Abstract
Study design
Multicenter prospective observational study of people with acute traumatic spinal cord injury (TSCI) admitted to rehabilitation.
Objectives
To update epidemiological characteristics of a TSCI Italian population and verify the impact of patient characteristics at admission on two outcomes: functional gain (SCIM III) and discharge destination.
Setting
Thirty-one SCI centers for comprehensive rehabilitation in 13 Italian regions.
Methods
All consecutive individuals admitted with acute TSCI were enrolled from October 1, 2013 to September 30, 2014; data were recorded on rehabilitation admission and discharge. Functional gain and discharge destination were identified as outcome measures and statistically analyzed with patient characteristics at admission to identify early outcome predictors.
Results
Five hundred and ten individuals with TSCI met inclusion criteria; falls represented the most frequent etiology (45%). On admission, AIS A-B-C tetraplegia was reported in 35% of cases; AIS A-B-C paraplegia in 40%; AIS D paraplegia/tetraplegia in 25%. The majority were discharged home (72%). The mean (SD) SCIM gain was 38 ± 26 points. A predictive model was found for discharge setting: individuals with fall-related injuries, severe SCI (AIS A-B-C tetraplegia), tracheal cannula or indwelling catheter on admission, were less likely to be discharged home (OR 95% CI 0.15 [0.06, 0.35]). A model with a lower predictive power was found for SCIM gain, with lower score expected for females, older age, higher severity of SCI, a longer onset of injury admission interval (OAI), and mechanical ventilation on admission.
Conclusions
Prognostic factors in early rehabilitation are still hard to identify, making it difficult to correctly approach customized rehabilitation.
Similar content being viewed by others
Introduction
Early outcome prediction after traumatic spinal cord injury (TSCI) is pivotal in the rehabilitation process, allowing clinicians to adequately inform both patients and families about prognosis, to predict rehabilitation potential, to plan rehabilitation process and to assess its efficacy. Furthermore, it is crucial to allocate resources appropriately. The sooner the endpoints are predicted, the better the rehabilitation pathway can be identified [1, 2].
The modification of epidemiological data during time may suggest to health policy-makers what is necessary to change in the organizational and clinical approach of management of spinal cord injury (SCI). Otherwise, even if the literature may provide tentative instruments of prediction of functional achievement [3], clinicians often continue to rely on intuitive assessment when defining which functional outcome is an appropriate target for each person with TSCI.
Whatever the specific evaluation for each person, the mission of SCI rehabilitation programs is to help patients take full advantage of neurological recovery and maximize functional improvement. Being discharged home is usually a major prerequisite to benefit of regained activity and achieve full participation [4]. It is known that people with SCI are frequently discharged home after rehabilitation hospitalizations, but it is not clear which factors may facilitate or hinder this goal [5, 6]. Functional gain is also a fundamental endpoint of the rehabilitation process; however, it remains a difficult parameter to evaluate in such a heterogeneous population [7]. As a matter of fact, several aspects may have an impact on it, including individual-related conditions, severity of the initial neurological damage, time interval between injury and access to rehabilitation care, etc. In the literature, many articles and reviews suggest predictors of functional outcomes after SCI [1, 2, 7,8,9]. The effect of some of these parameters, such as age at trauma, revealing relevant modifications in the contemporary Italian population, is controversial [10,11,12,13]. Also, many clinical aspects, such as respiratory and bladder function at admission, trauma-associated lesions, complications arising in acute care units (ICU, NCH, etc.), are not univocal as predictors [14,15,16].
About 20 years ago, the GISEM study, a prospective observational study that included 32 Italian SCI centers, collected socio-demographic and clinical data at admission and discharge from rehabilitation, and described the Italian situation at the time. A high incidence of traumatic SCI after transport accidents (53%) was one of the most peculiar aspects of the study. The outcome was evaluated with AIS improvement, bladder autonomy, and discharge home [17].
In the last two decades, the epidemiology of TSCI has deeply changed all over the western world. Italy, in particular, which has one of the oldest populations in the world, experienced a profound modification [18,19,20,21]. There has been a substantial increase of the average age at trauma and of cervical lesions, thus certainly resulting in greater fragility and complexity of patients accessing SCI rehabilitation departments. On the other hand, the increase of incomplete injuries has raised new challenges and new functional and rehabilitation goals during first hospitalization, aiming at the highest level of function and participation. Even the causes of traumatic SCI have changed as relative percentage. It is therefore crucial to evaluate and update the predictors of the main outcomes, according to our reality and in the light of the new epidemiological trends.
The main objective of this 1-year multicenter prospective observational study is to verify if patient characteristics, acute neurological impairment and some acute clinical indicators may have an impact on two chosen outcomes: functional gain, evaluated with Spinal Cord Independence Measure (SCIM III), and discharge home. The secondary objective is to update, 20 years later, the type and the weight of some early outcome predictors, in the light of the recent epidemiological trends.
Methods
This research was approved and funded by the Italian Ministry of Health (CCM number 15756 of 17-07-2012 and “Institutional research”). A regional network for a systematic data collection was created under the supervision of Age.Na.S. (National Agency for Regional Health Services).
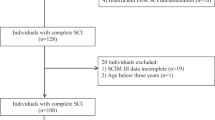
This prospective observational study included all consecutive persons with TSCI admitted to 31 SCI centers of 13 Italian regions, from October 1, 2013 to September 30, 2014 (Fig. 1) [21]. Data were collected by clinicians in two phases: T1 at admission and T2 at discharge. People who were still hospitalized at the end of enrollment (September 30, 2014) were assessed at discharge whatever the date.
A TSCI case was defined, for the purpose of this study, as an acquired traumatic lesion of the spinal cord or cauda equina, resulting in a complete or partial, transient or permanent loss of motor, sensory, bladder or bowel function below the level of the lesion. Exclusion criteria were: age below 16 years; time interval between event and admission to rehabilitation >12 months; nontraumatic etiology; other neurological diagnosis.
An etiological classification of the lesion was performed according to the International Spinal Cord Injury Core Data Set [22]. The International Standards for Neurological Classification of SCI was used to assess the level and completeness of the lesion [23].
A web database was created. It included a form for the collection of the following data: gender, age, origin of the patient (migration between regions: yes/no), nationality, date of the acute episode, spinal surgery (yes/no), and date of surgery, injury date, and admission date to rehabilitation setting were used to calculate onset-admission interval (OAI) and length of stay (LoS). At T1 other clinical data were collected: lesion level, completeness according to ASIA-ISCOS impairment scale (A-B-C-D), SCIM III. For the statistical analysis, level and completeness of injury were grouped as: AIS A-B-C paraplegia/AIS A-B-C tetraplegia/all D [24]. The causes of trauma (transport accidents, falls, sports, assault, or other) were grouped for the statistical analysis as follows: (1) transport accidents; (2) falls; (3) other causes (merged together). Data on breathing (mechanical or spontaneous), tracheotomy (yes/no), associated traumas (brain injury, other, or none), bladder management (indwelling catheter vs. all other solutions), complications (pressure ulcers, osteomyelitis, deep vein thrombosis, pulmonary embolism, respiratory complications, urological complications, heterotopic ossifications, complications of spine surgery, multiresistant infections) were also recorded. Complications were analyzed globally as absent or present (one or more). The most frequent complications (pressure ulcers, respiratory and infectious complications) were taken into consideration separately.
At T2, the following data were evaluated: mortality, changes in the neurological (AIS A-B-C-D-E) and functional status (SCIM III), LoS, and discharge destination.
The main outcomes considered were: discharge destination (home or other destination) and functional gain (SCIM gain = SCIM score at discharge − SCIM score at admission) (dependent variables).
All social, personal, anamnestic, and clinical indicators considered were used as result indicators (independent variables).
Statistical analysis
Categorical variables were calculated as frequencies and percentages for the whole sample. Standard descriptive statistics were used to summarize data, with respect to demographic and clinical characteristics.
First, a univariate analysis was performed to assess the ability of each feature to predict an outcome. Second, a multivariate analysis was performed, including all variables of interest, to evaluate the added value of a combination of predictors and to account for confounding and multicollinearity.
For each outcome, a model selection was applied to determine the best multivariate model among all possible linear models, using three different information criteria, such as AIC (Akaike Information Criterion), BIC (the Bayesian version of AIC), and BICg (an extended version of BIC). The model selection was performed using the R library “bestglm” [25]. Model performance was evaluated by area under the ROC curve (AUC) in the binary model for discharge destination and by R2 in the linear model for SCIM gain.
Statistical analyses were performed using STATA version 12.1 (StataCorp. 2011. Stata Statistical software: Release 12. College Station, TX: StataCorp LP) and R v3.3.2 (R Foundation for Statistical Computing, Vienna, Austria). All tests were two sided, and an alpha level of 0.05 was set for statistical significance.
Results
Out of the 1049 people enrolled at admission to SCI inpatient rehabilitation, 510 individuals met the inclusion criteria and were included in the analysis. The remaining were excluded for the following reasons: nontraumatic SCI (496); incomplete records (40 = 17 missing data at T1 + 23 missing data at T2); transferred from foreign countries; exceeding the maximum time limit between event and admission. This article is therefore based on a sample of 497 patients (Fig. 2).
Thirteen individuals (3%) died during the rehabilitation treatment period. The cause of death was not reported. The features of this group were: etiology (transport accidents: seven; falls: four, assault: two); the median (IQR) time from admission to death was 74 days (37–163 days). The median (IQR) age ate injury was 71 years (69–77 years); 11 (85%) suffered from tetraplegia and 2 (15%) from paraplegia; the most frequently reported complications during hospitalization were respiratory (11), pressure ulcers (10), spine instability (5), multiresistant infections (5), pulmonary embolism (1), and urological infections (2).
The descriptive analysis of the characteristics of surviving population at admission is shown in Table 1.
Male-to-female ratio was 4:1; mean age for all causes was 50 years (SD = 20 years); falls were the most frequent etiology (45%), followed by transport accidents (40%). A large number of SCIs were associated with multitrauma (42%) and traumatic brain injury (21%).
Only 25% of the population did not receive spinal surgery after trauma; 23% of the population received rehabilitation treatment in centers outside their area of residence. The median (IQR) OAI was 16 days (11–34 days).
As concerns the severity of the lesion, 35% presented tetraplegia (AIS A-B-C) and 40% paraplegia (AIS A-B-C) at admission. The remaining group (25%) included AIS D paraplegia or tetraplegia. At admission, AIS A was found in 173 patients, AIS B in 78, AIS C in 122, and AIS D in 104 (Table 2). Fifty-four patients needed mechanical ventilation at admission (11%). At T1, the great majority had an indwelling urethral catheter and the main complications were respiratory (34%) and pressure ulcers (30%).
LoS, neurological improvement, discharge setting, and SCIM gain were considered as rehabilitation outcomes. The median (IQR) LoS was 135 days (79–190 days). The neurological improvement is shown in Table 2: AIS condition was not reported at admission or discharge for 18 individuals, whose improvement was not possible to evaluate. The percentage of people reporting a worst AIS condition at discharge is negligible; out of 173 AIS A complete lesions at admission, 13 (8%) converted to B; 9 (5%) to C; and only 2 (1%) to D (Table 2).
The majority of patients (72%) were discharged home; a significant number of those not returning home were transferred to a nonspecific rehabilitation facility (15%).
The mean SCIM gain, calculated as the difference between SCIM at discharge (57 ± 29) and SCIM at admission (18 ± 16), was 38 (±26) points.
The predictive factors for outcome that were reported at admission were investigated with univariate analysis. A longer LoS was directly and significantly correlated with discharge home (Table 3). Moreover, discharge home was inversely significantly related to age, with the mean age of the individuals not discharged home exceeding by 9 years those discharged home. An inverse significant correlation was found between discharge home and severity of the lesion, with discharge home three times less frequent in the AIS A-B-C paraplegia group and six times less frequent in the AIS A-B-C tetraplegia group in respect of AIS D group. Discharge home was also four times less frequent in patients with mechanical ventilation or tracheal device and 50% less frequent in patients with respiratory complications or pressure ulcers at admission.
SCIM gain (Table 4) showed a weakly significant inverse correlation with LoS. A worst SCIM gain was significantly correlated with older age, etiology (lower score registered for victims of fall), female gender (9-point lower gain), longer OAI, associated trauma, but no brain trauma. Moreover, it was highly significantly correlated with the severity of the lesion (AIS A-B-C tetraplegia has 20-point lower gain, while AIS A-B-C paraplegia group has 8-point lower gain than all AIS D), mechanical ventilation (20-point lower gain) and complications (11-point lower gain for pressure ulcers and 8-point lower gain for respiratory complications).
The multivariate analysis designs a model with a good predictive power (80% AUC, Area under ROC Curve) (Fig. 3) for the discharge home outcome (Table 3): individuals with fall-related SCI, severe SCI (AIS A-B-C tetraplegia: eight times less likely; AIS A-B-C paraplegia: four times less likely than all AIS D), tracheal cannula (four times less likely) or indwelling catheter (six times less likely) at admission are less likely to be discharged home. As regards SCIM gain (Table 4), a lower score is expected for females, older age at admission (3-point lower score/10 years of age), severity of SCI (AIS A-B-C tetraplegia: 23 points and AIS A-B-C paraplegia: 14 points lower than all AIS D), a longer OAI (1-point lower score/week), mechanical ventilation at admission (14-point lower score); the model shows a lower predictive power (only 25% of the variance is explained).
Discussion
The study allowed us to detect some descriptive aspects that differ from data obtained by a previous comparable prospective, rehabilitation-based study (GISEM study), carried out 20 years earlier [17], drawing an epidemiological trend in agreement with the recent literature from other countries [18, 26]. We then tried to identify significant early predictors of the selected outcome measures: discharge home and functional gain (SCIM gain) during rehabilitation.
The low mortality (13/510) reported during rehabilitation can be explained because the data collection excluded the high-risk immediate postevent period [27]. Although a statistical comparison between heterogeneous groups of people with SCI who survived or died during rehabilitation was not carried out, the median age of the deceased group exceeded by 20 years that of the survived group, and tetraplegia was more represented in the deceased group.
Compared with the previous study [17, 28], there was a marked change in the mean age at the time of SCI onset of the survived population (from 38.5 to 50 years). This aspect has probably implied also a change in the etiology of trauma. We observed a decrease in the proportion of transport accidents (from 54 to 41%) and an increase in the proportion of falls (from 23 to 45%), especially of low-level falls. The mechanism involved in the predominant etiology makes tetraplegia more frequent (247 patients; 50%) in respect of 40% of GISEM study, with a high frequency of AIS D lesions (71 patients; 14%). These data are consistent with the recent international literature concerning the average age at injury and the etiology in high-income countries [18, 27, 29].
The mean OAI is reduced (from 34 to 15 median days), possibly due to a better organization of the acute rehabilitation pathway implemented in Italy in the last two decades, with an increase of the number of specific SCI rehabilitation facilities inside trauma centers/emergency hospitals on the whole Italian territory. It is noteworthy that preventable complications, such as pressure ulcers, did not decrease (30% vs. 27% in GISEM), possibly due to the increased clinical complexity of patients with acute SCI, as suggested by the report of 34% respiratory complications on admission (12% in GISEM study), 10% ventilated patients and a higher percentage of tetraplegia.
The median LoS was similar, with 135 median days reported in the current study vs. 122 in the GISEM study. The number of people being discharged home has decreased in the last 20 years (from 82 to 72%) [28]. These data may partially be explained by the increased percentage of incomplete lesions, leading to transfers to nonspecific SCI rehabilitation centers (15%), for outpatient rehabilitation or lower intensity rehabilitation programs. A higher patient complexity and a high burden of assistance may possibly discourage families from taking their relatives home at discharge. The increase of the mean age may also result in too few or too old relatives, that cannot guarantee an ongoing commitment towards their next of kin with SCI. In our sample 46% of patients who need to maintain tracheal cannula are discharged home.
The main negative predictors of discharge home are etiology (fall-related SCI), severe SCI (with an intuitive decreasing profile from “non functional” AIS A-B-C tetraplegia to incomplete AIS D lesions), and clinical severity indicators, such as indwelling catheter and tracheal cannula, at admission. In comparing the multivariate analysis for discharge home, only bladder management is still a predictive factor of outcome, as it was in the previous study.
As regards SCIM gain, a comparison with the Italian previous data is not possible because no functional outcome had been reported 20 years ago. The mean (SD) total SCIM III score reported at admission in the sample of this study (18 ± 16) is lower than other SCI samples reported in the literature in similar case-mix, ranging from the lowest in Israel (25.1 ± 17.2) to the highest in the USA (42, range 13–68) [30].
Lower score expected in the predictive model for severe SCI and mechanical ventilation at admission are consistent with reports in the literature [3, 14]. Age is also involved in the predictive model of SCIM gain at discharge: we found a significant correlation between age, AIS grade, and future functional status. Clinicians perceive that an older age is often in relation with a worse outcome, but this effect varies across the spectrum of injury severity and has to be considered in that perspective. A longer OAI is the most amendable factor in the model, suggesting a role of early management in the risk of complications, but also that early complications in complex patients are more often cause of delay in transferring patients to rehabilitation, thus hampering the rehabilitation process.
The presence of multiple trauma is significantly associated with a better SCIM gain outcome. These data could seem a contradiction at first reading, but it emerges that most of those who have a polytrauma have a post traumatic etiology and are younger. As previously said, those who are younger and have a post traumatic etiology have a better SCIM gain prognosis, thus the correlation can be explained.
Limitations
This study’s main limitation is the possible selection bias due to losing patients who died or spread out, because of an uneven acute rehabilitation pathway or overwhelming complications. Moreover, this study cannot be considered representative of the whole Italian population, since it covers about half of it with a nonhomogeneous distribution of recruitment centers.
Conclusions
Ageing and increasing complexity of people with SCI in a high-income country is a very challenging condition. Prognostic factors in early rehabilitation are still hard to identify, making it difficult to facilitate clinical interpretation, develop customized treatment and define the correct approach to rehabilitation programs for every single person with SCI, in the context of cost/effectiveness.
Data availability
Data are included in the registry of 2012 CCM project according to national privacy regulations and are available by a formal request to the Emilia-Romagna Regional Health Authority.
References
Richard-Denis A, Beausejour M, Thompson C, Nguyen BH, Mac-Thiong JM. Early predictors of global functional outcome after traumatic spinal cord injury: a systematic review. J Neurotrauma. 2018;35:1–21.
Wilson JR, Cadotte DW, Fehlings MG. Clinical predictors of neurological outcome, functional status, and survival after traumatic spinal cord injury: a systematic review. J Neurosurg Spine. 2012;17:11–26.
Aidinoff E, Front L, Itzkovich M, Bluvshtein V, Gelernter I, Hart J, et al. Expected spinal cord independence measure, third version, scores for various neurological levels after complete spinal cord lesions. Spinal Cord. 2011;49:893–6.
World Health Organization, International Spinal Cord Society. International perspectives on spinal cord injury. Geneve: World Health Organization; 2013. pp. 73–8.
Cheng CL, Plashkes T, Shen T, Fallah N, Humphreys S, O’Connell C, et al. Does specialized inpatient rehabilitation affect whether or not people with traumatic spinal cord injury return home? J Neurotrauma. 2017;34:2867–76.
New PW. Prospective study of barriers to discharge from a spinal cord injury rehabilitation unit. Spinal Cord. 2015;53:358–62.
AlHuthaifi F, Krzak J, Hanke T, Vogel LC. Predictors of functional outcomes in adults with traumatic spinal cord injury following inpatient rehabilitation: a systematic review. J Spinal Cord Med. 2017;40:282–94.
Fromovich-Amit Y, Biering-Sørensen F, Baskov V, Juocevicius A, Hansen HV, Gelernter I, et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord. 2009;47:597–603.
Ackerman P, Morrison SA, McDowell S, Vazquez L. Using the spinal cord independence measure III to measure functional recovery in a post-acute spinal cord injury program. Spinal Cord. 2010;48:380–7.
Abdul-Sattar AB. Predictors of functional outcome in patients with traumatic spinal cord injury after inpatient rehabilitation in Saudi Arabia. Neurorehabilitation. 2014;35:341–7.
Facchinello Y, Beausejour M, Richard-Denis A, Thompson C, Mac-Thiong JM. The use of regression tree analysis for predicting the functional outcome following traumatic spinal cord injury. J Neurotrauma. 2017. https://doi.org/10.1089/neu.2017.5321.
Wilson JR, Davis AM, Kulkarni AV, Kiss A, Frankowski RF, Grossman RG, et al. Defining age-related differences in outcome after traumatic spinal cord injury: analysis of a combined, multicenter dataset. Spine J. 2014;14:1192–8.
Furlan JC, Hitzig SL, Craven BC. The influence of age on functional recovery of adults with spinal cord injury or disease after inpatient rehabilitative care: a pilot study. Aging Clin Exp Res. 2013;25:463–71.
Kaminski L, Cordemans V, Cernat E, Bra Ki M, Mac-Thipong JM. Functional outcome prediction after traumatic spinal cord injury based on acute clinical factors. J Neurotrauma. 2017;34:2027–33.
Wilson JR, Grossman RG, Frankowski RF, Kiss A, Davis AM, Kulkarni AV, et al. A clinical prediction model for long-term functional outcome after traumatic spinal cord injury based on acute clinical and imaging factors. J Neurotrauma. 2012;29:2263–71.
Craven BC, Kurban D, Farahani F, Rivers CS, Ho C, Linassi G, et al. Predicting rehabilitation length of stay in Canada: it’s not just about impairment. J Spinal Cord Med. 2017;40:676–86.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil. 2003;84:1266–75.
DeVivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Selvarajah S, Hammond ER, Haider AH, Abularrage CJ, Becker D, Dhiman N, et al. The burden of acute traumatic spinal cord injury among adults in the United States: an update. J Neurotrauma. 2014;31:228–38.
Pérez K, Novoa AM, Santamariña-Rubio E, Narvaez Y, Arrufat V, Borrell C, et al. Incidence trends of traumatic spinal cord injury and traumatic brain injury in Spain, 2000-9. Accid Anal Prev. 2012;46:37–44.
Ferro S, Cecconi L, Bonavita J, Pagliacci MC, Biggeri A, Franceschini M. Incidence of traumatic spinal cord injury in Italy during 2013-4: a population-based study. Spinal Cord. 2017;55:1103–7.
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
Kirshblum SC, Burns SP, Biering-Sørensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34:535–46.
DeVivo MJ, Biering-Sørensen F, New P, Chen Y. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord. 2011;49:596–9.
Zhang Z. Variable selection with stepwise and best subset approaches. Ann Transl Med. 2016;4:136.
Lee BB, Cripps R, New P, Fitzharris M, Noonan V, Hagen EM, et al. Demographic profile of spinal cord injury. In: Chhabra HS, editor. ISCoS textbook on comprehensive management of spinal cord injuries. New Delhi: Wolters Kluwer; 2015. pp. 36–52.
Shibahashi K, Nishida M, Okura Y, Hamabe Y. Epidemiological state, predictors of early mortality, and predictive models for traumatic spinal cord injury: a multicenter nationwide cohort study. Spine. 2019;44:479–87.
Pagliacci MC, Celani MG, Spizzichino L, Zampolini M, Aito S, Citterio A, et al. Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord. 2003;41:620–8.
National Spinal Cord Injury Statistical Center (NSCISC). 2018 Annual Report. Complete Public Version. Birmingham, AL: University of Alabama; 2018. https://www.nscisc.uab.edu/public/2018%20Annual%20Report%20-%20Complete%20Public%20Version.pdf.
Fromovich-Amit Y, Biering-Sørensen F, Baskov V, Juocevicius A, Hansen HV, Gelernter I, et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord. 2009;47:597–603.
Acknowledgements
CCM is the National Center for Diseases prevention and Control whose task is to liaise with the Ministry of Health and the regional governments as far as surveillance and prevention are concerned and whose aim is to promptly respond to emergencies. http://www.ccm-network.it/progetto.jsp?id=node/1846&idP=740.
Collaborating Hospitals and Regional Health Authorities
M.V. Actis, M. Stillittano (Città della Salute e della Scienza Hospital, Turin); S. Petrozzino (Alessandria Hospital); C. Cisari (Novara Hospital), M. Salvini (Piedmont Region); T. Redaelli, R. Tosi (Niguarda Hospital, Milano); C.M. Borghi, A. Bava (Pini CTO Hospital, Milano); C. Pistarini, (IRCCS Maugeri Foundation, Pavia); G. Molinero, A. Signorelli (Bergamo Hospital); S. Sandri (Legnano- Magenta Hospital); F. Simeoni (Garbagnate Hospital); M. Brambilla (Valtellina Hospital) M.A. Banchero, A. Olivero, G. Zanaboni (Lombardy Region); R. Avesani (Don Calabria Hospital, Negrar, Verona); G. Bertagnoni, M. Leucci, L. Lain (S. Bortolo Hospital, Vicenza); M. Saia (Veneto Region); A. Zampa (Gervasutta Hospital, Udine); P. Del Fabro (Udine Hospital); M. Saccavini (Palmanova Hospital, Udine); A. Fanzutto (Friuli Venezia Giulia Region); A. Massone (Santa Corona Hospital, Pietra Ligure, Savona); J. Bonavita, D. Gaddoni, S. Olivi, G. Musumeci, R. Pederzini (Montecatone Rehabilitation Institute, Imola, Bologna); H. Cerrel Bazo, D. Nicolotti, (Villanova d’Arda Hospital, Piacenza); M. Nora, R. Brianti, C. Iaccarino, A. Volpi (Parma Hospital); A. Lombardi, S. Cavazza, F. Casoni (Baggiovara Hospital, Modena); F. De Iure, G. Gordini, R. Piperno (Maggiore Hospital, Bologna); G. Teodorani, A. Naldi, G. Vergoni, (Cesena Hospital); E. Maietti, A. Botti (Ferrara Hospital); S. Ferro, G. Pagoto (Emilia-Romagna Region); G. Del Popolo, M. Moresi, M. Postiglione, C. Bini (Careggi Hospital, Firenze); M. Tagliaferri (Tuscany Region); M. A. Recchioni, P. Pelaia (Ospedali Riuniti, Ancona); L. Di Furia (Marche Region); M.C. Pagliacci, R. Maschke, L. Caruso, L. Speziali (Perugia Hospital); M. Zenzeri (Umbria Region); P. Fiore, R. Marvulli (Bari Hospital); R. Nardulli (IRCCS Maugeri Foundation, Cassano Murge, Bari); C. Lanzillotti (IRCCS Maugeri Foundation, Ceglie Messapica, Brindisi); M. Ruccia (Puglia Region); M.P. Onesta, T. Di Gregorio (Cannizzaro Hospital, Catania); F. Franchina (Villa Sofia Hospital, Palermo); M.G. Furnari (Sicily Region); C. Pilati, M. Merafina, F. Crescia (Alesini CTO Hospital, Rome); D. Fletzer (Ostia Hospital, Rome); G. Scivoletto (IRCCS S. Lucia Foundation, Rome); N. Di Lallo (Lazio Region).
Funding
This study was financed within the framework of the 2012 CCM program.
Author information
Authors and Affiliations
Consortia
Contributions
MF participated in the scientific coordination of the project and contributed to writing the report. JB coordinated data collection and contributed to writing the report. LC conducted the statistical analyses and contributed to writing the report. SF coordinated all scientific aspects of the research project. MCP coordinated data collection and contributed to writing the report.
Corresponding author
Ethics declarations
Ethics statement
We certify that all applicable institutional and governmental regulations concerning the ethical use of data originally collected for clinical purpose were followed during the course of this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Franceschini, M., Bonavita, J., Cecconi, L. et al. Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome. Spinal Cord 58, 768–777 (2020). https://doi.org/10.1038/s41393-020-0421-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-0421-y
This article is cited by
-
The impact of COVID-19 and associated lockdowns on traumatic spinal cord injury incidence: a population based study
Spinal Cord (2024)
-
Incidence and mortality of spinal cord injury from 2008 to 2020: a retrospective population-based cohort study in the Piedmont Region, Italy
Spinal Cord (2023)
-
Causes and length of stay of readmission among individuals with traumatic spinal cord injury: a prospective observational cohort study
Spinal Cord (2023)
-
Epidemiology of traumatic spinal cord injury: a large population-based study
Spinal Cord (2022)
-
Respiratory morbidity and mortality of traumatic cervical spinal cord injury at a level I trauma center in India
Spinal Cord Series and Cases (2021)