Abstract
Study design
Observational pre-post study.
Objective
Guided internet-delivered CBT (ICBT) offers an alternative approach for mental health service delivery in the community for those with spinal cord injury (SCI). The feasibility and acceptability of guided ICBT programme is available for various chronic health conditions; however, the evidence related to SCI is limited. The primary aim of the current study was to examine feasibility and acceptability of a guided transdiagnostic ICBT programme for persons with SCI.
Setting
Community.
Methods
In this single-group pre-post study, persons with SCI (n = 20) living in the community were provided with a guided 8-week transdiagnostic ICBT programme for overall well-being. Study feasibility was examined by the following outcomes: patient recruitment, engagement, and attrition. Acceptability of the programme was evaluated post-treatment. Reductions in symptoms of depression and anxiety were assessed at baseline, post-intervention, and at 3-month follow-up.
Results
Approximately 60% of eligible participants were recruited. The study found high rates of programme completion (90%) and outcome data were obtained from 90% of participants. Improvement in symptoms of depression (and anxiety) were seen after treatment. Gains were maintained at 3-month follow-up.
Conclusions
Guided transdiagnostic ICBT programme is a feasible and acceptable treatment option for those with psychological needs following SCI.
Similar content being viewed by others
Introduction
Spinal cord injuries (SCIs) have lasting impact on economic stability and mental well-being of both the injured individual and their families. Common secondary health conditions experienced by individuals with SCI include psychological distress, including depression and anxiety, and pain [1]. Approximately 30% of those injured experience clinically significant levels of depression and/or anxiety [2]. Low self-esteem and negative body image can lead to emotional distress among people with SCI [3]. Multidisciplinary SCI rehabilitation programmes based on the biopsychosocial model have been shown to be effective [4, 5]. However, resource limitations can restrict the ability of service providers to deliver these integrative biopsychosocial approaches in the community. A Canadian survey, found that over 37% of individuals with SCI expressed a need for emotional counselling; of these, only 43% felt that these needs were met [6]. This same survey also found that transportation was an issue for these individuals with 87% and 73%, respectively, expressing a need for short- and long-distance transportation. These results are discouraging, as individuals with SCI, who have more social and emotional support and greater access to services in their community, tend to report fewer secondary health conditions [7]. As several barriers exist for service delivery from both the providers’ and the users’ perspectives, there is a great need for cost-effective solutions to improve long-term outcomes among the SCI population in the community.
Previous systematic reviews have found that cognitive behaviour therapy (CBT) is effective in reducing symptoms of depression post SCI [8, 9]. Both studies found small to large effects of CBT on depressive and anxiety symptoms. Dorstyn et al. [8] also found moderate-to-large effect sizes in the improvement of quality of life post CBT treatment in individuals with SCI. In addition, access to computers and the internet among those with SCI has increased in the past decade. Previous studies reported ~70% of persons with SCI had access to the internet [10]; however, recent reports indicate 98% of persons with SCI have daily or weekly access to the internet [11]. Hence, providing CBT via the internet may have several advantages over traditional forms of delivery for overcoming common treatment barriers such as saving therapist time, reducing wait lists, flexible admission of treatment, eliminating travel to in-person appointments, and reducing stigma [12, 13]. In internet-delivered CBT (ICBT), patients receive online education in CBT, which is often combined with weekly support from a therapist or coach via emails or phone calls, but can also be self-directed [13]. There is growing evidence that ICBT benefits individuals with various chronic health conditions, such as tinnitus, fibromyalgia, and rheumatoid arthritis [14, 15].
To date, four studies have examined the use of ICBT in adults with an SCI. One study evaluated its use in pain management [16] and three evaluated use for overall well-being [17,18,19]. The findings have been somewhat mixed in terms of completion rates and outcomes. Overall, the results of these studies suggest that ICBT may be beneficial in improving outcomes among those with SCI. However, completion rates and outcomes may be limited among self-directed programmes.
A feasibility open trial approach was used to inform larger, randomized, controlled trials, especially given the low prevalence of SCI and limited research on ICBT among this population. Given the large dropout rates in previous self-directed trials, the current study aims to evaluate feasibility of a guided approach. The primary objective of the current study is to evaluate feasibility of a guided ICBT programme among those with SCI. Feasibility will be evaluated through participant recruitment, engagement, and attrition, average guide time, and treatment satisfaction. In addition, improvement in symptoms of anxiety and depression along with quality of life will be assessed.
Methods
Study design and ethics
The current pilot study employed a single group pre-post design. The study was registered with ClinicalTrials.gov (NCT03457714) prior to commencement. Ethics approval was obtained from the Institution’s Research Ethics Board.
Participant recruitment and screening
The feasibility study recruited participants with SCI through primary care facilities, rehabilitation hospitals, and community support groups across Canada. Inclusion criteria for persons with SCI included the following: (a) self-reported diagnosis of SCI by a physician; (b) ages 18 years or older; (c) access to a computer and internet services; and (d) willing to provide a physician as an emergency contact. Exclusion criteria for persons with SCI were as follows: (a) high risk of suicide; (b) suicide attempt or hospitalization in last year; (c) primary problems with psychosis, alcohol, or drug problems, mania; (d) currently receiving active psychological treatment for anxiety or depression; (e) not present in Canada during the treatment period; and (f) significant concerns about ICBT.
Intervention
The transdiagnostic ICBT programme, Chronic Conditions Course, is described in more detail elsewhere [16, 20]. The Chronic Conditions Course consists of five lessons based on the principles of CBT that are delivered over an 8-week period. The course is transdiagnostic in that the content applies to both symptoms of depression and anxiety, and has been designed to be suitable for people with a broad range of chronic physical health conditions. The five lessons consisted of the following: (1) the cognitive behavioural model and symptom identification; (2) thought monitoring and challenging; (3) de-arousal strategies and pleasant activity scheduling; (4) graduated exposure and pacing; and (5) relapse prevention. Modifications to the programme included providing background on anxiety and depression relevant to those with SCI. Along with lessons, case vignettes were used to facilitate learning. Although the Chronic Conditions Course is often presented with a range of case stories of adults with different physical conditions and diseases, two of the existing case vignettes were adapted to reflect the experiences of those with SCI, to increase applicability. The adapted cases included one of an individual with chronic pain and another with irritable bowel syndrome. These cases were altered to include presence of an SCI with chronic pain or bowel dysfunction as secondary conditions. A team of experienced SCI clinicians including a psychologist, physiotherapist, and nutritionist were involved in the development of two additional SCI-specific case vignettes. Participants were also asked to complete homework assignments, which involved application of knowledge learned in each lesson. Additional resources that cover topics such as sleep, communication, managing pain, and problem solving were also provided as a part of the course to all participants.
Guide and support
A guide contacted participants through secure email or telephone, based on their preference, to answer any questions regarding the material and to review homework assignments. The guide was a postdoctoral research fellow with training in SCI and ICBT. The guide worked under supervision of registered clinicians (HH and MN). Previous research has demonstrated evidence of non-clinicians’ ability to provide guidance without compromising clinical outcomes or acceptability [21,22,23]. The guide focused weekly contact on (1) answering participant’s questions; (2) reviewing content; (3) encouraging application of skills; (4) normalizing challenges in learning skills. The guide did not provide any new therapeutic skills or therapeutic advice. The guide limited time spent with participants to 10–15 min per week but was allowed to spend more time with the clients if indicated. Participants also received weekly automated email messages informing them about upcoming lessons.
Outcomes
Feasibility was assessed by outcomes including success of patient recruitment, engagement, attrition, and treatment satisfaction [24]. Participant engagement was measured by average time spent with the guide. Programme completion was defined by completing at least four of the five lessons in the course. Completeness of data was evaluated by examining number of participants completing post-treatment and 3-month follow-up measures. Acceptability was measured based on patient satisfaction using the Treatment Satisfaction Questionnaire (TSQ). The TSQ measures reported satisfaction of treatment assessing the overall satisfaction with treatment quality, possibility of recommending treatment to others, and confidence in independently managing symptoms.
Symptoms of depression (Patient Health Questionnaire-9 items (PHQ-9) and anxiety (General Anxiety Disorder-7 items (GAD-7) were assessed at pre-treatment, beginning of each lesson, post-treatment, and at 3-month follow-up. Quality-of-life outcomes, International Spinal Cord Injury Basic Pain Data Set (ISCIBPD), were assessed at pre-treatment, post-treatment, and at 3-month follow-up. Measures for treatment satisfaction and working alliance were administered post-treatment.
Patient Health Questionnaire-9 items
The PHQ-9 is a nine-item questionnaire assessing symptoms of depression over the past 2 weeks. Respondents rate their symptoms on a four-point scale from 0 (not at all) to 3 (nearly every day). Individuals who score a 10 or greater, out of a maximum possible score of 27, are identified as likely having a diagnosis of major depression. The PHQ-9 has been shown to have high internal consistency (α = 0.86–0.89) and good construct validity [25].
General Anxiety Disorder-7 items
The GAD-7 measures general anxiety symptom severity using seven items. Participants rate their symptoms over the past 2 weeks on a four-point scale that ranges from 0 (not at all) to 3 (nearly every day). More severe symptoms of anxiety are associated with higher scores, with a cut-off score of 10 out of 21, indicating a likely diagnosis of generalized anxiety. Psychometric studies show that GAD-7 has excellent internal consistency (α = 0.92) and strong construct validity [26].
ISCIBPD version 2.0 assessed pain interference. The data set comprised three pain interference items (day to day activities, overall mood, ability to get a good night’s sleep) rated on a numeric rating scale of 0 (no interference) to 10 (extreme interference) [27].
The Spinal Cord Injury—Quality of Life (SCI-QOL) measurement system assesses emotional and physical well-being among those with SCI [28]. The SCI-QOL consists of a set of 19 item banks. It demonstrates excellent internal consistency and reliability [29,30,31,32,33,34]. Each item bank may be administered as a full bank or in its short form. Of the 19 item banks, the current study utilized the following six short-form item banks:
- 1.
Ability to participate short-form item bank consists of ten items scored on a five-point scale. Higher scores indicate greater functioning and ability to participate in social roles and activities.
- 2.
Grief/loss short-form item bank consists of nine items scored on a five-point scale. Higher scores indicate greater grief/loss and lower scores represent less grief/loss.
- 3.
Independence short-form item bank consists of eight items scored on a five-point scale. Higher scores indicate greater level of independence.
- 4.
Positive affect short-form item bank consists of ten items scored on a five-point scale. Higher scores indicate more positive affect and wellbeing.
- 5.
Resilience short-form item bank consists of eight items scored on a five-point scale. Higher scores indicate greater levels of resilience.
- 6.
Self-esteem short-form item bank consists of eight items scored on a five-point scale. Higher scores indicate greater level of self-esteem and better functioning.
Statistical analysis
Analyses were conducted using SPSS version 24. Descriptive statistics were provided for participant characteristics and injury factors. Generalized estimation equation (GEE) modelling was used to evaluate changes over time from baseline to 3-month follow-up [35]. An unstructured working correlation structure was applied to account for within subjects’ variances over time. A γ-distribution with a log link response scale was specified to address positive skewness and proportionally changing scores in the dependent variables [36, 37]. Pairwise comparisons were used to examine the statistical significance of changes in the outcomes between the time points.
Results
Demographics and baseline data
Participant’s demographic and clinical characteristics are presented in Table 1. Pre-treatment primary and secondary measure scores are presented in Table 2. Participants on average had mild levels of anxiety (GAD-7 = 8.50) and moderate levels of depression (PHQ-9 = 10.85) symptoms.
Feasibility and acceptability
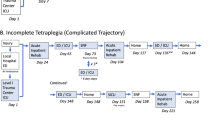
A total of 48 participants completed the online screening (Fig. 1). Applicants who did not meet the inclusion criteria were not Canadian residents (n = 5) or did not have a diagnosis of SCI (n = 8). Thirteen participants that met the inclusion criteria could not be reached by telephone. This resulted in ~60% of participants (a total of 20 participants) meeting the inclusion criteria. On average, five participants were recruited per month. Most participants completed the course, post-treatment measures, and 3-month follow-up measures (90%). Two participants dropped out of the course. One dropped out at week 2 and did not provide a reason for dropping out. The other dropped out at week 3 due to hospitalization unrelated to the programme. Weekly guide email and/or telephone contact on average was estimated at ~14.30 min (SD = 6.18). Of the 18 participants that completed the programme, 89% reported being satisfied or very satisfied with the programme. All participants reported that they would recommend it to others, and that it was worth their time. Eighty-nine per cent of participants reported that the programme helped increase their confidence in self-managing their symptoms.
Depression and anxiety symptom change
Table 2 provides details on means, per cent change, and effect sizes for primary outcomes of GAD-7 and PHQ-9. The GEE analyses revealed significant time effects were seen on both GAD-7 (Wald’s χ2 = 12.72, p = 0.002) and PHQ-9 (Wald’s χ2 = 18.27, p < 0.001). Planned contrasts revealed a significant reduction in GAD-7 and PHQ-9 scores from baseline to post-treatment and from baseline to follow-up (p < 0.001). Scores on the PHQ-9 continued to reduce significantly from post-treatment to follow-up (p = 0.03); whereas no significant difference in GAD-7 scores were seen from post-treatment to follow-up.
SCI-QOL subscales
Overall significant time effects were found on SCIQoL subscales of Grief (Wald’s χ2 = 19.38, p < 0.001), Self-Esteem (Wald’s χ2 = 6.62, p = 0.04), Resilience (Wald’s χ2 = 14.11, p < 0.002), Positive Affect (Wald’s χ2 = 15.92, p < 0.001), and Ability to participate (Wald’s χ2 = 15.68, p < 0.001). Planned contrasts revealed significant improvement in Grief and Self-Esteem at baseline to post-treatment and from baseline to follow-up (p < 0.01). Significant improvement in Resilience and Positive Affect were seen at baseline to post-treatment and from baseline to follow-up (p < 0. 1); these improvements were maintained from post-treatment to follow-up. No significant improvement was seen in ‘Ability to participate’, from pre-treatment to post-treatment; however, significant improvements were revealed at pre-treatment to follow-up and post-treatment to follow-up (p < 0.01). Lastly, planned contrasts revealed significant improvement in ‘Independence from pre-treatment’ to follow-up (p = 0.03), whereas no significant improvement was seen from pre-treatment to post-treatment or from post-treatment to follow-up.
Discussion
The purpose of the current study was to evaluate the feasibility and acceptability of a transdiagnostic ICBT programme for overall well-being among those with SCI. The study demonstrated that delivery of ICBT is feasible in a clinical setting with an SCI population. Guides spent ~15 min per week per participant. In terms of acceptability, participants reported high levels of satisfaction with the programme. The study found high levels of treatment adherence among participants and low levels of dropout. This is in contrast to some previous studies evaluating similar ICBT programmes among those with SCI, which reported greater levels of dropout [17,18,19] These differences may be due to the greater level of guided support provided to those participating in the current study. Previous studies have been predominantly self-directed, whereas the current study provided weekly guide contact to participants. Tailoring treatment to participants through guided support has been shown to be an effective strategy for improving adherence to web-based interventions [38]. In a qualitative study evaluating the barriers and facilitators of ICBT among those with SCI, the authors found that guided support was a strong facilitator in completing the programme [39]. Guided support was found to help improve understanding and the use of materials presented in lessons. It also provided participants with greater level of accountability in completing the programme and homework assignments, similar to that seen in a face-to-face session [39]. In addition, the brief and linear structure of the Chronic Conditions Course may also be a potential facilitator in programme adherence and completion [39]. Previous studied programmes were delivered over a longer period and allowed participants to select modules, as they progressed through the programme [17,18,19]. Further research on the efficacy of more structured vs. unstructured programmes for this population is warranted.
In terms of symptom change, participants experienced reduction in symptoms of anxiety and depression post-treatment and were maintained at a 3-month follow-up. These findings are consistent with a previous study examining the use of ICBT for pain management compared with a wait-list control group among those with SCI [16] and with previous trials of the intervention with other populations [20]. Migliorini et al. [17] found a significant time effect of internet-delivered psychological intervention in improving mood among those with SCI. The findings are also consistent with those found in face-to-face CBT [40] and telephone-based counselling [40, 41] among those with SCI. In addition, although no significant improvements were seen post-treatment for pain interference, SCI QoL independence, and SCI QoL ability to participate outcomes, they were seen at the 3-month follow-up. Hence, it may be that participants’ continued use of the skills learned in the course resulted in improvement over time. Studies evaluating longer-term outcomes are warranted.
This study has several limitations. First, the small sample size limits the study’s ability to draw firm conclusions about the treatment effects. In addition, due to the lack of control group, it is not possible to ascertain the effect of the intervention compared with other factors that may have contributed to the change including natural trajectory of recovery. Other factors such as positive changes in personal health, interpersonal relationship, or other factors may have also contributed to the improvement in symptoms. Larger, randomized, controlled trials may be important in evaluating direct effect of the intervention. Third, the participants in this study may not represent the comprehensive SCI population, as they were predominantly Caucasian, with an incomplete SCI, and paraplegic. Larger studies with a more heterogeneous population may be necessary to further establish the generalizability of the findings. In addition, the sample consisted of an equal proportion of males and females, which may not represent the proportions seen in the general population where males are overrepresented. Future studies examining engaging males may be warranted. Fourth, the study consisted of individuals with mild-to-moderate levels of anxiety and depression symptoms at baseline. Thus, the results from the study may not be generalizable to those with more severe symptoms. The study was limited by its short-term follow-up period of 3 months. Studies evaluating long-term maintenance and improvements in symptoms is warranted. Lastly, the current study relied on self-report measures and the impact on health care utilization or medication use was not evaluated.
Despite these limitations, the findings from the current study have several clinical implications for the use of ICBT in routine clinical care. Specifically, implementation of an ICBT programme among those with SCI should include at least once a week guided support throughout the programme, to help improve adherence. Guidance may not only improve understanding and utilization of material, but also increase accountability among clients. In addition, due to the structured and manualized nature of the Chronic Conditions Course, the programme may be administered by trained professionals using relatively little time with significant effects that are comparable to face-to-face care. This may highlight the potential cost savings of the intervention compared with traditional modes of service delivery, especially when the indirect costs of having patients travel to and attend equivalent face-to-face interventions is considered. Perry and colleagues [42] found costs of transport to multidisciplinary cognitive behavioural pain management programme was a significant barrier to access to services. In addition, the ICBT programme not only reduced negative symptoms of anxiety and depression but also improved quality of life and positive psychosocial factors such as self-esteem, resilience, independence, and ability to participate. Furthermore, due to the transdiagnostic nature of the Chronic Conditions Course, it has the potential to be delivered across other rehabilitation populations.
Future studies examining the use of ICBT in a randomized, controlled trial with larger sample is warranted to establish a stronger evidence base for its effectiveness. Consistent with previous ICBT studies among those with SCI, participants in the current study had mild-to-moderate symptoms of anxiety and depression [16,17,18,19]; future studies evaluating individuals with higher levels of symptoms may be warranted. In addition, examining the efficacy of ICBT in not only improving symptoms of distress but also health care utilization and changes in medication may be important. Future studies should also examine the role ICBT can play in an inpatient setting and, consistent with this recommendation, Lin et al. [43] argue for the potential cost savings and effectiveness of utilizing ICBT approaches in medical rehabilitation.
Conclusions
In conclusion, the findings from the current study provide support for the use of ICBT among persons with SCI. The study demonstrated the feasibility of recruitment efforts for internet programmes. The study found high levels of adherence and satisfaction when guidance is provided to meet the needs of participants. In addition, these interventions have the potential to be cost savings with limited time required for service delivery (~15 mins per week), while also overcoming many of the known barriers to attending face-to-face services. The study resulted in reductions in anxiety and depression symptoms. Improvements were also seen in several quality-of-life dimensions. ICBT is an acceptable and effective form of psychosocial service delivery among those with SCI and mental health concerns.
Data archiving
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Kennedy P, Rogers B. Anxiety and depression after spinal cord injury: A longitudinal analysis. Arch Phys Med Rehabil. 2000;82:932–7.
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47:108–14. https://doi.org/10.1038/sc.2008.115
Lightpole E. Quadriplegia–what I feel. Med J Aust. 1991;154:562.
Nicholson Perry KN, Nicholas MK, Middleton JW. Comparison of a pain management program with usual care in a pain management center for people with spinal cord injury-related chronic pain. Clin J Pain. 2010;26:206–16.
Norrbrink Budh C, Kowalski J, Lundeberg T. A comprehensive pain management program comprising educational, cognitive and behavioural interventions for neuropathic pain following spinal cord injury. J Rehabil Med. 2006;38:172–80.
Noreau L, Noonan VK, Cobb J, Leblond J, Dumont FS. Spinal cord injury community survey: understanding the needs of Canadians with SCI. Top Spinal Cord Inj Rehabil. 2014;20:265–76. https://doi.org/10.1310/sci2004-249
Noonan V, Fallah N, Park S, Dumont F, Leblond J, Cobb J, et al. Health care utilization in persons with traumatic spinal cord injury: the importance of multimorbidity and the impact on patient outcomes. Top Spinal Cord Inj Rehabil. 2014;20:289–301.
Dorstyn D, Mathias J, Denson L. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: a meta-analysis. J Health Psychol. 2011;16:374–91. https://doi.org/10.1177/1359105310379063
Mehta S, Orenczuk S, Hansen KT, Aubut JA, Hitzig SL, Legassic M, et al. An evidence-based review of the effectiveness of cognitive behavioral therapy for psychosocial issues post-spinal cord injury. Rehabil Psychol. 2011;56:15–25. https://doi.org/10.1037/a0022743
Goodman N, Jette AM, Houlihan B, Williams S. Computer and internet use by persons after traumatic spinal cord injury. Arch Phys Med Rehabil. 2008;89(Aug):1492–8.
Post MW, Leenders JM, Tepper M, Snoek GJ, Adriaansen JJ. Computer and internet use among people with long-standing spinal cord injury: a cross-sectional survey in the Netherlands. Spinal Cord 2019;57(May):396–403.
Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13:288–95. https://doi.org/10.1002/wps.20151
Andersson G, Titov N, Dear BF, Rozental A, Carlbring P. Internet‐delivered psychological treatments: from innovation to implementation. World Psychiatry. 2019;18:20–28.
Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost–effectiveness. Expert Rev Pharmacoecon Outcomes Res. 2012;12:745–64.
Mehta, S, Peynenburg, VA, Hadjistavropoulos, HD. Internet-delivered cognitive behaviour therapy for chronic health conditions: a systematic review and meta-analysis. J Behav Med. 2019;42:169–187.
Dear BF, Perry KN, Siddall P, Middleton JW, Johnson J, Katte L, et al. The Pain Course: exploring the feasibility of an internet-delivered pain management programme for adults with spinal cord injury. Spinal Cord. 2018;56:931.
Migliorini C, Sinclair A, Brown D, Tonge B, New P. A randomised control trial of an internet-based cognitive behaviour treatment for mood disorder in adults with chronic spinal cord injury. Spinal Cord. 2016;54:695–701. https://doi.org/10.1038/sc.2015.221
Migliorini C, Tonge B, Sinclair A. Developing and piloting ePACT: a flexible psychological treatment for depression in people living with chronic spinal cord injury. Behav Change. 2011;28:45–54.
Verwer JH, van Leeuwen CMC, Bolier L, Post MWM. Feasibility of an online well-being intervention for people with spinal cord injury: a pilot study. Spinal Cord. 2016;54:473.
Gandy M, Karin E, Fogliati VJ, McDonald S, Titov N, Dear BF. A feasibility trial of an Internet‐delivered and transdiagnostic cognitive behavioral therapy treatment program for anxiety, depression, and disability among adults with epilepsy. Epilepsia. 2016;57:1887–96.
Baumeister H, Reichler L, Munzinger M, Lin J. The impact of guidance on Internet-based mental health interventions: a systematic review. Internet Interventions. 2014;1:205–15.
Robinson E, Titov N, Andrews G, McIntyre K, Schwencke G, Solley K. Internet treatment for generalized anxiety disorder: a randomized controlled trial comparing clinician vs. technician assistance. PLoS ONE. 2010;5:e10942.
Titov N, Andrews G, Davies M, McIntyre K, Robinson E, Solley K. Internet treatment for depression: a randomized controlled trial comparing clinician vs. technician assistance. PLoS ONE. 2010;5:e10939.
Harvey, LA. Feasibility and pilot studies pave the way for definitive trials. Spinal Cord. 2018;56:723–724.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder - the GAD-7. Arch Intern Med. 2006;166:1092–7.
Widerström-Noga E, Biering-Sørensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The international spinal cord injury pain basic data set (version 2.0). Spinal Cord. 2014;52:282.
Tulsky DS, Kisala PA, Victorson D, Tate DG, Heinemann AW, Charlifue S, et al. Overview of the spinal cord injury–quality of life (SCI-QOL) measurement system. J Spinal Cord Med. 2015;38:257–69.
Bertisch H, Kalpakjian CZ, Kisala PA, Tulsky DS. Measuring positive affect and well-being after spinal cord injury: development and psychometric characteristics of the SCI-QOL Positive Affect and Well-being bank and short form. J Spinal Cord Med. 2015;38:356–65.
Tulsky DS, Kisala PA, Victorson D, Tate D, Heinemann AW, Amtmann D, et al. Developing a contemporary patient-reported outcomes measure for spinal cord injury. Arch Phys Med Rehabil. 2011;92:S44–51.
Kalpakjian CZ, Tate DG, Kisala PA, Tulsky DS. Measuring self-esteem after spinal cord injury: development, validation and psychometric characteristics of the SCI-QOL Self-esteem item bank and short form. J Spinal Cord Med. 2015;38:377–85.
Kalpakjian CZ, Tulsky DS, Kisala PA, Bombardier CH. Measuring grief and loss after spinal cord injury: development, validation and psychometric characteristics of the SCI-QOL Grief and Loss item bank and short form. J Spinal Cord Med. 2015;38:347–55.
Tulsky DS, Kisala PA, Victorson D, Choi SW, Gershon R, Heinemann AW, et al. Methodology for the development and calibration of the SCI-QOL item banks. J Spinal Cord Med. 2015;38:270–87.
Victorson D, Tulsky DS, Kisala PA, Kalpakjian CZ, Weiland B, Choi SW. Measuring resilience after spinal cord injury: development, validation and psychometric characteristics of the SCI-QOL Resilience item bank and short form. J Spinal Cord Med. 2015;38:366–76.
Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Lippman SA, Jewell N, et al. To GEE or not to GEE: Comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology 2010;21:467–74.
Karin, E, Dear, BF, Heller, GZ, Gandy, M, Titov, N. Measurement of symptom change following web-based psychotherapy: Statistical characteristics and analytical methods for measuring and interpreting change. JMIR Ment Health. 2018;5:e10200.
Rozental A, Andersson G, Boettcher J, Ebert DD, Cuijpers P, Knaevelsrud C, et al. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interventions. 2014;1:12–9.
Kelders, SM, Kok, RN, Ossebaard, HC, Van Gemert-Pijnen, JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. Journal of medical Internet research. 2012;14:e152.
Mehta S, Hadjistavropoulos H, Earis D, Titov N, Dear B. Patient perspectives of internet-delivered cognitive behaviour therapy for psychosocial issues post spinal cord injury. Rehabil Psychol 2019;64:351–9.
Dorstyn D, Mathias J, Denson L. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: a meta-analysis. J Health Psychol. 2010;16:374–91. https://doi.org/10.1177/1359105310379063
Dorstyn, D, Mathias, J, Denson, L. Applications of telecounselling in spinal cord injury rehabilitation: a systematic review with effect sizes. Clin Rehabil. 2013;27:1072–83.
Perry KN, Nicholas MK, Middleton J, Siddall P. Psychological characteristics of people with spinal cord injury-related persisting pain referred to a tertiary pain management center. J Rehabil Res Dev. 2009;46:57–68.
Lin J, Ebert DD, Lehr D, Berking M, Baumeister H. Internet based cognitive behavioral interventions: state of the art and implementation possibilities in rehabilitation. Die Rehabil. 2013;52:155–63.
Acknowledgements
We acknowledge our funding agencies including the Canadian Institutes of Health Research (CIHR) and Saskatchewan Health Research Foundation (SHRF) for their support. We acknowledge research staff, therapists, and patients associated with the Online Therapy Unit. BFD and the development of the Chronic Conditions Course has been supported by fellowship and grant funding from the Australian National Health and Medical Research Council.
Funding:
This work was supported by Operational and Postdoctoral Fellowship funding provided to SM by the Canadian Institutes of Health Research (CIHR; reference number 293379) and Saskatchewan Health Research Foundation. The project was also made possible in part by CIHR funding provided to HDH (reference number 152917). Funders had no involvement in the study design, collection, analysis, or interpretation of the data. We acknowledge research staff, therapists, and patients associated with the Online Therapy Unit for Service, Education, and Research, at the University of Regina. The development of the Chronic Conditions Course was supported by an Australian National Health and Medical Research Council (NHMRC) Project Grant as well as a NHMRC Career Development Fellowship. This work was supported by infrastructure funding provided by the Canadian Institutes of Health Research (152917). The study was also supported by postdoctoral fellowship funding from the Canadian Institutes of Health Research and Saskatchewan Health Research Foundation. Funders had no involvement in the study design, collection, analysis, or interpretation of the data
Author information
Authors and Affiliations
Contributions
SM conceived the methodology, acquired data, interpreted the results, and drafted the manuscript. HH was involved in designing the methodology, and drafting and revising the manuscript. MN was responsible for acquiring data and drafting the manuscript. EK was responsible for analysing the data and interpreting the results. NT was responsible for drafting and revising the manuscript. BDF was responsible for drafting and revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
I/we certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers/animals were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mehta, S., Hadjistavropoulos, H., Nugent, M. et al. Guided internet-delivered cognitive-behaviour therapy for persons with spinal cord injury: a feasibility trial. Spinal Cord 58, 544–552 (2020). https://doi.org/10.1038/s41393-019-0398-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0398-6
This article is cited by
-
Predictors of resilience for people with spinal cord injury over two periods of COVID-19 social distancing restrictions: a 12-month longitudinal study using structural equation modelling
BMC Public Health (2023)
-
Internet-delivered cognitive behaviour therapy for chronic health conditions: self-guided versus team-guided
Journal of Behavioral Medicine (2022)
-
Resilience and mental health in individuals with spinal cord injury during the COVID-19 pandemic
Spinal Cord (2021)