Abstract
Study design
Descriptive study of the second community survey of the Swiss Spinal Cord Injury Cohort Study (Survey 2017) conducted between 03/2017 and 03/2018.
Objectives
To describe the methodology, recruitment results, characteristics of participants and non-participants, and non-response of the Survey 2017.
Setting
Community.
Methods
Description of the sampling strategy and sampling frame. Recruitment results and characteristics of participants and non-participants of the two Survey 2017 questionnaire modules were analyzed using descriptive statistics. Determinants of survey participation were examined using multivariable logistic regression, and the impact of non-response bias on survey results was evaluated using inverse-probability weighting.
Results
Out of 3959 persons who met the eligibility criteria, 1530 responded to module 1 (response rate 38.6%) and 1294 to module 2 (response rate 32.7%) of the Survey 2017. Of the 4493 invited persons, 1549 had participated in the first SwiSCI community survey conducted in 2012/2013. Of these, 1332 were invited to the Survey 2017 and 761 participated in module 1 (response rate 58.9%) and 685 in module 2 (response rate 53.1%). The majority of module 1 participants were male (71.2%, 95% CI: 68.9, 73.5), with a median age of 57 (IQR: 46.0, 67.0) years and incomplete paraplegia (41.9%, 95% CI: 39.3, 44.5). Survey non-response was higher in the oldest age group, among females, and those with tetraplegia.
Conclusions
The design of the Survey 2017 was successful in recruiting a substantial proportion of the SCI source population in Switzerland. To counteract survey non-response, survey weights may be applied to subsequent analyses.
Sponsorship
none
Similar content being viewed by others
Introduction
Longitudinal population-based studies provide an essential basis for evidence-based development of health policy and public health strategies [1] and are particularly beneficial for populations for which data are scarce, such as people living with spinal cord injury (SCI). Several large-scale cohort studies on SCI, such as the SCI model systems from the USA, the British ageing with SCI study, and the Canadian SCI community survey [2,3,4] have been developed, and these contribute to a better understanding of affected individuals’ life situation. The Swiss Spinal Cord Injury Cohort Study (SwiSCI) complements this evidence base by prospectively investigating aspects of functioning, health, well-being, and life expectancy of persons with SCI living in Switzerland [5, 6].
Population-based studies in the disability setting are important; however, their implementation is subject to various methodological challenges, one of which is the compilation of a representative source population, i.e. the sampling frame from which participants are drawn [7]. Poor knowledge of the target population, i.e. all persons living with SCI in a given region, due to the absence of central registries that could provide systematic information on affected people, is a frequent limitation in disability research [8, 9]. In the absence of such registries, persons meeting the eligibility criteria may be recruited from multiple channels to build up a sampling frame. This strategy often increases the complexity of the survey design and restricts the generalizability of study results, unless the source population does fully match the entire target population. Another challenge is the achievement of satisfying recruitment outcomes; response rates and non-response bias are important indicators of a survey’s methodological quality. Bias introduced by survey non-response can seriously affect the representativeness of the source population and the generalizability of study results [10], which is highly problematic when drawing conclusions to inform policy [1]. To understand and correctly interpret longitudinal population-based data, a sound description of a survey’s methodological quality components, such as sampling frame, response rates as well as responder and non-responder characteristics is inevitable [10,11,12].
The SwiSCI community survey represents a population-based study that relies on complex, multi-channel recruitment of a representative source population and multiple measurement time points. The objective of the present study is to describe the methodology, recruitment results, characteristics of participants and non-participants, and non-response of the second SwiSCI community survey (subsequently referred to as Survey 2017). Specifically, we aim to (1) detail the survey protocol (i.e. study design, sampling frame, recruitment procedure and questionnaire modules), (2) provide the participation rates and characteristics of the study participants, (3) identify determinants of study participation to assess potential non-response bias, and (4) examine the impact of potential non-response bias on selected survey results. The present paper provides a useful reference for the various SwiSCI analyses of this special edition of Spinal Cord and for upcoming studies using the Survey 2017 data.
Methods
Survey protocol
Study design, setting, and procedures
The Survey 2017 was conducted between 3/2017 and 3/2018, around 5 years after the first SwiSCI community survey that was performed between 9/2011 and 3/2013 (subsequently referred to as Survey 2012). The rationale and design of the Survey 2012 are described in detail elsewhere [5, 6]. Briefly, it consisted of three modules that were successively sent to the participants with a time interval of ~3 months across all modules. In the Survey 2017, the number of modules was reduced to two to lower participant burden and dropout risk. Module 1 included 132 items on sociodemographic factors, work situation, secondary health problems, general health, quality of life and mood, functional independence and participation, and environmental factors. Module 2 was sent to the participants 4–6 weeks after module 1 and included 188 items covering pain, sleep and mood, activity and participation, work integration, care situation, health services use, health information seeking behavior, perceived discrimination and psychological personal factors. Supplementary File 1 details the measurement time points and modules of the Survey 2012 and 2017.
The items in the Survey 2017 modules were selected based on the SCI-specific core sets of the International Classification of Functioning, Disability and Health [13, 14], complemented with additional variables on psychological personal factors [15] and the subjective appraisal of health and well-being. Because the Survey 2017 was part of the International Spinal Cord Injury (InSCI) community survey [16] additional items from that survey were included. To allow for longitudinal comparison between the Survey 2012 and Survey 2017, key items from the 2012 modules were retained in 2017. The 2017 modules included new areas of interest, such as health information seeking behavior and perception of discrimination. The Survey 2017 modules are available online [17].
A mixed-mode data collection design including paper-and-pencil or online questionnaire and face-to-face or telephone interviews was used to achieve optimal response rates [6, 18]. The modules were provided in three official Swiss languages (German, French, or Italian). Unless validated translations of items were available, translations were provided by a translation agency and cross-checked by bilingual researchers from Swiss Paraplegic Research. For this, the guidelines for cross-cultural adaptation by Epstein et al. were followed [19]. Prior to data collection, participants received postal mailings with an invitation letter, study information, informed consent forms, a hard copy of the first module with a cover sheet including an individual study ID and a personal password for online completion, as well as a preprinted, addressed and postage-paid envelope to return the module. Participants who completed the online version were still asked to return the signed informed consent form. Based on experiences from the Survey 2012, reminder management was further optimized and only included one written reminder 4–6 weeks after delivery of the survey documents and one telephone reminder after an additional 4–6 weeks [18]. Persons who did not answer the phone after ten calls were coded as “no contact”. Recruitment, data collection, and data storage were performed according to standardized operational procedures.
Participants
Eligible for the Survey 2017 were all community-dwelling persons aged over 16 years with traumatic or non-traumatic SCI (e.g. degeneration of the spinal column, tumor, vascular problem, or infection) who were living in Switzerland at the time of the survey. We excluded people with congenital conditions leading to SCI (e.g. spina bifida), those with neurodegenerative disorders (e.g. multiple sclerosis or amyotrophic lateral sclerosis) and Guillain-Barré syndrome [5, 6].
Due to the absence of a central registry, a contact database was set up for the Survey 2012, based on records of Swiss Paraplegic Association members (SPA, the organization representing people living with SCI in Switzerland), patient records of ParaHelp (the specified home care organization for individuals with SCI in Switzerland) and patient records from 2005 to 2009 of three out of four specialized SCI rehabilitation centers in Switzerland [6]. This resulted in a Survey 2012 source population of 3807 individuals, of which 3144 fulfilled eligibility criteria, and is estimated to have covered over 50% of the estimated total Swiss SCI population (the estimated prevalence of SCI in the Swiss adult population with roughly 6.7 million inhabitants was 6000 persons in 2012) [6]. For the source population of the Survey 2017, the existing Survey 2012 database was supplemented with patient records of all four specialized SCI rehabilitation centers from 1967–2004 to 2010–2013, and 2005–2009 from the fourth specialized SCI rehabilitation center. From 2013 on, eligible individuals who were discharged from first rehabilitation and have lived for at least two years in the community were added to the contact database using information from the SwiSCI inception cohort, which covers individuals starting a first rehabilitation after SCI onset [5]. In addition, persons from the SPA and Parahelp who neither participated in the Survey 2012 nor appeared in the patient records in the centers were added. This resulted in a source population of 4493 individuals (n = 3959 persons who met eligibility criteria) who were invited to the survey. Considering the estimated prevalence of SCI in 2012, the coverage rate of the total Swiss SCI population was ~65%. Person names and contact details from all recruitment sources were cross-checked to avoid double contacting.
Ethics
The Survey 2017 has been conducted according to the ethical principles of the Declaration of Helsinki. The central ethical institution Ethikkommision Nordwest- und Zentralschweiz approved the study protocol. Participants were asked to sign an informed consent.
Descriptive analysis: survey participation and study population characteristics
Participation rates were calculated according to internationally accepted standards published by the American Association of Public Opinion Research [20] for the source population of Survey 2017 for both Survey 2017 modules and for participants who completed both core modules (modules 1 and 2) of the Survey 2012 and modules 1 and 2 of the Survey 2017. Participant characteristics included gender, age at time of completing the questionnaire (grouped into 16–30, 31–45, 46–60, 61–75, 76+ years), marital status (single, married/in partnership, widowed/divorced), years of education, years since SCI (≤5, 6–15, 16–25, 26+ years), SCI severity (incomplete paraplegia, complete paraplegia, incomplete tetraplegia, complete tetraplegia), and SCI etiology (traumatic vs non-traumatic). We used ISCoS-recommended cut-offs for age and years since SCI [21]. The information on SCI severity was either derived based on patient records (if available) or self-report. Survey characteristics, such as preferred language of communication (German, French, Italian) and response mode (online, paper, telephone/face-to-face interview) were additionally included in descriptive analysis. Proportions with 95% confidence intervals (CIs) were calculated for categorical variables, and medians with interquartile ranges were used to describe continuous variables.
Non-response analysis: determinants of non-response and inverse-probability weights for non-response correction
A similar analytic approach as used for the Survey 2012 was employed to identify determinants of non-response [6, 18]. Potential factors for non-response bias were analyzed using multivariable logistic regression to assess the likelihood to respond to the two Survey 2017 modules with reference to the eligible persons in the source population. To do so, we used data on gender, age, language, and SCI level, which represented the only information that was available for people recruited from the SPA and ParaHelp records and individuals recruited from the patient records of the specialized SCI rehabilitation centers. In a sensitivity analysis for the subset of people who participated in Survey 2012 and 2017, means of body and mental functions scores [22] and self-reported satisfaction with health from the Survey 2012 were compared between responders and non-responders of the Survey 2017. Corresponding inverse-probability weights (IPWs) were calculated based on the multivariable logistic regression and served as sampling weights to correct for survey non-response in subsequent analyses [6, 23, 24]. Missing data were imputed using a random forest procedure [25].
Impact of non-response bias on selected survey results
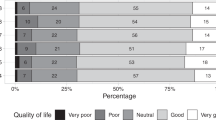
To determine the impact of possible non-response bias on associations studied, we investigated the effect of IPWs on the estimates of a selection of outcome variables representing different thematic areas of both Survey 2017 modules. The selection of these items was based on expert discussions and aligned with previous analyses for the Survey 2012 [6]. Differences in means and relative frequencies between the corrected (using IPWs) and uncorrected estimates were calculated with 95% CI using bootstrapping with 2000 replications. The following nine outcome variables were used: from module 1; marital status, years of education, employment status, and handbike use; from module 2; number of visits to any hospital or SCI-specialized center in the past year, number of days inpatient in any hospital or SCI-specialized center in the past year, quality of life (WHO-QoL BREF) sum score, ability to move from sitting at the side of the bed to lying down on the back, and confidence in one’s ability to get all the information needed to minimize complications.
Analyses were conducted using Stata SE 15.1 (College Station, TX, USA).
Results
Survey participation and study population characteristics
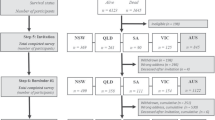
Figure 1 depicts the flow chart of study participation in relation to the source population of the Survey 2017. In total, 4493 persons were invited to participate, of whom 534 were not eligible, mainly because the person died before invitation (n = 146), contact mail was undeliverable (n = 144), person was double contacted (n = 113), or inclusion criteria was not met (n = 108), resulting in a final source population in 2017 consisting of 3959 persons. Of them, 1530 (38.6%) completed module 1 and 1294 (32.7%) module 2, which in absolute terms received 84.6% response. Of the 2429 non-participants in module 1, 1689 (69.5%) refused participation, and 740 (30.5%) could not be contacted. Of the 236 eligible non-participants in module 2, 198 (83.9%) refused participation and 38 (16.1%) could not be contacted due to lack of a valid phone number (n = 13), person did not answer the phone after ten calls (n = 18), or person died after having completed module 1 (n = 7). Of the 4493 invited persons, 1549 participated in the Survey 2012. Of these, 1332 were invited to the Survey 2017, of whom 1291 were eligible. Ineligibility was due to inclusion criteria not met (n = 17), died before invitation (n = 17), contact mail undeliverable (n = 3), double contacted (n = 1), or unknown reason (n = 3). Of the eligible persons of Survey 2012/2017, 761 (58.9%) individuals participated in module 1 and 685 (53.1%) in module 2, which in absolute terms received 90.0% response (Fig. 1—right side of the flow chart).
Percentages in circles within trapezoids indicate the cumulative response rate, in brackets the absolute response rate for the respective module. *Not eligible—unknown: the majority reported no SCI but brain injury. **Not eligible—other reason: n = 9 moved abroad, n = 6 recovered from SCI, n = 1 duplicate, n = 12 medical exclusion criteria, n = 10 contact mail undeliverable, n = 10 unknown. ***Not eligible—inclusion criteria not met: n = 6 moved abroad; n = 2 language difficulties; n = 6 medical exclusion criteria; n = 3 cognitive impairment.
Table 1 provides basic characteristics of the survey participants of Survey 2017 (column 1) and the participants in both Survey 2012 and 2017 (column 2), by modules 1 and 2, and the source population of Survey 2017 (column 3).
Determinants of survey participation and impact of IPWs on selected survey results
Table 2 details the results of the multivariable logistic regression. For the source population for Survey 2017, less people in the age group 76+ years (OR: 0.8; 96% CI: 0.6–1.2 for module 1) as well as females (OR: 0.9; 95% CI: 0.8–1.0 for module 1) and those with tetraplegia (OR: 0.9; 95% CI: 0.8–1.0 for module 1) responded to the survey. For the Survey 2012/2017 subgroup, more people in the age group 61–75 years compared to the remaining age groups (OR: 2.3; 95% CI: 1.5–3.8 for module 1) and less people with tetraplegia compared to those with paraplegia (OR: 0.8; 95% CI: 0.7–1.0 for module 1) responded the 2017 survey. Sensitivity analysis showed no differences in means between the body and mental functions scores and self-reported satisfaction with health between responders and non-responders for the Survey 2012/2017 subgroup (data not shown).
The IPWs ranged from 0.8 to 1.6 (module 1) and from 0.8 to 1.7 (module 2) for the source population for Survey 2017, and from 0.7 to 2.3 (module 1) and from 0.7 to 2.6 (module 2) for the Survey 2012/2017 subgroup (Table 3). The mean difference between the uncorrected and corrected point estimates ranged from −0.9 (95% CI: −1.2 to −0.6 for % widowed) to 1.2 (95% CI: 0.8–1.5 for % in paid work) for the source population for Survey 2017 characteristics. For the Survey 2012/2017 subgroup mean differences ranged from −1.1 (95% CI: −1.8 to −0.4 for % widowed) to 1.3 (95% CI: −0.4 to 3.0 number of inpatient hospitalization in past year).
Discussion
The present study provides information on the methodology, recruitment results and participants and non-participants of the Survey 2017. Although response rates were lower than for Survey 2012, the Survey 2017 design was successful in sampling a substantial proportion of the source population with an estimated coverage rate of 65% of the adult SCI population in Switzerland. The likelihood of survey non-response was greater among those aged 76 years or older, females, and those with tetraplegia. The small differences between corrected and uncorrected point estimates for selected outcome variables point toward a marginal non-response bias.
A drop in response rates from Survey 2012 to 2017 (from 49.3 to 38.6%) may be related to differences in the composition of the source population between 2012 and 2017. In the Survey 2012, eligible persons were identified from different sources including patient records from 2005 to 2009 to build up a representative source population for the Survey 2012. In 2017, the existing SwiSCI cohort was supplemented with contact addresses from patient records from before 2005, of which some were dating back to the 1970s’. The high “no contact” rate (more than twice as high compared to Survey 2012) may be caused by outdated contact addresses from old patient records, or by deaths. Moreover, the high refusal rates in our study are in line with a general trend of high refusal rates observed in general population survey research, in particular for online surveys and cell phone interviews [26, 27]. In a systematic review, various ways to increase response rates in postal and electronic questionnaires were examined, and both operational and content-specific aspects of a questionnaire survey, such as pre-contacting people before sending the questionnaire, use of a stamped-return envelope, offering incentives, or using reminders, while keeping the questionnaire short and interesting, turned out to be effective to increase response rates [28]. The response rates for the Survey 2017 are comparable to the ones for community surveys on SCI populations worldwide, as for example, the response rates for the InSCI community survey, ranging from 23 to 54% [16]. The higher response rates in the Survey 2012/2017 subgroup are in line with previous reporting on response rates in follow-ups of cohort studies [29]. Optimizing the length and content of the SwiSCI modules and communication strategy of SwiSCI findings and their benefits to persons living with SCI may additionally increase response rates in future SwiSCI community surveys.
The likelihood of non-response was greater among the oldest and those with tetraplegia, and women for module 1 in the source population for Survey 2017. It is a well-known phenomenon that persons with higher age are frequently found among survey non-responders; usually due to their multitude of health problems paired with lower socioeconomic status as well as attitudinal and motivational factors [30]. Regarding lesion level, we can only speculate why there was a difference in response rates. Reasons for non-response may be related to the specific items of the modules, or fatigue feared as a result of completing a long questionnaire. Similarly to the Survey 2012, the non-response bias in the Survey 2017 appears to be marginal [6]. Of note, there is still no registry with information on the entire adult Swiss SCI population, which makes it difficult to draw conclusions about the relationship of sociodemographic and SCI characteristics with survey participation. Comparison with the similar Canadian SCI community survey [2] shows comparable distribution of sociodemographic and SCI characteristics, while comparison with the US SCI model systems data shows a higher proportion of single persons (US: 49% [1-year post-injury] to 40% [10-years post-injury] vs Switzerland: 24.5%) and a rising proportion of people with incomplete tetraplegia in the USA (from 28% in the 1960s to 42% in the mid-2010s) compared to 22% in Switzerland [30]. Of note, the SCI model systems database only enrolls people with traumatic SCI, which may limit the comparability to our participants. Also, differences captured in these figures are most likely due to different socioeconomic and healthcare conditions and only related to a fraction of the target population [2, 6, 31]. Finally, it is noteworthy that body function and mental health scores as well as satisfaction with health did not differ between survey responders and non-responders of the source population for Survey 2012 and 2017, which indicates that persons with poorer health ratings were not more frequently among the non-responders in the Survey 2017.
Strengths and limitations
A major strength of Survey 2017 is its broad sampling frame with the inclusion of individuals from all SCI-specialized rehabilitation centers, a large patient association and home care organization, resulting in a source population with almost 4500 persons with more than 1500 responders to the Survey 2017. However, the representativeness of the source population of the target population remains unknown, in particular because prevalence and patient characteristics of people with SCI have not been systematically assessed in Switzerland. Using the crude prevalence estimate of 6000 persons with SCI, participation to the Survey 2017 module 1 represented at least 25%. Plans for the future comprise the inclusion of acute care hospitals to generate a population-based sampling frame for the SwiSCI community survey.
Moreover, the present non-response analysis is based on a minimal set of available demographic and SCI characteristics, which does not include social, cultural and personal determinants that may be paramount for survey response behavior. The selection of variables was determined by feasibility issues, given that only a limited set of variables were available on non-responders due to logistical challenges and legal restrictions in using data of those not consenting to a study. The lack of additional data about the non-responders hindered a more detailed non-response analysis. This limitation has been reported in other studies too [29]. Thus, any future SwiSCI data analysis on social, cultural and personal determinants could be prone to response bias. Also, the notion of negligible survey non-response bias strictly refers to the invited population, potentially missing those with reduced access to rehabilitation who were never seen by the specialized centers nor became members of the patient organization.
Conclusion
By providing information on the methodology, recruitment results and the study population of the Survey 2017, the present study offers a useful reference for analyses using Survey 2017 data. Albeit lower than those of the Survey 2012, response rates were comparable to other international community surveys. Our non-response analysis, which was based on a minimal set of available sociodemographic and SCI characteristics of the source population, pointed towards a marginal non-response bias.
Data availability
Owing to our commitment to SwiSCI study participants and their privacy, datasets generated during the current study are not made publicly available but can be provided by the SwiSCI Study Center based on reasonable request (contact@swisci.ch).
References
Bach M, Jordan S, Hartung S, Santos-Hovener C, Wright MT. Participatory epidemiology: the contribution of participatory research to epidemiology. Emerg Themes Epidemiol. 2017;14:2.
Noreau L, Noonan VK, Cobb J, Leblond J, Dumont FS. Spinal cord injury community survey: a national, comprehensive study to portray the lives of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20:249–64.
Savic G, Charlifue S, Glass C, Soni B, Gerhart K, Jamous A. British ageing with SCI study: changes in physical and psychosocial outcomes over time. Top Spinal Cord Inj Rehabil. 2010;15:41–53.
Chen Y, DeVivo MJ, Richards JS, SanAgustin TB. Spinal cord injury model systems: review of program and national database from 1970 to 2015. Arch Phys Med Rehabil. 2016;97:1797–804.
Post MW, Brinkhof MW, von Elm E, Boldt C, Brach M, Fekete C, et al. Design of the Swiss Spinal Cord Injury Cohort Study. Am J Phys Med Rehabil. 2011;90:S5–16.
Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A. Swiss national community survey on functioning after spinal cord injury: Protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
Paneth N, Monk C. The importance of cohort research starting early in life to understanding child health. Curr Opin Pediatr. 2018;30:292–6.
Mitchell S, Ciemnecki A, CyBulski K, Markesich J (editors). Removing barriers to survey participation for persons with disabilities. 1st ed. Rehabilitation Research and Training Center on Disability Demographics and Statistics, Ithaca, NY: Cornell University; 2006.
Parsons JA, Baum S, Johnson TP, Hendershot G. Inclusion of disabled populations in interview surveys: review and recommendations. In: Barnartt SN, Altman BM, editors. Exploring theories and expanding methodologies: Where we are and where we need to go, vol. 2. Bingley: Research in Social Science and Disability, Emerald Group Publishing Limited; 2001. p. 167–84.
Eisner NL, Murray AL, Eisner M, Ribeaud D. A practical guide to the analysis of non-response and attrition in longitudinal research using a real data example. Int J Behav Dev. 2019;43:24–34.
Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17:643–53.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Cieza A, Kirchberger I, Biering-Sorensen F, Baumberger M, Charlifue S, Post MW, et al. ICF Core Sets for individuals with spinal cord injury in the long-term context. Spinal Cord. 2010;48:305–12.
Prodinger B, Cieza A, Oberhauser C, Bickenbach J, Ustun TB, Chatterji S, et al. Toward the International Classification of Functioning, Disability and Health (ICF) Rehabilitation Set: a minimal generic set of domains for rehabilitation as a health strategy. Arch Phys Med Rehabil. 2016;97:875–84.
Geyh S, Muller R, Peter C, Bickenbach JE, Post MW, Stucki G, et al. Capturing the psychologic-personal perspective in spinal cord injury. Am J Phys Med Rehabil. 2011;90:S79–96.
Fekete C, Brach M, Ehrmann C, Post M, InSCI, Stucki G. Cohort profile of the International Spinal Cord Injury (InSCI) Community Survey implemented in 22 countries. Arch Phys Med Rehabil. 2020. https://doi.org/10.1016/j.apmr.2020.01.022.
The SwiSCI Community Survey. 2017. https://swisci.ch/en/research-projects-home/study-design/community-survey.
Fekete C, Segerer W, Gemperli A, Brinkhof MW. Participation rates, response bias and response behaviours in the community survey of the Swiss Spinal Cord Injury Cohort Study (SwiSCI). BMC Med Res Methodol. 2015;15:80.
Epstein J, Osborne RH, Elsworth GR, Beaton DE, Guillemin F. Cross-cultural adaptation of the Health Education Impact Questionnaire: experimental study showed expert committee, not back-translation, added value. J Clin Epidemiol. 2015;68:360–9.
The American Association for Public Opinion Research. 2016. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed. AAPOR. https://www.aapor.org/Publications-Media/AAPOR-Publications.aspx.
Hinrichs T, Prodinger B, Brinkhof MW, Gemperli A. Subgroups in epidemiological studies on spinal cord injury: evaluation of international recommendations in the Swiss Spinal Cord Injury Cohort Study. J Rehabil Med. 2016;48:141–8.
Prodinger B, Ballert CS, Brach M, Brinkhof MW, Cieza A, Hug K, et al. Toward standardized reporting for a cohort study on functioning: the Swiss Spinal Cord Injury Cohort Study. J Rehabil Med. 2016;48:189–96.
Harrod LA, Lesser V. The use of propensity scores to adjust for nonignorable nonresponse bias. Proc Am Stat Assoc. 2006: 3109–12.
Peress M. Correcting for survey nonresponse using variable response propensity. J Am Stat Assoc. 2010;105:1418–30.
Stekhoven DJ, Buhlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28:112–8.
Pedersen MJ, Nielsen CV. Improving survey response rates in online panels: effects of low-cost incentives and cost-free text appeal interventions. Soc Sci Comput Rev. 2016;34:229–43.
Dutwin D, Loft JD, Darling JE, Holbrook AL, Johnson TP, Langley RE, et al. Current knowledge and considerations regarding survey refusals: executive summary of the AAPOR Task Force Report on survey refusals. Public Opin Q. 2015;79:411–9.
Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009:MR000008.
Nohr EA, Liew Z. How to investigate and adjust for selection bias in cohort studies. Acta Obstet Gynecol Scand. 2018;97:407–16.
Rodgers WL, Herzog R. Collecting data about the oldest old: problems and procedures. In: Suzman RM, Willis DP, Manton KG, editors. The oldest old. New York: Oxford University Press; 1992. p. 135–56.
National Spinal Cord Injury Statistical Center. 2019 annual statistical report for the spinal cord injury model systems. Birmingham, Alabama: University of Alabama at Birmingham; 2019. https://www.nscisc.uab.edu.
Acknowledgements
We thank the SwiSCI Steering Committee with its members Xavier Jordan, Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger, Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis, Kerstin Hug (REHAB Basel, Basel); Laurent Prince (Swiss Paraplegic Association, Nottwil); Heidi Hanselmann (Swiss Paraplegic Foundation, Nottwil); Daniel Joggi (Representative of persons with SCI); Nadja Münzel (Parahelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Armin Gemperli (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Funding
SwiSCI is hosted and funded by Swiss Paraplegic Research.
Author information
Authors and Affiliations
Contributions
MHGH, AG, CF, and US were responsible for conceptualization of the analysis. MHGH and AG were responsible for data analysis and interpretation of results. MHGH wrote the first draft of the manuscript and all authors (AG, CF, US, MB, GS) worked on, reviewed, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was granted by the leading ethical institution Ethikkommision Nordwest-und Zentralschweiz (EKNZ, Project-ID: 11042 PB_2016-02608, approved Dec 2016). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gross-Hemmi, M.H., Gemperli, A., Fekete, C. et al. Methodology and study population of the second Swiss national community survey of functioning after spinal cord injury. Spinal Cord 59, 363–372 (2021). https://doi.org/10.1038/s41393-020-00584-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00584-3
This article is cited by
-
Use of professional home care in persons with spinal cord injury in Switzerland: a cross-sectional study
BMC Health Services Research (2023)
-
Australian arm of the International Spinal Cord Injury (Aus-InSCI) community survey: 1. population-based design, methodology and cohort profile
Spinal Cord (2023)
-
Does the socioeconomic status predict health service utilization in persons with enhanced health care needs? Results from a population-based survey in persons with spinal cord lesions from Switzerland
International Journal for Equity in Health (2022)
-
Pathways to loneliness: a mediation analysis investigating the social gradient of loneliness in persons with disabilities in Switzerland
International Journal for Equity in Health (2021)
-
First contact of care for persons with spinal cord injury: a general practitioner or a spinal cord injury specialist?
BMC Family Practice (2021)