Abstract
Study design
A qualitative study with an emergent design using semi-structured interviews in focus groups.
Objectives
To explore the expectations, experiences and desires among individuals who are prescribed drugs for spinal cord injury (SCI) neuropathic pain (NP).
Setting
SCI rehabilitation centre.
Methods
Eighteen informants with SCI and NP were enrolled. The informants originated from large and small cities in southern Sweden. Data were collected in focus groups consisting of 4–5 individuals in four separate sessions. An emergent design was employed using an interview guide containing open questions. The interviews were transcribed verbatim and data were analyzed according to qualitative content analysis.
Results
A model of three themes emerged: “Balancing between pain and side-effects” described the difficult choices the informants had to make between drugs and their unwanted side-effects and pain, “Desiring competence and structure in pain management” described the informants wishes regarding pain management and “From hope to personal solutions” described the process from hope of total pain relief from drugs to the development of personal strategies.
Conclusions
There is a great need for improvement of SCI-related neuropathic pain management since recommended drugs are insufficiently effective and accompanied by severe side-effects that impact quality of life but also due to structural limitations and physicians’ lack of competence in pain management.
Similar content being viewed by others
Introduction
Neuropathic pain (NP) is often described as the most troublesome secondary medical consequence of spinal cord injury (SCI), with prevalence rates estimated to be 40–60% [1,2,3]. Pain severity typically remains relatively high, consistent, or even increasing over time for individuals with SCI [4]. It is well-documented that chronic pain is detrimental to quality of life, and consequently that individuals with SCI who suffer from treatment-refractory pain are at elevated risk of severe psychological distress. Individuals with SCI have a fivefold increase in risk of suicide, and pain may be a contributing factor [5].
Clinically, SCI-related pain is often described as “mixed”, meaning that it has both nociceptive and neuropathic components in various degrees of severity and ratios that may be challenging to pinpoint and differentiate between [6]. While nociceptive pain is to some extent considered manageable, NP is notoriously more difficult to diagnose and treat adequately. The severity, complexity, and relatively high prevalence of SCI-related pain has led to longstanding efforts towards the development of more eloquent and reliable pain taxonomies to assist clinical work and mechanistic understanding in which a common taxonomy, the International Spinal Cord Injury Pain Classification, has been widely accepted [7]. Our work, however, is limited to investigating SCI-related NP.
Primarily, SCI-related NP is managed pharmacologically, including the use of both traditional analgesics, adjuvants, and several other types of drugs which are prescribed off label. It is no understatement to say that there exist unmet medical needs in the management of SCI-related NP. The vast majority of individuals with severe SCI-related NP are not expected to achieve complete or even acceptable pain relief, given current clinical best practices [8]. Hence, many individuals who suffer from SCI-related NP are dissatisfied with the pain management therapies that they receive [9, 10].
This work focuses entirely on the individual’s perspective of drugs that have been prescribed against SCI-related NP and is aimed to explore the informants’ expectations, experiences, and desires with these drugs.
Materials and methods
Theoretical perspective
When exploring individual experiences of a certain and unexplored area, a qualitative approach is considered a suitable method [11]. In order for the informants to be able to relate and respond to input from other informants, using group interaction for exploring experiences, focus group (FG) interviews was considered the most suitable method. We chose an emergent design with a purposive sampling technique for a focused research process [12] and used semi-structured interviews with open questions provided by an interview guide. However, due to the limited number of individuals that fulfilled the inclusion criteria, a convenience sample had to be used (Fig. 1). An interview guide was developed in a group of four professionals with various expertise in the field of SCI rehabilitation and pain management and with support from earlier qualitative study protocols. Collected data (recorded and transcribed verbatim) were analyzed using content analysis with constant comparison [12].
Informants
Inclusion criteria were having an SCI (>2 years), pain classified as neuropathic (>1 year) at and/or below the level of injury, between 20 and 70 years of age, 4 points or more on Douleur Neuropatique en 4 questions (DN4), an estimated average pain intensity during the last week of 4 or more on a 0–10 numerical rating scale (NRS), and experience of using at least one drug against NP. The informants had to be able to freely express themselves in Swedish. The recruitment aimed at including informants representing a wide variation with respect to the extent and level of injury, age, time since injury, experiences of using drugs for SCI NP and a male/female ratio representative of this patient group.
Exclusion criteria were having a concomitant brain injury or a disease that can cause NP in addition to the SCI.
The informants were recruited using five Swedish Facebook groups for individuals with SCI having 304/915/1340/1520/2600 followers respectively at the time of advertising. Furthermore, announcements were posted on the homepage of an SCI foundation and the SCI rehabilitation centre where the interviews were conducted. The goal was to have five informants each in four interviews. In total, 58 individuals communicated their interest to participate in this study, and all were contacted to fill out a form in order to match them towards the inclusion and exclusion criteria. Thirty individuals returned complete forms out of whom 24 fulfilled the study criteria. Three declined due to lengthy travel distance, thus 21 were contacted to schedule an interview and accepted to participate. Three individuals cancelled at the last minute due to sickness. In total, 18 informants participated in the interviews (Fig. 1).
All 18 informants consented to participation in writing. Of these, 13 were men and 5 were women with a median age of 57 years (range 26–68 years), with a median time since injury of 8 years (range 2–37 years). The informants lived both in large cities and smaller towns and had experience with a total of 6 different rehabilitation settings (regional and county hospitals). Sixteen had a traumatic injury. The informants reported having pain (classified as neuropathic) since a median of 5 years (range 2–37 years) and the median intensity of their pain on average during the last week was 7 on a 0–10 NRS. Median score on the DN4 was 7 (range 5–9). All had experience from using drugs for their SCI NP but at the time of the interview 15 used prescribed drugs for SCI NP on a regular basis; 10 individuals used antiepileptic drugs, 8 antidepressants, 5 opioids, 1 a cannabinoid (nabiximols) and 1 a local anaestethic. Mean value for number of current drugs used for SCI NP was 1.4 (range 0–4). Six informants used two or more drugs for their SCI NP. For demographic data, see Table 1.
Data collection and analysis
All the informants were screened in a telephone interview regarding inclusion and exclusion criteria. At this occasion, the informants reported that their pain had been classified as neuropathic by a physician at a spinal or a rehabilitation unit. In order to confirm this classification, a score of 4 or more (cut-off value for NP) on the DN4 was an inclusion criteria. DN4 is a screening instrument for NP and has been proven reliable in a cohort of individuals with SCI NP [13]. The first two questions of the DN4 were asked over the phone and at the occasion of the interview all informants went through a minor sensory assessment (DN4 questions 3 and 4) conducted by CN. The interview team consisted of one moderator (KW, physiotherapist experienced in SCI research and qualitative methodology), one supporting moderator (CN, physiotherapist with long experience from SCI pain management and experienced in SCI NP research as well as in qualitative research and focus group interviews), and one observer (KS, medical student). The interviews were conducted at an SCI rehabilitation centre, lasting for a mean of 80 minutes (range 74–85 min), and were all recorded and transcribed verbatim (KS). The interview guide consisted of open questions addressing the informants’ expectations and fears, positive and negative experiences of using drugs, as well as compliance and desires concerning pain management. Using an emergent design, the interview guide went through minor revisions after the second and third interview according to the emerged data and the aim of the study. This resulted in “desires” being explored in more detail during interview 3 and 4 while “compliance” was considered saturated after interview 3.
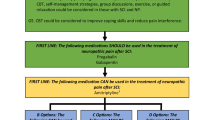
Data analysis ran parallel to the data collection and coding, using the Open Code computer programme, version 4.03 [14], and started after the first two interviews with coding of phrases and sentences by CN, KS, KW and FvK separately. Comparing and discussing codes until agreement was done after the first two interviews. The coding was manifest [12] aiming at capturing the content of the data. Interviews three and four were both coded by KW and CN separately. After the first two interviews categorization of the codes was initiated. After coding all four interviews, categorization of interview 3 and 4 was continued by CN, KW and FvK. Constant comparison was utilized during the whole process. Comparing codes, categories and themes back and forth was carried out to ensure that the categories were based on the collected data. The categories were entitled conferring to content. The categories were then analyzed to identify overlapping and similarities. The unified categories were then relabelled when needed. At this point 17 categories emerged; the treatment process, little or good effect of drugs, none or insufficient effect of drugs, cognitive side-effects, unacceptable additional side-effects, scepticism towards drugs, secondary gain, alternatives to medication, personal strategies, the structure of pain management, meeting with the physician, knowledge, family support, peer support, hope and expectations, disappointment and hopelessness, and the choice between pain and side-effects. The 12 final categories were discussed and clustered into three main themes. The three themes were labelled to reflect content. Finally, representative quotes were chosen to exemplify the themes. The emerging categories were thereafter discussed until all investigators agreed (Fig. 2).
To ensure trustworthiness, triangulation was used throughout the research process using the following strategies [15]: (1) we used a convenience sampling including informants living in both large cities and small towns having varied experiences from specialized SCI units, general rehabilitation units/county hospitals and primary care mirroring the actual situation for the SCI population in Sweden. The informants represented different age groups, level of injury, time since injury and years living with SCI and NP (i.e., transferability and credibility). (2) The researchers involved had complementary professions and fields of expertise; KW and CN as described previously, FvK a medicinal chemist, CH a physician specialized in SCI rehabilitation and KS a medical student. During the analysis the authors’ different pre-understanding was highlighted and discussed throughout the course of the analysis to ensure confirmability and credibility. The fact that the interviewers were the same and that the interviews were conducted during a short period (7 weeks) supports dependability. Neither KW nor CN were or had been involved in the informants’ rehabilitation, except for one informant who was a patient in a pain clinic (about 13 years ago) where CN worked.
Ethical approval was given by The Regional Ethical Review Board in Stockholm with ref. no. 2018/1669-31. The informants did not receive compensation for participating in the interviews.
Results
The first 17 categories were in the process merged into 12 and finally into 3 themes (Fig. 2); “Balancing between pain and side-effects”, “Desiring competence and structure in pain management” and “From hope to personal solutions”. Thereafter the model “Challenges and facilitators—navigating in the landscape of SCI neuropathic pain” (Fig. 3) was constructed to illustrate the process the informants had gone through, their experiences, desires and strategies. The three main themes are described below, illustrated by quotations from the informants.
Balancing between pain and side-effects
The theme “Balancing between pain and side-effects” contain five categories (see Fig. 2), and is derived from the positive and negative experiences the informants had from the use of prescribed drugs for their NP.
All informants had tried numerous analgesics and adjuvants commonly recommended in treatment recommendations and most of the informants were still on one or more drugs (see Table 1). Positive and negative effects of drugs mirror that many of the informants had tried drugs that were described as having no or very limited effect on their NP. However, even a slight improvement in pain was highlighted as very important, affecting quality of life positively. Taking the edge off the pain could be sufficient for continuing medication, if the side-effects were tolerable. But a low effect could also be the reason for ceasing medication.
“Somehow you are hoping, could it reduce the peaks a bit? I’m thinking that when your quality of life is as bad as many of us feel that it is, then that improvement, percentage-wise, is really important. What for other people would have been a very small improvement in percentage becomes for us a very big improvement”.
Interview 1—Informant no 1
“Unacceptable additional side-effects” contained statements where many drugs were tried but reasons for ceasing medication could be due to insufficient effect or unwanted side-effects, even though there were those that described having a moderate effect without any major side-effects. The reported effects of a specific drug and its side-effects varied greatly amongst the informants. The most bothersome side-effects the informants reported were cognitive ones such as “alterations in my personality”, “feelings of being drugged”, “being in my own bubble”, “being slow/stupid, aggressive” or feeling like a “zombie”. Gastro-intestinal side-effects, nausea and weight-gain were also described as major limitations to compliance.
“Then, you get used to it fairly quickly too, so in the end I didn’t feel groggy; it was my husband who said I was groggy”.
Interview 3—Informant no 1
“But that is exactly the problem, isn’t it, that you get such goddamn strong drugs, perhaps necessarily so, and turn into a zombie, all day. I mean you exist, but in some way you’re not really alive. But the pain goes away”.
Interview 4—Informant no 5
Scepticism towards drugs came in many variations. Existing scepticism towards drugs dating from before the injury was described, but scepticism also developed as a result of the experience of trying different drugs and from reading about common side-effects on the drug’s leaflet. Desires for more “natural” drugs were expressed.
“I think that it to me is much about my attitude toward chemical substances, simply. I don’t want to take too much of those because I want to be as clean as possible in both brain and body, sort of. For me personally, Sativex is the only one I know that works. And, with the addition that it is so natural. At least it’s a plant. Not only chemical additives, and it works. It feels like there are fewer physiological side-effects from cannabis than from neurontin and lyrica, so that’s why I continued with that one. And I know the others don’t work”.
Interview 2—Informant no 3
Secondary gain reflects the participant dilemma when it comes to continue or not with the treatment. For instance, a gain that was described as contributing to continued use was improvement on sleep and sometimes spasticity due to the drugs prescribed for NP. This could actually be the solitary effect of the drug but was described as important.
“I do sleep a little better on the [pain] medication because it makes me so tired. Without any drugs, I sleep maybe two hours in total each night”.
Interview 4—Informant no 4
Choosing between pain and side-effects cover the informants’ descriptions concerning that the effect of the drug and its side-effects could lead to difficult choices. The cognitive side-effects were described as major limitations regarding participation in both occupational and social activities as well as in family life. Not only drugs, but also pain was reported to have major “side-effects”, i.e., negative impact on life and therefore many described having to make a difficult choice between pain relief accompanied by side-effects from drugs or being an active participator in life. Sometimes it was considered more important to be able to take an active part in life than having pain relief accompanied by unwanted side-effects and therefore the use of drugs/dose could change depending on the situation.
“Am I supposed to feel this drugged, yet still somehow get by and manage to have my children grow up to become good people? My children were young when I injured myself so there were no viable alternatives. The only option was to stop taking the medicine and be mentally alert instead”.
Interview 2—Informant no 3
Desiring competence and structure in pain management
The theme “Desiring competence and structure in pain management“ are based on three categories. It was not only the effect and/or the unwanted side-effects that were described as influencing drug compliance but also the treatment process together with the personal meeting with the physician. “The treatment process” included the informants’ description of a lack of continuity that would normally be found in a structured treatment plan that included evaluation of prescribed medication and follow-up. Due to this lack of follow-up, some did not know if their current medication still had a pain-relieving effect but continued anyway. Many times, the informants felt left on their own, and with no one to contact easily when needed, they experimented with doses by themselves whereas they would have liked to have someone to discuss with.
“Will it [pain] be evaluated, questioned some day? I don’t know, and I haven't heard anything about that. But you would like to simply do an evaluation some time. Should I try and take away something or should we try something else? It’s just a complete blank. There is no sounding board at all”.
Interview 3—Informant no 2
“Meeting with the physician” underline that those who had the opportunity to discuss dosing with their treating physician, and/or could contact a nurse for discussion, highlighted this as important. At the same time they wanted to be trusted by their physician for self-regulation of smaller changes in dosage. Since trying a new drug takes time and often is accompanied by side-effects that are worst in the initial phase, the informants described that the testing periods need to be well planned in order to increase compliance. They also reported that they were more comfortable with decreasing rather than increasing the dose on their own.
“Because that’s the way it is for us, we have a nurse to call. It’s not always that you get through that same day but if you leave a message they’ll call you back the next day, and that makes a big difference, because then you won’t feel so vulnerable either if there is an issue with something”.
Interview 1—Informant no 3
Having a good dialogue and well-functioning communication with the treating physician was described as essential and having this was often associated with a stable and long-term contact. But the opposite was also frequently reported whereby they experienced a lack of interest in their pain by their physician. Also, the informants reported lack of competence in their physicians regarding issues such as what drug to prescribe and if the prescribed drugs interacted.
“I feel I haven’t gotten, like when you see the doctor, they have thought things to be super-complicated, really heavy and [they have] not even wanted to have a dialogue. I would rather just come in, and that someone had had at least a little knowledge about this, asked the right questions and sort of guided me. And that part has been completely absent, I think. So, in these situations I have felt pretty much alone”.
Interview 3—Informant no 2
“Back then I would have wished that someone had done, that there had been someone… I mean, reasonable investigations after a while. Now we will examine you, now you have taken this for two years. And that you kind of have, someone who has the know-how”.
Interview 3—Informant no 1
They wondered if physicians at other spinal/rehab centres were more capable. Physicians in primary care just prescribed the drugs that once had been initiated without evaluation or discussion. Being educated about pain and pain management by the physician was also stressed as important but rare. Informants reported that the contacts with their physicians could be a struggle and that they were leaving out pain as a problem in their meetings based on former experiences where this had not led to action. Trust in a physician and trust back affected the relationship. The informants also believed that the relationship could affect compliance and the effect of drugs.
“Then it’s almost like you avoid taking up the conversation, just because you don’t want to waste the energy of the doctor on it so that there is some left for the ordinary diseases you have, like urinary tract infections, intestines and other problems”.
Interview 3—Informant no 3
The informants reported that it was easier to get help with the addition of a new drug rather than the opposite. In Alternatives to medication they alsostated that they wanted a more holistic approach from the physicians in which not only drugs were offered for their NP, but non-pharmacological alternatives also. The informants described positive effects from primarily physical activity and exercising but also from interventions such as transcutaneous electrical nerve stimulation, massage and psychological strategies. They had, on their own, learnt to accept and live with their pain but wanted the health care system to incorporate not only drugs but also other alternatives for the management of their NP.
“Dare to try alternative drugs and treatments. So it doesn’t become a shelved question, but it’s there on the table; here you are, here is our smorgasbord and there are all these kinds of pills, of course, but also other things!”
Interview 4—Informant no 5
In summary, the informants desired improved availability, continuity in contacts, a structured treatment plan including alternatives to drugs, evaluation of prescribed medications, and a good dialogue with a treating physician that has both an interest in and high degree of competence with pain treatment. When needed, the informants wanted referral to a pain specialist. This was not a common occurrence in this group, and those who were referred reported that it was a very lengthy process.
“He did something I appreciated, because when I had gone through a lot of medications he put it like this: ‘This is the map that lies ahead, that is, these are the possible things to test apart from what we have already tried. There are not many possible options left.’ We started talking about transcranial magnet stimulation and so on, so he said there are a few of these things that I don’t think you should do, but I think you should know which possibilities remain. And I think that it was fantastic, to meet such a doctor”.
Interview 1—Informant no 1
From hope to personal solutions
In the beginning, when their pain started, hope for pain relief was described as great, based on former experiences where a pill most often relieved pain completely. “Hope and expectation” illustrate for instance that over time hope decreased rather significantly or became more realistic due to knowledge acquired about common effects from drugs usually prescribed for NP. Further it reflects that expectations if trying a new drug were rather low, but still a hope for a new, better and useful drug was vivid. A drug with greater pain relief than in those tried, without unwanted side-effects, and a drug that could be taken when needed instead of daily. It was described as important not to lose hope and that hope increased when a new drug was on the market.
“When I sit there at the doctor’s, the expectations are still high, that there will be a miracle medication, but still, in my brain I know that this isn’t something I expect. But still I do kind of expect it, kind of a hope, I mean hope is what can’t abandon you because then, then you kind of end up with suicidal thoughts. But then you still get as disappointed every time it doesn’t work”.
Interview 1—Informant no 3
But alongside hope and expectation was “Disappointment and hopelessness” since after trying a new drug with less effect than desired and/or intolerable side-effects, despair and exhaustion were described. The trial periods were often long (and many) and when the new drug didn´t lead to improvement disappointment, grief and hopelessness was described, even suicidal thoughts.
“Personal strategies” describe that the informants over time developed personal strategies to cope with their situation; both with pain, medication, and side-effects. Distraction was an often-used tool; social and leisure activities were especially highlighted, but also work could be a distraction.
“The bottom line is perhaps that distraction is the only thing that helps, and that is the reason I exercise so much, so I don’t think about it [the pain]”.
Interview 1—Informant no 4
“So when something’s not quite as it should be when I go to bed at night, that it is these really awful [pain episodes] that come. And I don’t think I’ve ever fallen asleep without listening to a podcast in like three years. That too is a distraction”.
Interview 4—Informant no 1
Being still at home aggravated pain. Some informants had learnt to live with their pain or at least accepted that for now it is not going to get better, but some just endured their pain. Giving up the struggle for better pain relief was a relief in itself.
“I accept the pain more. I have learnt to deal with it in another way. And I think that that is the most important part. You have to try, even if you only want to go and bury yourself, you have to try to deal with it somehow”.
Interview 1—Informant no 5
“Alcohol is bloody good, it helps. There is no getting out of that. It takes down the pain a fair bit. In this aspect, alcohol works as a medication, sort of. But that is unsustainable of course”.
Interview 2—Informant no 1
Having “drugs in the drawer” is another side of “Personal strategies” and was reported to be important and a source of security when and/or if needed. Taking an extra pill in order to be able to do something out of the ordinary like going out with friends, or on a long flight was expressed as a feeling of being safe and secure.
“I have a prescription for oxycodone in case things turn out really bad. So I can take it, but it’s just sitting in my drawer, and you have to throw away boxes when they expire. Nevertheless though, it’s damn nice to have it [available]. I can accept a higher pain intensity when I know I have it [access to the drug], compared to when I don’t”.
Interview 4—Informant no 2
Support includes descriptions of taking support from peers as well as assistance from family. Peer support was especially important at times when pain increased and health care was unavailable. Peer support could even be initiated before contacting their physician. Exchange of experiences, obtainment of advice and solicitation of others in the same situation was performed using social media. Facebook groups gave support and knowing that you are not alone in this situation helped out.
“When you are in the worst possible pain, there’s no way in hell I call the doctor right then. I call my buddy, who is in the same situation as me. But what the heck had you done right now?”
Interview 1—Informant no 3
Families were victims but also important support and were reported to take active part in decisions regarding, e.g., continuing or ceasing medication since both pain and side-effects affected the family. The close relatives could be the ones discovering cognitive side-effects that the informant had become accustomed to.
"Well, it was my wife who pointed out [that things were perhaps not alright] when I lay in bed at night and read children’s books out loud. And spluttered. At first, I didn’t notice it myself. But later when she called my attention to it... I started thinking".
Interview 2—Informant no 4
Discussion
The overall findings in this study are captured in the three main themes; “Balancing between pain and side-effects”, “Desiring competence and structure in pain management” and “From hope to personal solutions”, together creating the model Challenges and facilitators—navigating in the landscape of SCI NP. Both categories and themes could be parallel experiences and processes could be shorter or longer in time or ongoing. The informants experienced both the challenges and facilitators that the categories constituted of and they described having to navigate between them.
The informants commonly described their journey from being hopeful regarding pain relief to a stage where they had developed personal strategies to cope with pain. This often included the use of drugs providing little or moderate pain relief, taking the edge of their pain and helping them function in daily life. Many of the drugs used were accompanied by unwanted side-effects, with the cognitive side-effects especially limiting the possibility to take an active part in social and occupational life. Therefore, it was described as making a choice between pain relief and side-effects. Non-pharmacological treatments for pain were warranted as part of the pain management package. Improved structure of pain management such as follow-up and evaluation of prescribed drugs, and increased interest in and knowledge about SCI NP was desired.
The limited effects of the prescribed drugs as well as the unwanted debilitating side-effects reported by the informants confirm the difficult situation faced by both individuals with SCI and NP and health care professionals since the drugs used are those recommended for this particular type of pain. These findings are not new, nor unique for this particular cohort and have also been reported from Italy [16], UK [17] and Canada [18, 19] as well as from another cohort in Sweden [10] indicating that we, as health care professionals, need to address this topic world-wide. NP in general is challenging to relieve pharmacologically, and SCI NP even more. NNT-values (number needed to treat) for the drugs recommended for NP are high and varies between 3.6 and 7.7 [8] supporting the difficulty faced in relieving this type of pain. Few, and mainly small, pharmacological studies have shown efficacy when treating SCI NP and most of these studies have also reported substantial side-effects affecting compliance.
In our study the cognitive side-effects were described as the most bothersome ones; findings supported by previous studies [9, 17, 18]. As in the study by Hearn et al. [17] many informants therefore refrained from using (these) drugs “choosing” to live with pain and the unwanted side-effects from pain itself instead. A most difficult choice to make, especially since the informants highlighted that pain itself is accompanied by several “side-effects” such as insomnia, stress, and social isolation.
But in parallel, the informants in our study highlighted that even a small reduction in pain intensity—taking the edge off the pain—can be of major importance and the drugs prescribed for NP could also exert a major effect on other parameters such as sleep and spasticity even when no effect on pain was experienced, stressing why these drugs still have a role to play.
There were informants that did not know if their current medication even demonstrated any effect, since evaluation and follow-up were something that the informants lacked, but desired. The informants described a wish for the physicians to take a greater interest in and demonstrate more knowledge about SCI NP, results supported by informants in one of our previous studies [10] as well as in the study by Buscemi et al. [16]. In the current study the informants also described wanting a dialogue with the treating physician regarding when to start a testing period, how to experiment with the suggested dose together with regular follow-ups and evaluations. Testing periods were tiresome and therefore needed structure and planning for best result. In this process, the informants often felt being on their own with availability to a nurse-on-call was highlighted as valuable.
The results raise an interesting question regarding whether compliance to drugs, and thereby a better outcome, could be facilitated through an improved pain management structure that includes improved knowledge of and competence in pain assessment and treatment. The desire to be offered non-pharmacological treatments as a part of the pain management package has also been described by others [9, 16, 18] and in previous published studies [20, 21], patients have stated that interventions such as massage, warmth, TENS, physical exercise and acupuncture are (the most) effective treatments for their NP. These types of treatments are, however, rarely suggested in guidelines due to the limited evidence from scientific studies. Only tDCS [22] is in a review on non-pharmacological options for SCI NP considered to be effective. tDCS is in the CanPain SCI clinical practice guidelines [23] mentioned as third-line therapy where visual illusion (third line) and TENS (fourth line) are also listed as useful alternatives to drugs. Unfortunately, at least in Sweden, tDCS is not an available option.
The findings in theme “From hope to personal solutions” underline that even though disappointment with the effect of drugs was initially great, experience from trial periods and increased knowledge about NP over time served to decrease initial expectations. Nevertheless, hope never seemed to abandon them. Hope for a cure—a single pill that could dramatically relieve pain without side-effects was still there. Additionally, the informants described that support and guidance was solicited via the internet, where other persons with SCI networking in specific SCI communities on Facebook could play an important role as peers with the addition of support, knowledge, and suggestions. This factor has also been described in the cohort from the UK [17].
Limitations
The study findings should be taken in consideration of the following limitations. One of our study´s limitations was the low number of individuals fulfilling the study criteria (n = 24) and thus invited to participate in our study. We aimed for a purposive sampling but ended up with a convenience sample due to this. Even so the distribution in gender and type of injury was representative of the SCI population but having a lower mean age would have been preferable since experiences would be broader in time. Recall bias can be a problem when asking informants to share their experiences and several of the informants recalled memories that in some cases lay many years back. However, the results contained critical aspects of living with pain and dealing with pharmacological treatment that according to the informants were significant for them.
Public health care in Sweden differs from other parts of the world, why transferability may not be appropriate to all other contexts. But even so, our results were supported by findings from studies conducted in other countries.
It is true that studies supporting an effect from interventions such as physical exercise, cognitive behavioural therapy, pain programmes, massage and acupuncture are scarce but side-effects are rare and the mentioned treatments safe. Considering the small effects of recommended drugs, the extent of side-effects, the multiple studies where patients request options other than drugs, and the fact that NP has such a major impact on the informants’ daily life and on sleep quality, we want to strongly encourage the inclusion of non-pharmacological options when treating SCI NP.
Finally, SCI units could also facilitate the development of coping strategies for persons with SCI living with NP through creation of favourable clinical settings. This could include “Support“ from peers and family, presentation of a palette of commonly used “Personal strategies” as well as being sounding board for the informants when navigating through the challenges described in this study.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Werhagen L, Norrbrink Budh C, Hultling C, Molander C. Neuropathic pain after traumatic spinal cord injury—relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord. 2004;42:665–73.
Dijkers M, Bryce T, Zanca J. Prevalence of chronic pain after traumatic spinal cord injury: a systematic review. J Rehabil Res Dev. 2009;46:13–29.
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015;19:5–14.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47:108–14.
Hagen EM, Rekand T. Management of neuropathic pain associated with spinal cord injury. Pain Ther. 2015;4:51–65.
Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord. 2012;50:413–7.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;4:162–73.
Löfgren M, Norrbrink C. “But I know what works”-patients’ experience of spinal cord injury neuropathic pain management. Disabil Rehabil. 2012;34:2139–47.
Norrbrink C, Löfgren M. Needs and requests-patients and physicians voices about improving the management of spinal cord injury neuropathic pain. Disabil Rehabil. 2016;38:151–8.
Barbour R, Kitzinger JE. Developing focus group research. London: SAGE Publications; 1999.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12.
Hallström H, Norrbrink C. Screening tools for neuropathic pain: can they be of.use in individuals with spinal cord injury? Pain. 2011;152:772–9.
ICT Services and System Development and Division of Epidemiology and Global Health. OpenCode 4.0. Umeå: and Department of Public Health and Clinical Medicine, Umeå University, Sweden; 2011. http://www.phmed.umu.se/enheter/epidemiologi/forskning/open-code/.
Lincoln Y, Guba E. Naturalistic inquiry. London: SAGE Publications; 1985.
Buscemi V, Cassidy E, Kilbride C, Reynolds FA. A qualitative exploration of living with chronic neuropathic pain after spinal cord injury: an Italian perspective. Disabil Rehabil. 2018;40:577–86.
Hearn JH, Cotter I, Fine P, Finlay AK. Living with chronic neuropathic pain after spinal cord injury: an interpretative phenomenological analysis of community experience. Disabil Rehabil. 2015;37:2203–11.
Henwood P, Ellis JA. Chronic neuropathic pain in spinal cord injury: the patient’s perspective. Pain Res Manag. 2004;9:39–45.
Henwood P, Ellis J, Logan J, Dubouloz CJ, D’Eon J. Acceptance of chronic neuropathic pain in spinal cord injured persons: a qualitative approach. Pain Manag Nurs. 2012;13:215–22.
Norrbrink Budh C, Lundeberg T. Non-pharmacological pain-relieving therapies in individuals with spinal cord injury; a patient perspective. Complement Ther Med. 2004;12:189–97.
Heutink M, Post MW, Wollaars MM, van Asbeck FW. Chronic spinal cord injury pain: pharmacological and non-pharmacological treatments and treatment effectiveness. Disabil Rehabil. 2011;33:433–40.
Boldt I, Eriks-Hoogland I, Brinkhof MW, de Bie R, Joggi D, von Elm E. Non-pharmacological interventions for chronic pain in people with spinal cord injury. Cochrane Database Syst Rev. 2014;11:CD009177.
Mehta S, Guy SD, Bryce TN, Craven BC, Finnerup NB, Hitzig SL, et al. The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord: screening and diagnosis recommendations. Spinal Cord. 2016;54:S7–13.
Acknowledgements
We gratefully acknowledge Neuro Sweden for their contribution.
Funding
This study was partly funded by Neuro Sweden.
Author information
Authors and Affiliations
Contributions
All authors have contributed to all aspects of the stated criteria. Design: CN, KS, CH, FvK, and KW. Data collection: CN, KS, and KW. Analysis of collected data and the results interpretation of the result: CN, KS, FvK, and KW. Draft and or revision of paper: CN, KS, CH, FvK, and KW. Approved the final paper and agreed to be responsible for all aspects of the work: CN, KS, CH, FvK, and KW.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Ethical approval was given by The Regional Ethical Review Board in Stockholm with ref. no. 2018/1669-31.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Norrbrink, C., Sörling, K., Hultling, C. et al. “Challenges and facilitators—navigating in the landscape of spinal cord injury neuropathic pain”—a qualitative study on the use of prescribed drugs. Spinal Cord 59, 215–224 (2021). https://doi.org/10.1038/s41393-020-00553-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00553-w
This article is cited by
-
Central neuropathic pain
Nature Reviews Disease Primers (2023)