function Basic Dataset [27]. The International Bowel Function Extended SCI Data Set [19] incorporates three broad items addressing lifestyle alteration and QoL, but inter-rater reliability is poor to moderate [28]. There is therefore an ongoing need for complementary outcome measures which incorporate the experience of living with SCI and NBD, and in particular capture the impact of NBD on ICF domains such as ‘activities’, ‘participation’, ‘environmental factors’ and ‘personal factors’.
Recently, Tulsky et al. employed rigorous methodology to develop the SCI-QoL Bowel Management Difficulties Items Bank [21]. This instrument is comprised of 26 items and is intended to measure the impact of NBD on QoL. While there is overlap in the areas assessed by the SCI-PROBE and the SCI-QoL Bowel Management Difficulties Items Bank, it is unclear if the latter provides comprehensive coverage of ICF. As an example, the SCI-QoL Bowel Management Difficulties Items Bank does not address issues such as loss of privacy, required assistance, or financial impact, which have been identified as important to stakeholders [9, 11].
An advantage of the SCI-PROBE is its comprehensive coverage of ICF domains. As a result, the SCI-PROBE can assess the efficacy of interventions which target issues extending beyond the ‘body functions and structures’ domain (e.g., emotional health, financial costs, need for assistance). In this way, the SCI-PROBE can facilitate the future evaluation of clinical interventions, promote research activity in this important area, and ultimately improve the provision of services, treatment, and rehabilitation related to NBD. The SCI-PROBE, however, still requires further development and refinement. The current version of the SCI-PROBE is intended primarily for research; specifically, to measure the relative efficacy of interventions intended to reduce the impact of NBD on affected individuals. Time requirements will likely preclude its use in daily clinical practice. Other measures will be required to fill this gap. In addition, the clinical importance of corresponding scores requires further study.
Future longitudinal cohort studies are therefore planned to determine concurrent validity, responsiveness to change, relative sensitivity to change, and comparative utility by comparing the SCI-PROBE to other existing measures. This includes determining if synergies can be achieved by using a combination of measures. These studies will also provide additional insight into the clinical implications of specific SCI-PROBE scores.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–83.
Glickman S, Kamm MA. Bowel dysfunction in spinal-cord-injury patients. Lancet. 1996;347:1651–3.
Kirk PM, King RB, Temple R, Bourjaily J, Thomas P. Long-term follow-up of bowel management after spinal cord injury. SCI Nurs. 1997;14:56–63.
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I. Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol. 1990;85:1114–9.
Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: a postal survey in the United Kingdom. Spinal Cord. 2009;47:323–30. quiz 31-3.
Dunn M. Social discomfort in the patient with spinal cord injury. Arch Phys Med Rehabil. 1977;58:257–60.
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Coggrave M, Norton C, Cody JD. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev. 2014;1:Cd002115.
Burns AS, St-Germain D, Connolly M, Delparte JJ, Guindon A, Hitzig SL, et al. A phenomenological study of neurogenic bowel from the perspective of individuals living with spinal cord injury. Arch Phys Med Rehabil. 2015;96:49–55.
Burns AS, St-Germain D, Connolly M, Delparte JJ, Guindon A, Hitzig SL, et al. Neurogenic bowel after spinal cord injury from the perspective of support providers: a phenomenological study. PM R. 2015;7:407–16.
Pires JM, Ferreira AM, Rocha F, Andrade LG, Campos I, Margalho P, et al. Assessment of neurogenic bowel dysfunction impact after spinal cord injury using the International Classification of Functioning, Disability and Health. Eur J Phys Rehabil Med. 2018;54:873–9.
Wheeler TL, de Groat W, Eisner K, Emmanuel A, French J, Grill W, et al. Translating promising strategies for bowel and bladder management in spinal cord injury. Exp Neurol. 2018;306:169–76.
Craven BC, Verrier MC, Balioussis C, Wolfe DL, Hsieh JTC, Noonan VK, et al. Rehabilitation environmental scan atlas: capturing capacity in Canadian SCI rehabilitation. Vancouver, BC: Rick Hansen Institute; 2012. http://www.rickhanseninstitute.org/e-scan-atlas.
Choukou MA, Best KL, Craven BC, Hitzig SL. Identifying and classifying quality of life tools for assessing neurogenic bowel dysfunction after spinal cord injury. Top Spinal Cord Inj Rehabil. 2019;25:1–22.
DeWalt DA, Rothrock N, Yount S, Stone AA. Evaluation of item candidates: the PROMIS qualitative item review. Med Care. 2007;45:S12–21.
Department of Health & Human Support Food & Drug Administration. Patient-reported outcome measures: use in medical product development to support labeling claims. Rockville, MD: U.S. Food and Drug Administration; 2009.
Streiner DL, Norman GR. Health Measurement Scales: A practical guide to their development and use. Fourth ed. New York, NY: Oxford University Press; 2008.
Khanna P, Agarwal N, Khanna D, Hays RD, Chang L, Bolus R, et al. Development of an online library of patient-reported outcome measures in gastroenterology: the GI-PRO database. Am J Gastroenterol. 2014;109:234–48.
Krogh K, Perkash I, Stiens SA, Biering-Sorensen F. International bowel function extended spinal cord injury data set. Spinal Cord. 2009;47:235–41.
Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–31.
Tulsky DS, Kisala PA, Tate DG, Spungen AM, Kirshblum SC. Development and psychometric characteristics of the SCI-QOL Bladder Management Difficulties and Bowel Management Difficulties item banks and short forms and the SCI-QOL Bladder Complications scale. J Spinal Cord Med. 2015;38:288–302.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. Thousand Oaks, CA: Sage Publications; 2005.
Beatty PC, Willis GB. Research synthesis: the practice of cognitive interviewing. Public Opin Q. 2007;71:287–311.
Bredart A, Marrel A, Abetz-Webb L, Lasch K, Acquadro C. Interviewing to develop Patient-Reported Outcome (PRO) measures for clinical research: eliciting patients’ experience. Health Qual Life Outcomes. 2014;12:15.
Coggrave MJ, Ingram RM, Gardner BP, Norton CS. The impact of stoma for bowel management after spinal cord injury. Spinal Cord. 2012;50:848–52.
Patel DP, Elliott SP, Stoffel JT, Brant WO, Hotaling JM, Myers JB. Patient reported outcomes measures in neurogenic bladder and bowel: a systematic review of the current literature. Neurourol Urodyn. 2016;35:8–14.
Krogh K, Emmanuel A, Perrouin-Verbe B, Korsten MA, Mulcahey MJ, Biering-Sorensen F. International spinal cord injury bowel function basic data set (Version 2.0). Spinal Cord. 2017;55:692–8.
Juul T, Bazzocchi G, Coggrave M, Johannesen IL, Hansen RB, Thiyagarajan C, et al. Reliability of the international spinal cord injury bowel function basic and extended data sets. Spinal Cord. 2011;49:886–91.
Funding
This study was funded by The Rick Hansen Institute (RHI #G2015-28).
Author information
Authors and Affiliations
Contributions
ASB was responsible for designing the study protocol, participating in the outcomes advisory committee, advising on data analysis, interpreting the data, and drafting the report. JJD was responsible for designing the study protocol, recruiting study participants, completing data collection, extracting and analyzing data, interpreting results, and drafting the methods and results sections of the report. SLH was responsible for designing the study protocol, participating in the outcomes advisory committee, and reviewing the report. BCC was responsible for designing the study protocol, participating in the outcomes advisory committee, and reviewing the report. JS was responsible participating in the outcomes advisory committee, and reviewing the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers/animals were followed during the course of this research. All study procedures were approved by the University Health Network research ethics board (#15-9461).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Burns, A.S., Delparte, J.J., Hitzig, S.L. et al. Development of a novel neurogenic bowel patient reported outcome measure: the Spinal Cord Injury Patient Reported Outcome Measure of Bowel Function & Evacuation (SCI-PROBE). Spinal Cord 58, 1060–1068 (2020). https://doi.org/10.1038/s41393-020-0467-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0467-x