Abstract
Study design
Qualitative descriptive study with inductive thematic content analysis.
Objectives
To explore how individuals living with paraplegia in South Africa experience sex and intimacy and how they perceive the related health services and support they received whilst adapting to life post injury.
Setting
Community based in Cape Town, South Africa.
Methods
Purposive and snowball sampling were combined to enrol ten individuals with paraplegia who were all users of the public health system and had been injured for more than 1 year. Semi-structured interviews were conducted, and data analysed using inductive thematic content analysis.
Results
Four categories were derived and captured by the overarching theme of ‘a journey to reclaiming sexuality’, as depicted by each participant. Psychological consequences of the injury led to challenges with sex and intimacy including a strong emphasis on partner satisfaction. A perceived lack of support mechanisms particularly in relation to poor timing of health services and insufficient peer support led to a lack of understanding and difficulties adjusting to changes in sexual function. Meaningful relationships including elements of sex and/or intimacy were rediscovered following a re-adjustment period although participants often felt disabled by society as socio-cultural norms, such as gender concepts, influenced each individual journey.
Conclusions
Complex interactions between intrinsic psychological factors, such as low sexual self-esteem and external factors such as socio-cultural norms, affect sex and intimacy in individuals with paraplegia in this novel context. South Africa’s health system should be strengthened to support optimal sexual outcomes of persons with a spinal cord injury.
Similar content being viewed by others
Introduction
Sexuality is a fundamental aspect of human existence, encompassing a broad range of facets and includes both physical and emotional characteristics of being [1]. Whilst sex or sexual function is commonly described in the literature in terms of heteronormative penetration it goes beyond this narrow realm [2]. Likewise, intimacy is believed to include, but is not limited to, aspects of affection, cohesion and expressiveness, rather than sexuality alone [2]. The American Occupational Therapy Association recognises sex and intimacy as an activity of daily living [3] and the World Health Organisation acknowledge that the sexual needs of people with disabilities must be met as a basic human right [4]. Sexual function is frequently impaired following spinal cord injury [5, 6] and consequently, a number of emotional and psychological challenges exist [7, 8].
In the global arena, many studies are emerging due to a growing interest in sexuality within the context of spinal cord injury, yet the focus is largely on physiological changes such as erectile dysfunction [6] and research is predominantly conducted in high income countries, thus low- and middle-income settings are trailing behind [9]. These less affluent settings are typically characterised by a lack of high-quality specialised services with fewer available resources, which inherently affects health outcomes of a population [10]. Furthermore, little attention has been paid to intimacy or related emotional well-being despite the fact that sexuality continues to be rated of paramount importance for those living with a spinal cord injury [8, 9, 11]. For those with paraplegia level injuries in particular this has been stressed as the top functional priority [11]. Understanding the experiences and challenges of persons with spinal cord injury in relation to sexuality and intimacy is paramount for the development of holistic, multifaceted interventions in promoting optimal sexual function.
Verschuren et al. offer a non-linear conceptual framework for exploring sexuality in the context of disability [12]. This framework highlights interplay between five main components (the disability, physical condition, psychological well-being, relationships and sexual function/well-being) affecting sexuality, as well as suggesting more subtle aspects to consider, e.g. medication compliance and acceptance. Although not developed specifically developed for use within the field of spinal cord injury it can be used here as a basis for exploring and understanding how individuals are affected given the known physiological and functional changes which occur. Further, the framework provides a context in which to frame the study.
Spinal cord injury is a notable public health problem in South Africa, with an incidence rate of ~76 per million [13], around three times that of the estimated global rate [14]. Injuries are predominantly due to violence, with males around 18–30 years from lower socio-economic backgrounds at the forefront of this group [13]. These injuries fall within the ‘violence and injuries’ category which alongside HIV/AIDS and tuberculosis, non-communicable diseases and maternal and child health form the country’s quadruple burden of disease [15]. Whilst research in this setting is growing, little is known about the sexual needs of this group, a particularly important topic given that injuries are frequently sustained during the developmental period of peak sexuality. With this in mind, the aim of the study was to explore how individuals living with paraplegia in South Africa experience sex and intimacy and how they perceive the related health services and support they received whilst adapting to life post injury.
Methodology
Setting
This study was conducted in the Cape Town metropolitan, Western Cape province, South Africa. South Africa has been classified as an upper middle-income country by the World Bank and is characterised by extreme wealth inequalities. Around 84% of South Africans, predominantly from lower socio-economic groups, are believed to use the overburdened public health system [16]. The Western Cape Rehabilitation Centre is the sole public sector specialist service within the province; however, not all survivors of spinal cord injury are treated here due to limited resources, thus the remainder either receive generic outpatient rehabilitation or none at all. Length of stay at the rehabilitation centre is around 10 weeks for those with paraplegia. During this time one formal mixed gender session of sex education is provided by social workers; primarily from a functional perspective. Private sessions are possible but individuals most often initiate this themselves.
Study design and participants
A qualitative descriptive approach was used allowing for a full and detailed descriptive summary of events, with phenomena unfolding naturally due to minimal manipulation [17]. This approach thus permitted broad exploration of how sexuality is experienced by persons living with a spinal cord injury in an undiscovered context, which is unique in a number of ways. Given the sensitivity of the topic this design further provided a way to reach some kind of true understanding of participants’ processes and to present the phenomena with low levels of interpretation. Purposive sampling was used initially, following principles of maximum variation (with respect to gender, age, time since injury and lesion level) to identify participants from the Western Cape spinal injury database compiled by a research group. Participants were recruited via telephone due to setting constraints, e.g. irregular email use, and the following inclusion criteria adhered to:
-
(1)
Community dwellers within the Cape Town metropolitan.
-
(2)
Paraplegia grade A-D, as defined by the American Spinal Injury Association Impairment Scale [18].
-
(3)
Injured for >1 year.
-
(4)
Previously treated within the public health system.
Due to logistical challenges, e.g. incorrect contact details, plus participants either declining participation or withdrawing prior to the interview, purposive sampling was complimented by snowball sampling from initial participants in order to recruit the desired number of participants. Sample size was guided by both data saturation and the concept of information power [19]; the latter being a relatively new concept concerning how ‘powerful’ the sample is. In relation to this study we believe, for example, the aim to be focussed, with a relatively homogenous group of participants and the quality of interview dialogues high given the way in which participants generously shared their perspectives. Table 1 presents basic characteristics of the participants with specific details removed to protect identities. Most participants were males from lower socio-economic groups having sustained a violence related injury an average of 12.5 years ago.
Data collection
Individual semi-structured interviews were conducted; nine face-to-face and one telephonically (due to health and safety reasons). Participants living in areas deemed unsafe either by the researchers or participants, came into the University of the Western Cape whilst others were given a choice of interview location. This resulted in four interviews at participants’ homes, two at work places and three at the university. Interviews ranged from 29 to 70 min in length with travel costs reimbursed where relevant. Verschuren’s framework was used as a basis for the interview guide that was developed by three of the authors and topics covered (1) the meaning of sex and intimacy, (2) intimate relationships, (3) support systems and (4) perceived challenges. Examples of questions can be found in Table 2. Three pilot interviews were conducted and changes made according to data quality and participant guidance. Alterations included more positively framed questions, increased use of silent probes and ensuring an optimal environment for conducting interviews of a sensitive nature.
Each interview was conducted, audio-recorded and transcribed verbatim by CT, an English occupational therapist. Participants chose to be interviewed in English; however, two regularly expressed themselves in Afrikaans which was translated in real time by a South African research assistant. Trustworthiness processes informed by Lincoln and Guba [20] included researcher immersion in the context and an audit trail, and member checking was performed both during and post interviews to check details and discuss concepts. Participants were informed of the study background and objectives prior to the interview and every effort was made to build rapport and create an open environment, with the opportunity for participants to ask questions and have some time for ‘free comments’ at the end. Despite the topic sensitivity and the primary interviewer originating from a different setting, participants appeared extremely open and humble in their responses, revealing personal details and often stating that they were happy to have the opportunity to discuss sexuality. Discussions between authors were held throughout the interview process to clarify meaning and consider arising phenomena as well as co-investigator debriefing sessions including discussions concerning pre-conceptions. Field notes plus supporting information from notes taken during discussions with social workers and therapists at Western Cape Rehabilitation Centre concerning sexual rehabilitation processes and session contents have aided with triangulation of data. Diverse backgrounds of those involved in the project (occupational therapy, physiotherapy, public and global health, from high- and middle-income settings) allowed for in-depth discussions and conceptualisation from different perspectives and through an allied health lens.
Data analysis
Thematic content analysis [21] was used beginning with data familiarisation through repeated reading and open coding of transcripts. All transcripts were scrutinised by CT and five were examined by CJ and LB. Descriptive summaries of each case were produced and compared across the interviews in order to contrast experiences and uncover patterns amongst participants’ responses. Meaning units were next identified and condensed (e.g. ‘have to empty bladder for intimacy’) and then labelled with a data driven code (e.g. ‘bowel and bladder’), of which similar ones were merged in order to reduce volume. All codes were developed inductively and entered into NVivo 12.3.0 software for assistance with management and analysis. Grouping of similar codes resulted in 14 sub-categories, and 4 final categories were established following numerous in-depth discussions between the researchers.
Results
‘It’s been quite a journey, honestly, it’s been quite a one’ (female, thoracic lesion).
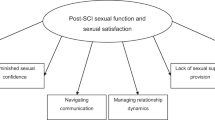
Most participants tended to refer to sex rather than sexual function and this was defined by participants as a physical act of intercourse. Four categories were derived and embodied by the overarching theme of a journey to reclaiming sexuality, as presented in Fig. 1. Perspectives of intimacy were euphemistic, still referring to intercourse and thus not including broader concepts such as emotional connection. Participants each described their journey of various challenges, yet many went on to suggest fulfilment in relationships once barriers had been overcome. Alongside frustration with healthcare services, strong socio-cultural elements such as gender norms and beliefs surrounding disability were evident throughout the findings and responsible for certain behaviours; these factors continuously influencing the experience of each depicted journey. Quotations have been selected to represent a range of voices, however limited demographic information is provided so as to eliminate risk of participant identification.
Psychological consequences
All participants identified intrinsic psychological barriers arising from the physiological changes resulting from injury. These findings revealed that participants feared rejection from their partner as well as experiencing a lack of confidence sexually and sexual self-esteem.
Incontinence during sex was described as leaving participants feeling embarrassed and put-off; this lack of bladder and bowel control was at the heart of both females’ responses, ‘I think that is the only problem, the intimate story when you make an accident…we would literally have sex and I wanna poo poo…. ‘you can’t, I must stop everything now, I have to go to the toilet because if I don’t I’m gonna do it on the bed’….stuff like that man, not only the pee story…. that’s the only damn put off about this wheelchair story!’ (female, thoracic lesion).
Erectile dysfunction dominated many of the males’ responses and the effect of not being able to sustain an erection had profound consequences, as highlighted by this participant ‘…it’s like er, puts you down if you can’t last long enough’(male, thoracic lesion) and one referred to the erection as ‘the most sensitive part in, in, a paraplegics’ life’ (male, thoracic lesion). This inability to maintain an erection appeared to dominate some individuals’ lives and the negative impact of an inability to ejaculate was frequently alluded to. Participants described feeling more content once they took steps to overcome erectile difficulties.
A strong focus on partner satisfaction was evident for both genders, ‘now it’s a priority, I must do it, I must keep me on tune’ (female, thoracic lesion) and this was coupled with a fear of rejection, as one participant put it, ‘when a paraplegic dates a woman or get married…., then she maybe don’t get satisfied enough and she moves on. You know she leaves that guy. There’s many, many paraplegics I know that got married, that wives left them because of that’ (male, thoracic lesion). Alongside this, a lack or loss of sensation led to insecurities around underperforming and uncertainty around having an orgasm. This in turn led to comparisons with non-disabled counterparts for some.
Perceived lack of support systems
Unsurprisingly, a lack of both systemic support and social support networks had a negative effect on reclaiming sex and intimacy. A proactive approach was often necessary to enhance sexuality focussed support, and many described how they were only supported when they sought assistance, suggesting that those who were more passive recipients of care were likely to miss out.
Infertility was a fundamental stressor for most men and many expressed that support was inadequate in terms of highlighting infertility risks and consequences during the early days of injury. One of them described the sadness upon discovering he would not be able to have children, ‘there’s one thing I sit with [on his mind], I was thinking if he had told me this like, maybe 15 years ago then I think that I would have done that, to just go throw, the sperm out, freeze it and, keep it in a sperm bank until I’m ready, you know?… But now it’s a bit, very difficult for me’ (male, thoracic lesion). Accessing fertility investigations and treatment proved challenging unless they were able to afford private healthcare, which is likely impossible given the low socio-economic nature of the cohort.
Common complaints regarding health service provision related to poor timing of services, inadequate support and a lack of knowledge amongst professionals. Many expressed that sex and intimacy was not a priority for them during the rehabilitation phase, as one put it, ‘I don’t wanna have sex now man, I wanna walk’ (female, thoracic lesion). Likewise, even if they attended the sex education session it was not necessarily experienced as being meaningful at that time. Most participants described feeling isolated and left to their own devices after hospital discharge with no community follow up, although they would have likely benefitted from more support. As one participant explained, ‘in relation to sex I would have loved at least to have had someone maybe talk, guided me and have been able to speak to me openly in terms of spinal cord injury …. the expectants of what it is, what is sex, what’s intimacy, what should I expect, what should I not expect, coz those are the things I didn’t really get’ (female, thoracic lesion). Further, they often blamed themselves for what appeared to be systemic faults.
Peer support and its significance were highlighted by all participants, providing a source of connection, value and empowerment. Yet a sense of a lack of both formal and informal peer support was evident, perhaps even more so once back in the community. Any existing peer support came in the form of informal networks, chance encounters or via mutual contacts thanks to the closely-knit spinal cord population in the Cape Metropolitan, with some also finding solace within social media. Participants explained how it was easier to talk to someone in a similar situation, ‘it makes it easier to, to open up with, with someone that’s…. also has a spinal cord injury, so it definitely was easier to communicate with her because she will have a better understanding…. than someone without the injury’ (female, thoracic lesion). At the time the interviews took place it appeared that any pre-existing formal peer support at the rehabilitation centre was now non-existent.
Disabled by society
All participants alluded to experiences strongly linked to public views in South Africa on disability and sexuality, often leaving them feeling isolated and despondent. Changing the societal mindset was seen as a major challenge that lies ahead. Many participants remarked on the prevailing belief within society that people with disabilities are asexual, ‘like I said they don’t think that if you’re in a wheelchair you can still have sex’ (male, thoracic lesion) viewing it as an extra factor to face on top of an already life changing event. One participant even recalled how a family member told her that disabled people should not enjoy pleasure in the same way non-disabled people do.
Ideals of masculinity were woven into findings, driving participants’ perceptions of sex and intimacy, with frequent reference to erections and ejaculation defining a man. ‘In the area and society that I grew up, being a young man who is good on satisfying a woman was the, was what makes you the man’ (male, thoracic lesion). Whilst women found that they had to have sex to prove they were ‘still a woman’. A number of participants emphasised that sexuality is not openly discussed as they felt South African culture to be somewhat conservative, presenting them with challenges to talk freely. At the same time, many feared being gossiped about within the immediate community, ‘…you know people in our society, people will always talk’ (female, thoracic lesion), hence some even disclosed sensitive information during the interviews which they had never explicitly discussed with their partner.
Moving towards meaningful relationships
Despite a long journey filled with challenges, all participants were in a meaningful relationship at the time of interview even if they were not all sexually active. High importance was placed on accepting the consequences of spinal cord injury and being open and honest with a partner. Many participants described aspects of intimacy other than just physicality even if they did not formally define it that way, and further often described a shift from casual sex pre injury to more stability in current relationships.
For most, having accepted the consequences of injury and adjusted to a new routine, the opportunity to re-focus on sexuality arose, and this normally took place around 1 year or so post injury. ‘After um, doing a lot of questioning with regards to my injury and then I, as soon as I…..realised that, it doesn’t matter what you’re gonna do here now, you’re screwed! You know? You’re toasted. And that’s when I said ok, as long as I can have sexual intercourse and I can be with someone when I feel like being with someone, I’m good’ (male, thoracic lesion). Over time the meaning and importance of sex and intimacy changed, and after some years it was often viewed as a normal part of life again. A number of participants even suggested they were now ‘better lovers’ than prior to their injury.
One of the key elements to sustaining a relationship appeared to be open and honest communication, even if not always easy. One participant reflected on openness as a two-way process, ‘….depends on the person that you’re dating or the person that you’re sleeping with… you might wanna be open and honest but there’s certain things that you really can’t be 100% open with and you’ll be like ok, you will see as things have been, then you will take it from there of how somebody’s going to react….. you need to be both clear and understanding and you need to know what you’re both getting yourself into’ (female, thoracic lesion).
Discussion
The aim of this study was to explore how individuals living with paraplegia in South Africa experience sex and intimacy and how they perceive the related health services and support they received whilst adapting to life post injury. Each journey to reclaiming sexuality was strongly shaped by a range of interlinked factors, but perhaps most strikingly so by participants’ experiences within the healthcare system and the influence of the society they live in. Whilst the meaning of sex and intimacy had changed to some degree, regaining sexuality was considered important on many levels; for individual well-being, for building meaningful relationships and to a certain extent, feeling ‘normal’ again.
The consequences of both erectile dysfunction and incontinence during sexual activity were profound in this study and echoes that of similar research conducted in high- or middle-income settings [6, 22]. Gomes et al. found that whilst many predictors of an active sex life exist, male erectile function is the only one related to perceived satisfaction with sex life [22], which likewise reflects views and feelings of some participants in this study. Fear of rejection and low sexual self-esteem may well stem from an inability to perform as before or in comparison with others, and vice versa; as Robinson et al. suggest self-esteem and sexual function are closely connected in this South African setting [23]. Further, this low self-esteem can affect engagement levels during rehabilitation [7, 23] and is likely perpetuated by societal norms. Perceived partner satisfaction in this study appears to determine sexual adjustment and well-being and echoes other findings [7, 8], however, the actual perspectives of the partners are not known.
Levels of knowledge concerning infertility amongst men in this study were strikingly low, often characterised by asking the interviewer questions on the topic. This indicates evidence of poor health literacy, a trait commonly observed amongst those from low socio-economic backgrounds [24], and a system not understanding or supporting their needs. Given that sperm quality is thought to diminish rapidly in the first 2 weeks following injury [25], the option to freeze sperm early on is a justified approach for fertility management [26]. However, this is not necessarily feasible given the overburdened public health system, scarce resources, and disparities in accessing healthcare [27].
The perspectives of those in this study mirrored Fisher et al.’s findings [8] relating to a period of decreased interest in sexual activity directly after the injury whilst accepting and adapting to new circumstances, followed by a renewed interest later on. They found this to be around six months post injury in the United States [8] yet here interest in sex and intimacy generally recurred after at least 1 year. What is unknown, however, is whether it was always on participants minds early on post injury but just took less priority or whether they did not even consider it until much later on in their journey. Considering the context, it may take longer to address basic physiological and safety needs post injury due to environmental constraints, e.g. inappropriate housing. Interventions in South Africa may thus be well suited to the community setting, in addition to acute services.
Communication was a clear driver for many in the present study for building and maintaining intimate relationships. Saxton [28] even found that meeting with a peer offers individuals with disabilities a unique opportunity to improve communication with their partners, encouraging them to push their boundaries and strengthening relationships further. Those struggling to communicate with their partner in an open and honest way, particularly in relation to incontinence, were identified not only here but also by Braaf et al. [29]. Yet, some participants in this study, and similarly in Ostrander’s review [30], found the injury actually gave them the opportunity to become better lovers. This suggests that for those individuals who were able to find a way to express their sexual needs this resulted in a deeper relationship with their partner, with a sound understanding of each other’s needs and desires.
Participants largely focussed on heteronormative penetrative sex and an inability for men to reach orgasm could lead to their masculinity being challenged [30]; non-adherence to these masculine scripts may well lead to psychological damage [6]. The initial willingness of participants who then later withdrew, and the fact that some declined participation from the outset suggests individuals are likely influenced by societal norms and a discomfort in discussing the topic. This pertinent point is perhaps unsurprising given the existing hegemonic masculinity in this setting, with sexual prowess as a status symbol and peer pressure surrounding the number of sexual partners [31]. As Sakellariou reflects, it is the societal impact which impinges on sex and intimacy, not the impairment per se [32] and these socio-cultural norms appear to add to the intensity of the aforementioned experiences in this study.
The importance of the social environment has been a salient finding in this study, including formal and informal support systems, yet dissatisfaction with in-patient sexuality support was evident and is consistent with findings from other studies globally [6, 23, 30]. A sense of loneliness in confronting changes in sexuality post injury has been revealed, partly illustrated by confiding in the researcher. However, this study does demonstrate a noticeable resilience amongst participants and an ability to find their own coping mechanisms, re-engaging in sex and intimacy once again.
The value of peer support after spinal cord injury has been well documented, particularly for dealing with emotional concerns and self-identity [7, 23, 28, 33, 34], likewise here it was deemed to empower individuals and enhance self-efficacy when facing topics of a sexual nature. We believe support of this kind to be especially powerful in South Africa due to the effect of the aforementioned socio-cultural norms and individuals feeling isolated in dealing with their condition; Sharma et al. revealed similar findings in the Indian context [9]. Furthermore, peer support may help improve health literacy amongst those in lower socio-economic settings [35]. Whilst some informal networks exist in Cape Town, one of the biggest concerns is the lack of formal peer support currently in place, especially post discharge and those who are less proactive or have more barriers in place miss out on the abundant benefits.
Finally, the importance of theoretical frameworks and models cannot be disputed. Whilst Verschuren’s framework is useful for considering the impact of disability on sexual well-being and functioning [12], no emphasis is placed on socio-cultural factors, and limited focus on social support mechanisms; both of which were extremely influential in this study. A more holistic framework taking these factors into consideration would be beneficial for both researchers and clinicians in South Africa as well as other settings.
Limitations and recommendations
Due to the nature of this study, findings cannot be transferred to all persons living with a spinal cord injury; however, comparable findings may be uncovered in similar cohorts within similar contexts. All participants were in a relationship and the majority had been injured for many years, thus recall bias cannot be eliminated. Whilst participants appeared able to remember earlier challenges of the injury, a future longitudinal study would give insight into which obstacles are most pertinent and when. A study including those not in stable relationships, either by choice or circumstance, and considering perceptions of sexuality early on in injury would provide more depth, as would including voices of those living with tetraplegia. Insight into the perspective of those who have been treated within the private health service would enable some comparison between the health systems and provide a fuller picture of circumstances in South Africa. Further, examining partners’ and healthcare professionals’ stances on this topic could help provide more optimal sexual support.
Implications of this research
The development of public health services for people with spinal cord injuries is crucial with respect to structured peer support, person-centred approaches, open environments and accessible services at both in-patient and outpatient level. All men would benefit from early education about infertility. Lastly, there is a need to break down mis-conceptions regarding sexuality and disability within society as whole.
Conclusion
This study revealed that complex interactions between psychological factors such as low sexual self-esteem, a lack of formal support from health services and the influence of wider socio-cultural norms including perceptions surrounding masculinity deeply affect how individuals with paraplegia reclaim their sexuality in South Africa. Strengthening of health systems within South Africa is required to provide more timely, integrated and personalised support and education to people with spinal cord injury across the care continuum from acute to community settings.
Data availability
Data generated and analysed for this study is available from authors on request. However, some limitations may apply in order to protect the identity of participants in this small study.
References
World Health Organisation. Defining sexual health: report of a technical consultation on sexual health 28–31 January 2002. Geneva: World Health Organisation; 2006.
Bowling J, Blekfeld-Sztraky D, Simmons M, Dodge B, Sundarraman V, Lakshmi B, et al. Definitions of sex and intimacy among gender and sexual minoritised groups in urban India. Cult, Health Sexuality. 2019;22:520–34.
American Occupational Therapy Association. Occupational therapy practice framework: domain and process (2nd ed.). Am J Occup Ther. 2008;62:625–83.
World Health Organisation. Promoting sexual and reproductive health for persons with disabilities: WHO/UNFPA guidance note. Geneva: World Health Organisation; 2009.
Goddard RL. Sexuality and spinal cord injury. J Neurosci Nurs. 1988;20:240–4.
Aikman K, Oliffe JL, Kelly MT, McCraig F. Sexual health in men with traumatic spinal cord injuries: a review and recommendations for primary health-care providers. Am J Men’s Health. 2018;12:2044–54.
Thrussell H, Coggrave M, Graham A, Gall A, Donald M, Kulshrestha R, et al. Women’s experiences of sexuality after spinal cord injury: a UK perspective. Spinal Cord. 2018;56:1084–94.
Fisher TL, Laud PW, Byfield MG, Brown TT, Hayat MJ, Fiedler IG. Sexual health after spinal cord injury: a longitudinal study. Arch Phys Med Rehabil. 2002;83:1043–51.
Sharma CS, Singh SR, Dogra SR, Gupta SS. Assessment of sexual functions after spinal cord injury in Indian patients. Int J Rehabil Res. 2006;29:17–25.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-Dewan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6:e1196–252.
Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371.
Verschuren JEA, Enzlin P, Dijkstra PU, Geertzen JHB, Dekker R. Chronic disease and sexuality: a generic conceptual framework. J Sex Res. 2010;47:153–70.
Joseph C, Delcarme A, Vlok I, Wahman K, Phillips J, Wikmar LN. Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: a prospective, population-based study. Spinal Cord. 2015;53:692–6.
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6.
Naidoo S. The South African national health insurance: a revolution in health-care delivery! J Public Health. 2012;34:149–50.
Babikir A, Satty A, Mwambi H. Determinants of out-of-pocket health expenditure and their welfare implications in a South African context. J Econ Financ Sci. 2018;11:e1–7.
Sandelowski M. Focus on research methods: whatever happened to qualitative description? Res Nurs Health. 2000;23:334–40.
Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American Spinal Injury Association (ASIA) impairment scale. Clin Orthop Relat Res. 2017;475:1499–504.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26:1753–60.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, California: Sage Publications; 1985.
Green J, Thorogood N. Qualitative methods for health research. 3rd ed. Los Angeles: Los Angeles; SAGE; 2014.
Gomes CM, Miranda EP, de Bessa J, Bellucci CHS, Battistella LR, Abdo CHN, et al. Erectile function predicts sexual satisfaction in men with spinal cord injury. Sex Med. 2017;5:e148–55.
Robinson J, Forrest A, Pope-Ellis C, Hargreaves A. A pilot study on sexuality in rehabilitation of the spinal cord injured: exploring the woman’s perspective. South Afr J Occup Ther. 2011;41:13–7.
Marimwe C, Dowse R. Development of an item bank of health literacy questions appropriate for limited literacy public sector patients in South Africa. J Commun Healthc. 2017;10:273–84.
Das S, Soni BM, Sharma SD, Gazvani R, Lewis-Jones DI. A case of rapid deterioration in sperm quality following spinal cord injury. Spinal Cord. 2006;44:56–8.
Karsenty G, Bernuz B, Metzler-Guillemain C, Grillo J-M, Saias-Magnan J, Rigot J-M, et al. Should sperm be cryopreserved after spinal cord injury? Basic Clin Androl. 2013;23:6.
Bradshaw DSK. Poverty and chronic diseases in South Africa. Technical report 2001. 2001. http://www.samrc.ac.za/sites/default/files/files/2017-07-03/povertyfinal.pdf.
Saxton M. Reclaiming sexual self-esteem-peer counseling for disabled women. West J Med. 1991;154:630.
Braaf S, Lennox A, Nunn A, Gabbe B. Social activity and relationship changes experienced by people with bowel and bladder dysfunction following spinal cord injury. Spinal Cord. 2017;55:679–86.
Ostrander N. Sexual pursuits of pleasure among men and women with spinal cord injuries. Sex Disabil. 2009;27:11–9.
Ragnarsson A, Townsend L, Ekström AM, Chopra M, Thorson A. The contrsuction of an idealised urban masculinity among men with concurrent sexual partners in a South African township. Glob Health Action. 2010;3:5092.
Sakellariou D. If not the disability, then what? Barriers to reclaiming sexuality following spinal cord injury. Sex Disabil. 2006;24:101–11.
New PW, Seddon M, Redpath C, Currie KE, Warren N. Recommendations for spinal rehabilitation professionals regarding sexual education needs and preferences of people with spinal cord dysfunction: a mixed-methods study. Spinal Cord. 2016;54:1203–9.
Joseph C, Wahman K, Phillips J, Nilsson, Wikmar L. Client perspectives on reclaiming participation after a traumatic spinal cord injury in South Africa. Phys Ther. 2016;96:1372–80.
Chaffey L, Bigby C. ‘I feel free’: the experience of a peer education program with fijians with spinal cord injury. J Dev Phys Disabil. 2018;30:175–88.
Acknowledgements
We would like to thank all participants who took part in this study, as well as research assistants (Tarryn Jeftha and Sherwin Gerwell) who assisted with logistical arrangements, translation and contextual understanding.
Author information
Authors and Affiliations
Contributions
CT was responsible for the study design, conducting interviews, interpreting results and drafting the manuscript. LB was responsible for the study design, interpreting results, revising the manuscript and approved the final version. DMC conceived the work that led to submission, was responsible for revising the manuscript and approved the final version. CJ contributed to the study design, interpreting results, revised manuscript and approved the final version. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of patient identifiable data were followed during the course of this research. Ethical approval was granted by the Western Cape Senate Research Ethics Committee (BM19/1/16). Written (nine) or verbal (one, telephone interview) informed consent was obtained prior to each interview.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Thurston, C., Blom, L., Conradsson, D.M. et al. Sex, support and society: a journey to reclaiming sexuality for individuals living with paraplegia in Cape Town, South Africa. Spinal Cord 59, 225–233 (2021). https://doi.org/10.1038/s41393-020-00558-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00558-5
This article is cited by
-
Sexual Health Among Individuals with Spinal Cord Injury: A Meta-Synthesis of Qualitative Evidence
Sexuality and Disability (2023)