Abstract
Study design
Health-related quality of life (HRQOL) data from two parallel independent single-blinded controlled randomized studies of manual (Study 1) and robotic (Study 2) locomotor training were combined (ClinicalTrials.gov #NCT00854555).
Objective
To assess effects of body-weight supported locomotor training (BWSLT) programs on HRQOL in persons with long-standing motor incomplete spinal cord injury and poor walking function.
Settings
Two inpatient rehabilitation facilities and one outpatient clinic in Norway.
Methods
Data were merged into intervention (locomotor training 60 days) or control group (“usual care”). Participants completed questionnaires before randomization and 2–4 weeks after the study period, including demographic characteristics, HRQOL (36-Item Short-Form Health Status Survey, SF-36), physical activity (The International Physical Activity Questionnaire Short Form, IPAQ-SF), exercise barrier self-efficacy (EBSE), and motivation for training (Behavioral Regulation in Exercise Questionnaire, BREQ). Physical outcomes i.e., Lower extremity motor score (LEMS) was assessed. The main outcome was change in HRQOL. Secondary outcomes included changes in IPAQ-SF, EBSE, BREQ, and physical outcomes.
Results
We recruited 37 of 60 predetermined participants. They were autonomously motivated with high baseline physical activity. BWSLT with manual or robot assistance did not improve HRQOL, though LEMS increased in the BWSLT group compared with control group.
Conclusions
The study was underpowered due to recruitment problems. The training programs seem to benefit LEMS, but not other physical outcomes, and had minimal effects on HRQOL, EBSE, and motivation. Autonomous motivation and high physical activity prior to the study possibly limited the attainable outcome benefits, in addition to limitations due to poor baseline physical function.
Similar content being viewed by others
Introduction
In the last decades, body-weight supported locomotor training (BWSLT) has been promoted as a rehabilitation tool for persons with incomplete spinal cord injury (SCI) [1]. An early report [2] and more recent studies [3,4,5,6,7,8] show that BWSLT improves walking function for persons with SCI in subacute (<1 year post injury) and chronic (≥1 year post injury) phases. Also, health-related quality of life (HRQOL) [5, 6, 9] and perceived physical function seem to improve [8,9,10] in the chronic phase, but so far, HRQOL-studies following BWSLT are relatively few [5,6,7,8,9,10]. Table 1 provides an overview of BWSLT studies that have assessed HRQOL and well-being among SCI populations with postinjury time >1 year. A recent review and meta-analysis of activity-based interventions among SCI populations included three BWSLT randomized controlled trials (RCTs) that assessed HRQOL [11]. The authors conclude that such intervention had no effect on HRQOL compared with none or conventional physical therapy.
Although the main goal of BWSLT is to improve walking function, there may be secondary psychological benefits from the experience of standing and walking [9]. In addition, there are several psychosocial factors at work in an intervention, such as psychological needs satisfaction or social support from instructors. Few studies have assessed the role of psychosocial factors in relation to how they influence the outcomes and individual experiences of a BWSLT program. Knowing that psychosocial factors influence, and are influenced by a totality of experiences and behavior, the present study tests the hypothesis that compared with controls, a BWSLT intervention improves HRQOL and psychological outcomes such as exercise barrier self-efficacy (EBSE) and quality of motivation in participants with long-standing (+2 years post injury) incomplete SCI with severely reduced physical function (walking function, lower limb muscle strength or balance).
Methods
Design
We combined data from our two independent single-blinded randomized controlled RCTs [12, 13], study 1 with manually assisted BWSLT and study 2 with robot assistance. The studies follow the CONSORT 2010 guidelines, were approved by the Regional Ethics Committee in North Norway (P REK NORD 69/2008 and 2009/634–5) and registered in ClinicalTrials.gov (#NCT00854555).
Recruitment
Briefly, participants were recruited nationwide through the Norwegian SCI units and cooperation with patient organizations. For logistical reasons, participants from the entire country, except the Oslo area, were enrolled to the inpatient study in Tromsø (Study 1), whereas those living within driving distance from Oslo were enrolled as outpatients (Study 2). Written informed consent was obtained prior to inclusion.
Participants
The study included adults (18–70 years) with motor incomplete SCI classified as American Spinal Injury Association (ASIA) Impairment Scale grade C or D (AIS C-D) [14], with postinjury time +2 years and body mass index <30 kg/m2. Participants were primarily wheelchair dependent, cognitively unaffected and motivated for BWSLT (Supplementary Fig. 1) and instructed to continue their usual dose of antispasmodic medication and physical activity level throughout the study.
Setting
Pre- and post-intervention evaluations were conducted single-blinded by the same physical therapists and physicians at Sunnaas Rehabilitation Hospital, Norway.
Randomization
In both studies, participants were randomized in blocks of ten by the sealed envelope method.
Training protocol
Intervention consisted of 60 training days of BWSLT, either with manual or robotic assistance 60–90 min per day, 3–5 days per week over 6 months [12, 13]. Participants were suspended in a body-weight support system with treadmills (Vigor Equipment, Inc., Stevensville, MI, USA) (Study 1) or the Lokomat® gait training robot (HOCOMA AG, Zürich, Switzerland, version 4) (Study 2). A physical therapist supervised three to five staff members (Study 1) or controlled the robotic device (Study 2).
Control group
The C-group received usual care, typically one-on-one, by their local physical therapists 1–3 times per week (range 0–5). Telephone follow-up secured compliance [12, 13]. After the study period, control participants were offered the BWSLT.
Outcome measures
Prior to randomization, baseline evaluation occurred within 1 month before and post evaluation 2–4 weeks after the study period. Assessors were blinded to participants’ group allocation.
Physical outcome variables included lower extremity motor score (LEMS), 10-meter walk test, 6-min walk test and Berg balance scale, modified functional reach, and aerobic capacity (VO2) [12, 13] (Table 2). Self-administered questionnaires were completed at baseline and post evaluation, and included demographic characteristics, a standardized questionnaire on HRQOL [15, 16] and well-tested, validated questionnaire on physical activity [17], EBSE and motivation for the training [18, 19]. Participants’ expectations to the BWSLT and how important these were regarded, were registered. All outcome measures have previously been used in disabled persons [20,21,22,23].
The primary outcome was change in HRQOL measured by the 36-Item Short-Form Health Status Survey (SF-36, version 1.2 chronic) [15, 23]. This generic questionnaire includes eight health-related components, from limitation of physical functioning due to health problems to questions on general mental health [15, 16]. Two aggregated component scores were used: (1) Physical component score (PCS) and (2) Mental component score (MCS) with higher score indicating better perception of HRQOL on a scale of 0–100.
Secondary outcomes were changes in (1) Self-reported physical activity, (2) Self-efficacy related to confidence in ability to exercise in spite of barriers, (3) Type of motivation, and (4) Participants’ expectations of the results and their importance.
The International Physical Activity Questionnaire short form (IPAQ-SF) gathers information about physical activity from the last 7 days and has shown good or acceptable reliability and validity [17]. Time spent walking/wheeling, engagement in moderate activity, vigorous-intensity activities, time spent sitting, and total physical activity (MET-min/week) were recorded according to IPAQ guidelines (https://sites.google.com/site/theipaq/home) [24].
EBSE was assessed with 14 items rated on a 1–7 scale [18]. We used the Behavioral Regulation in Exercise Questionnaire with 14 items rated on a 1–7 scale, describing the type of motivation on a continuum from external, identified, introjected and intrinsic motivation [19]. These subscales were merged and reported as autonomously regulated (intrinsic and introjected), and controlled motivation (external and identified). According to Self-determination theory, the autonomous types of motivation are the more robust forms [19]. Outcome expectations were assessed by asking the participants to note expectations they believed to gain from the BWSLT and rate how well they thought they were able to meet the expectations, on a scale of 0–100 [19]. Physical outcome measures are described in detail elsewhere [12, 13].
Statistical analysis
Sample size estimation was based on data from our pilot study and the literature. For each study, 30 participants (15 in interventions and 15 in controls) were required to obtain statistical power of 0.80 with alpha error 0.05 for the primary outcome, walking function [12, 13]. HRQOL and the psychological outcomes were not used in sample size calculation, since the primary aims of the original studies was on changes in physical outcomes.
For the present analyses, we merged data from studies 1 and 2 after confirming that baseline characteristics and interventional changes in physical outcomes were similar. Baseline comparisons between the merged intervention (I) and C-groups were done using Chi-square test/Fisher Exact test and Independent samples t-test, as appropriate. Differences in between-group changes were compared by independent samples t-test or non-parametric Mann-Whitney test (non-normal distribution). Significance levels were all two-sided p < 0.05. IBM SPSS for Windows statistical software was used (version 25, IBM SPSS, Armonk, New York). We estimated the minimal clinical important difference (MCID) by the analytic (distribution-based) approach, and considered 0.5 standard deviation (SD) of baseline value as threshold for MCID [25].
Results
We were able to recruit only 44 of the 60 predetermined participants. Six participants dropped out from the intervention, and one was excluded (attended only 20/60 training sessions) resulting in 16 participants in the I-group and 21 in the C-group (Supplementary Fig. 1). At enrollment, participants had poor physical function but they were physically active, motivated and were confident of the positive consequences of the planned training (Table 2). Twenty-four of the 37 participants were wheelchair-dependent for ambulation.
The I-group had 58 days (SD 3) of BWSLT, and effective walking during each training session averaged 42 min (SD 10) with mean walking distance 1737 m (SD 443) and mean body-weight support 40% and 33%, respectively, for the robot-assisted and the manually assisted.
At study start, 15/16 in the intervention and 18/21 in the C-group had expectations of improvement in physical outcomes, especially walking function (Table 3), but at the final evaluation, expectations had declined in both groups, most among the controls (Table 4). The mean difference between the groups in “meeting the outcome expectation” variable exceeded the MCID value of 11.8 by 11.9 units (Table 5).
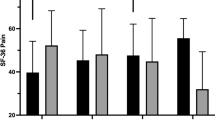
Quality of life
Baseline PCS and MCS were similar in the I- and C-group, with minor and nonsignificant changes (Table 4) and none of the mean differences between the groups exceeded the MCID values (Table 5).
EBSE and other measurements
The I-group reported higher physical activity level at baseline (5210 METs/week vs 3601 in the C-group) (Table 2), and differences were slightly greater at follow-up (Table 4), but the between group change was smaller than MCID (Table 5). EBSE was high in both groups at baseline, and declined in both, especially in the controls −1.5 compared with −0.7 in the I-group (Table 4) and the between-group difference was twice the MCID value (Table 5). The between-group difference in change in controlled form of motivation was greater than the MCID threshold (Table 5) and the change in the I-group was larger than the C-group (Table 4). However, the between-groups difference in autonomous motivation was below the MCID threshold (Table 5). Both groups had high baseline scores on expected importance of benefits from BWSLT, but changes from baseline to follow-up were small, similar and difference was below the MCID value (Table 5).
Physical outcomes
Among the physical outcomes, only LEMS showed significant improvement. A MCID >3 units has been reported as required for improving walking function [26], and we found a between-group difference of 3.6 units, favoring the I-group (Table 4). Threshold values were not exceeded for walking speed, endurance or balance [27,28,29].
Discussion
To our knowledge, this is the first RCT assessing the effect of a BWSLT intervention on HRQOL and psychological outcomes in relation to changes in physical functions among persons with long-standing incomplete SCI. Compared with usual care, intensive BWSLT did not improve physical outcomes or HRQOL. However, some of the changes in psychological outcomes including EBSE, controlled form of motivation and meeting the outcome expectations, may be of clinical importance.
For this research, we merged data from our two independent RCTs that were virtually identical in design, duration, intensity, evaluation, and outcomes, but where methods of assisted BWSLT differed. The primary purpose of the two RCTs was to assess the effect of BWSLT on walking [12, 13] and whether the interventions influenced HRQOL and psychological factors such as social and mental functioning. For these latter outcomes, we used standardized generic self-administered questionnaires [15, 18, 19, 23] suitable for the SCI population, despite shortcomings with mobility, reporting and interpretation of PCS and MCS [20, 23].
In general there is a positive association between physical activity and well-being among the SCI populations [11], but HRQOL effect studies of different training methods are scarce and inconclusive [11, 20]. This also applies to studies using BWSLT [5,6,7,8,9,10]. Mean postinjury time varied between 5 and 10 years in four RCTs [5,6,7,8], hence our study is the one with the longest time (mean time 13 years) from injury to start of intervention.
We consider the term well-being and mental HRQOL closely related, and focus on the mental dimension of the SF-36. The changes in the two HRQOL assessments (PCS and MCS) and psychological outcomes were small and the physical activity (IPAQ, autonomous motivation and importance of benefits gained) did not exceed the thresholds for the MCID. However, the difference in change between the I- and C-group exceeded the MCID for EBSE, controlled motivation and meeting the outcome expectations. Some BWSLT studies [5, 8, 9] report beneficial effects both on well-being and quality of life. Different HRQOL measures (Quality of Life index, Satisfaction with Life scale, Schedule for the Evaluation of Individual Quality of Life) [6, 8, 10], or only parts of the standardized questionnaires (SF-36) have previously been used [5, 9], making it difficult to compare the results.
EBSE and participants' expectations
We chose to study psychological components since they may influence the outcome of physical training, and vice versa. Expectations regarding outcome, perceptions of control and mastery and type of motivation for the training [18, 19] may all be important. We were, however, unable to demonstrate improvement in psychological outcomes, possibly because our participants were strongly motivated at baseline. EBSE is a persons’ confidence in own capability to keep exercising in spite of barriers [18]. Persons with high EBSE use sufficient efforts that often lead to success, whereas those with low EBSE are likely to stop their efforts early and thus fail [18]. EBSE has not been investigated in the earlier BWSLT studies [5,6,7,8,9,10]. However, a study of home-based upper-body training found a positive association between improved physical outcome and exercise self-efficacy, a more task oriented form for self-efficacy [20]. In the present study, EBSE scores fell for both groups, and more so for the controls. This may be an effect of low statistical power, as one would expect the scores to be lower among participants in the intervention group, due to the lack of substantial improvements in physical outcomes. In hindsight, we underestimated the fact that the demands of the intervention would result in a selection of individuals with an initial robust EBSE, and therefore it was not realistic to expect an increase in barrier self-efficacy post intervention. Participants' expectations of improving their walking function were high, maybe unrealistic, considering their poor baseline function and long-standing incomplete SCI. Overall, 33 of the 37 (89%) reported that their main expectation was to improve physical outcome. This is in line with reports from a previous study showing that the priority among persons with SCI recovering from an injury (irrespective of severity, age and time of injury) was to improve walking function [30]. The lowering of expectations found in our study is most likely due to the limited training results.
We anticipated improvement in physical outcomes followed by improved HRQOL, but this was not evident. Even though the participants had invested time, completed the study and experienced a positive training environment with some effects on LEMS, there was still no clear effect on HRQOL. Nor did disappointment with the results seem to lower HRQOL. Hicks et al. [9] in 12 month observational BWSLT study (n = 14), found improvements in both walking function and mental HRQOL among persons with incomplete SCI with mean postinjury time of 8 years. Satisfaction in life and in physical outcomes correlated with improvements in walking function. Alexeeva et al. [5] compared BWSLT with manual assistance when needed, BWSLT in a fixed track and conventional therapy in a RCT of 35 persons with incomplete SCI grade AIS C and D (postinjury time 7 years). Although walking speed, LEMS and Satisfaction with abilities of well-being Scale (SAWS) improved significantly in all three groups, no clear benefit was between any of the groups. A positive association was found between Mental HRQOL (SAWS) and change in balance, but not with walking speed, but again, there was no difference between the groups. On the other hand, some studies show discordant changes in physical outcomes and HRQOL. A RCT compared exercise (control) with BWSLT with functional electrostimulation, and the latter group had improvement on a mobility scale, but not in mental HRQOL [8]. Wu et al compared manual and robot-assisted BWSLT in a RCT: both groups improved walking function during training, but there was no association with HRQOL measures as assessed with SF-36 [7]. Thus, based on our findings and the literature, the association of the physical outcomes of BWSLT with HRQOL and psychological factors remains inconclusive.
Are the participants representative of the long-standing SCI population in Norway?
We think that they are, with respect to HRQOL [23]. Interestingly, their PCS and MCS scores are similar to the general Norwegian population [16], confirming data from a previous training study [20]. The participants reported being physically very active, well above the weekly 3000 MET minutes, which is the threshold value for a high physical activity level in the general population [24]. We anticipated that participation in the study would be attractive to persons with long-standing incomplete SCI, since opportunities for intensive rehabilitation are rather limited. Few individuals, however, were willing to participate in the intensive long-lasting training programs, in spite of extensive recruitment efforts through advertisements, patient organizations’ meetings, conferences etc. Their return to a regular life with established assistance, equipment, school or work, and a stabilized social life may have reduced motivation for intensive training and resulted in selection of individuals with high scores on a strong and robust form of motivation for training and exercise.
Strengths and limitations
The main strengths of our study include the randomized design, the blinded evaluation of outcomes by the same team and a homogenous patient group with respect to time since injury. Thus, we have avoided the overly optimistic results reported in previous uncontrolled studies. The main limitation is that we were unable to recruit the planned number of participants, resulting in a statistically underpowered study with less balanced intervention and control groups. However, a few more participants would hardly have changed the mainly negative outcomes.
The intense training program many years after SCI resulted in selection of well-trained participants, with very high self-reported baseline physical activity and high scores on EBSE as well as on autonomous motivation, and a strong belief that they should gain important benefits from the training. Hence, we cannot exclude the possibility that our participants already had reached the best function they could obtain within the limits given by their injury. Their strong autonomous motivation and positive attitudes could thus contribute to a “ceiling effect” both for physical and mental function. Even though the C-group was instructed to continue their usual training programs, we cannot exclude the possibility that some also increased their training during the study, thus contributing to the null findings in physical outcomes.
Some effects, such as increased lower extremity muscle strength, could potentially facilitate future alternative training (such as cardiotraining), and in the end, improve a person’s HRQOL. Others may think evaluation immediately after intervention would increase the chance of detecting improvement, which may be true. However, our intensive training program was limited in time, and participants were expected to continue their regular conventional training afterwards. If the improvement gained should decline or vanish within 2–4 weeks after return to ordinary life, the training program would not be worth the efforts and costs. Finally, the intensity of the treatment was different between the groups, mainly due to the lack of funding to develop a standardized and more intensive training for the C-group. Low intensity treatment is the common practice among individuals with long-standing SCI in Norway, and therefore we chose this approach.
At the time we designed the RCT, no psychological instruments were validated for use among SCI populations. SF-36 and IPAQ emphasize walking function, which is not relevant for wheelchair-dependents. We were able to use a modified IPAQ version that included activities performed by wheelchair users [21]. We did not formally measure participant satisfaction. However, our general impression was that they were grateful for the training, and felt it had been a good experience, even if their goal of better walking was not achieved. Appreciation of the therapists’ enthusiasm and the care provided (a Hawthorne effect) is likely, as well as other psychosocial/environmental factors present in the BWSLT setting. The role of these in eliciting changes should probably also have been better assessed.
What can be learned from this study?
Late onset training of individuals with long-standing SCI and poor baseline function resulted in only minor improvements in physical outcomes and small or no changes in HRQOL. Admittedly, the study was underpowered, but we find it unlikely that a larger number of participants would have changed the outcome significantly. Few individuals with long-standing SCI were willing to participate in an intensive long-lasting training program, and this resulted in a selection of autonomously motivated, well-trained individuals who possibly already had reached their ceiling for improvement. When training studies are compared, it may be important to consider participants’ baseline motivation and training status/exercise habits.
The clinical importance of our findings is debatable. The results argue neither for, nor against late onset intensive BWSLT in long-standing SCI, but we believe future studies should preferably be done among persons with somewhat better baseline function, and at an earlier postinjury stage. It would be interesting to see what effects a BWSLT intervention would have on walking ability, HRQOL, EBSE, type of motivation, psychosocial/environmental factors and physical outcomes among physically inactive, less autonomously motivated persons with SCI.
In conclusion, this RCT demonstrates that BWSLT among poorly functioning individuals with long-standing SCI, improves neither physical outcomes nor HRQOL. The present results cannot be extrapolated to other settings, such as training early after injury, or to those who have regained or have some remaining walking function. In this study, training started long after the SCI resulting in selection of autonomously motivated participants who already had trained intensively, and thus may have had a very small potential for further improvement.
Data Archiving
The datasets analyzed during the current study are not publicly available due to Norwegian laws and regulations.
References
Mehrholz J, Harvey LA, Thomas S, Elsner B. Is body-weight-supported treadmill training or robotic-assisted gait training superior to overground gait training and other forms of physiotherapy in people with spinal cord injury? A systematic review. Spinal Cord. 2017;55:722–9.
Wernig A, Muller S. Laufband locomotion with body weight support improved walking in persons with severe spinal cord injuries. Paraplegia. 1992;30:229–38.
Esclarín-Ruz A, Alcobendas-Maestro M, Casado-Lopez R, Perez-Mateos G, Florido-Sanchez MA, Gonzalez-Valdizan E, et al. A comparison of robotic walking therapy and conventional walking therapy in individuals with upper versus lower motor neuron lesions: a randomized controlled trial. Arch Phys Med Rehabil. 2014;95:1023–31.
Alcobendas-Maestro M, Esclarín-Ruz A, Casado-López RM, Muñoz-González A, Pérez-Mateos G, González-Valdizán E, et al. Lokomat robotic-assisted versus overground training within 3 to 6 months of incomplete spinal cord lesion: randomized controlled trial. Neurorehabil Neural Repair. 2012;26:1058–63.
Alexeeva N, Sames C, Jacobs PL, Hobday L, Distasio MM, Mitchell SA, et al. Comparison of training methods to improve walking in persons with chronic spinal cord injury: a randomized clinical trial. J Spinal Cord Med. 2011;34:362–79.
Adams MM, Hicks AL. Comparison of the effects of the body-weight-supported treadmill training and tilt-table standing on spasticity in individuals with chronic spinal cord injury. J Spinal Cord Med. 2011;34:488–94.
Wu M, Kim J, Wei F. Facilitating weight shifting during treadmill training improves walking function in humans with spinal cord injury: a randomized controlled pilot study. Am J Phys Med Rehabil. 2018;97:585–92.
Hitzig SL, Craven BC, Panjwani A, Kapadia N, Giangregorio LM, Richards K, et al. Randomized trial of functional electrical stimulation therapy for walking in incomplete spinal cord injury: effects on quality of life and community participation. Top Spinal Cord Inj Rehabil. 2013;19:245–58.
Hicks AL, Adams MM, Martin Ginis K, Giangregorio L, Latimer A, Phillips SM, et al. Long-term body-weight-supported treadmill training and subsequent follow-up in persons with chronic SCI: effects on functional walking ability and measures of subjective well-being. Spinal Cord. 2005;43:291–8.
Effing TW, van Meeteren NLU, van Asbeck FWA, Prevo AJH. Body weight-supported treadmill training in chronic incomplete spinal cord injury: a pilot study evaluating functional health and quality of life. Spinal Cord. 2006;44:287–96.
Quel de Oliveira C, Refshauge K, Middleton J, de Jong L, Davis GM. Effects of activity-based therapy interventions on mobility, independence, and quality of life for people with spinal cord injuries: a systematic review and meta-analysis. J Neurotrauma. 2017;34:1726–43.
Piira A, Lannem AM, Sørensen M, Glott T, Knutsen R, Jørgensen L, et al. Manually assisted body-weight supported locomotor training does not re-establish walking in non-walking subjects with chronic incomplete spinal cord injury: a randomized clinical trial. J Rehabil Med. 2019;51:113–9.
Piira A, Lannem AM, Sørensen M, Glott T, Knutsen R, Jørgensen L, et al. Robot-assisted locomotor training did not improve walking function in patients with chronic incomplete spinal cord injury: a randomized clinical trial. J Rehabil Med. 2019;51:385–9.
Waring WP 3rd, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A, et al. 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010;33:346–52.
Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Garratt AM, Stavem K. Measurement properties and normative data for the Norwegian SF-36: results from a general population survey. Health Qual Life Outcomes. 2017;15:51. https://doi.org/10.1186/s12955-017-0625-9.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
McAuley E, Mihalko SL. Measuring exercise-related self-efficacy. In: Duda JL, editor. Advances in sport and exercise psychology measurement. Morgantown: Fitness Information Techn, Inc.; 1998. p. 371–81.
Deci EL, Ryan RM. The "what" and "why" of goal pursuits: human needs and the self-determination of behavior. Psychol Inq. 2000;11:227–68.
Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99:1998–2006.
Saebu M, Sørensen M. Factors associated with physical activity among young adults with a disability. Scand J Med Sci Sports. 2011;21:730–8.
Costa R, Probst M, Bastos T, Vilhena E, Seabra A, Corredeira R. Behavioural Regulation in Exercise Questionnaire in people with schizophrenia: construct validity of the Portuguese versions. Disabil Rehabil. 2018;40:2577–84.
Lidal IB, Veenstra M, Hjeltnes N, Biering-Sorensen F. Health-related quality of life in persons with long-standing spinal cord injury. Spinal Cord. 2008;46:710–5.
International Physical Activity Questionnaire. Guidelines for data processing and analysis. https://sites.google.com/site/theipaq/home.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of Changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;5:582–92.
Kim CM, Eng JJ, Whittaker MW. Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord. 2004;42:156–62.
Lam T, Noonan VK, Eng JJ, Team SR. A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord. 2008;46:246–54.
Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–33.
Gervasoni E, Jonsdottir J, Montesano A, Cattaneo D. Minimal clinically important difference of berg balance scale in people with multiple sclerosis. Arch Phys Med Rehabil. 2017;98:337–40.
Ditunno PL, Patrick M, Stineman M, Ditunno JF. Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord. 2008;46:500–6.
Acknowledgements
We thank the three primary rehabilitation centers for SCI in Norway, which have contributed to recruitment of the patients. We appreciate the cooperation with the patients’ organization LARS (National Association of the Spinal Cord Injured) and LTN (National Association of the Traffic Injured). The efforts of the staff, who conducted the body-weight supported locomotor training in Tromsø and Oslo and the work of the test team at Sunnaas Rehabilitation Hospital, are greatly appreciated.
Funding
The study has been financed with the aid of the Norwegian Health Authorities and “EXTRA” funds from the Norwegian Foundation for Health and Rehabilitation. Gjensidige insurance company donated the LOKOMAT® robot.
Author information
Authors and Affiliations
Contributions
AP, AML, KG, NH, RK, SFK, and MS have conceived the study. KG, RK, TG and SFK obtained funding for the study. AP, AML, KG, RK, NH, SFK, and MS participated in its design, all authors contributed (AP, AML, KG, RK, LJ, TG, NH, SFK, and MS) to coordination and manuscript drafting. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
We ensured that this research was conducted with high ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Piira, A., Lannem, A.M., Gjesdal, K. et al. Quality of life and psychological outcomes of body-weight supported locomotor training in spinal cord injured persons with long-standing incomplete lesions. Spinal Cord 58, 560–569 (2020). https://doi.org/10.1038/s41393-019-0401-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0401-2
This article is cited by
-
Combining robot-assisted therapy with virtual reality or using it alone? A systematic review on health-related quality of life in neurological patients
Health and Quality of Life Outcomes (2023)
-
Body weight-supported gait training for patients with spinal cord injury: a network meta-analysis of randomised controlled trials
Scientific Reports (2022)
-
The effects of active upper-limb versus passive lower-limb exercise on quality of life among individuals with motor-complete spinal cord injury
Spinal Cord (2022)