Abstract
Study design:
Prospective cohort study with a repeated measures analysis.
Objectives:
To measure the effects of the Active Rehabilitation (AR) training programme for community-dwelling individuals with spinal cord injury (SCI) in Botswana on physical independence, wheelchair mobility, self-efficacy, life satisfaction, level of physical activity and community participation.
Setting:
The inaugural AR training programme in Botswana, a community peer-based programme for people with SCI. The 10-day residential programme in Botswana was led by an international team of peer mentors and health professionals.
Methods:
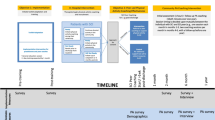
Participants with SCI (on average 4 years after injury) completed a survey comprising a battery of standardised outcome measures at three timepoints: at the start, on completion and at 5 months after the programme (n = 14). Participants also completed a practical wheelchair skills test at start and completion of the programme (n = 17).
Results:
Participants improved in the mobility subscale of the Spinal Cord Independence Measure Self Report on completion (p = 0.011, d = 0.85) and at 5-month follow-up (p = 0.005, d = 0.93) as compared to baseline. They also achieved moderate improvement in self-efficacy to manage their condition (physical function domain of Moorong Self-Efficacy Scale) and large improvements in wheelchair mobility as assessed through the Queensland Evaluation of Wheelchair Skills test and the Wheelchair Skills Test Questionnaire. All positive results were retained at 5-month follow-up.
Conclusions:
Findings indicate that the peer-based programme AR can play an important role in promoting physical independence, wheelchair mobility and injury-management self-efficacy in community-dwelling individuals with SCI in Botswana.
Similar content being viewed by others
Introduction
The implementation of the Spinalis spinal cord injury (SCI)-Rehabilitation Centre at the Princess Marina Hospital in Gaborone in 2013 as a national referral centre contributed to positive outcomes for newly injured individuals with a SCI in Botswana [1,2,3,4]. Recent findings from Botswana show a large reduction in in-hospital and 2-year mortality rates, fewer secondary complications, and higher rates of return to work and education at 2-year follow-up [2, 4]. These positive results were largely attributed to the improved level of care, the higher knowledge among health care professionals working in the area of SCI, the successful implementation of evidence-informed rehabilitation (e.g. bowel and bladder management strategies), the establishment of a service delivery system for assistive equipment, and the high attendance rates of yearly follow-up visits [2, 4].
Nevertheless, community-dwelling individuals with SCI in Botswana still experienced high rates of pressure ulcers and no further improvement in their level of independence between discharge and 2-year follow-up [4]. They also acknowledged the importance of having a strong identity and positive attitude for inclusion in the community, but they expressed feelings of fear, shame and isolation [3]. The role of family, having a source of income and faith in God were also positively commented as key facilitators for inclusion in the community [3]. While contact with peers emerged as an important aspect in the latter study, this was not discussed as being an available source of support for the respondents [3]. Furthermore, lack of accessibility was reported to be one of the main barriers for community participation and integration [3].
The first Active Rehabilitation (AR) training programme in Botswana took place in December 2017 with the aim to address these issues, that is, physical independence, wheelchair mobility, fear, shame, isolation, networking and peer support. The AR concept was first developed in Sweden in 1976, and since then, aspects of the concept have been implemented in more than 20 countries throughout Europe, Asia and Africa [5]. AR training programmes provide opportunities for ongoing rehabilitation to community-dwelling individuals with SCI. Training is led by peer mentors (individuals who have successfully faced a comparable experience) and is primarily delivered through 5–10 days residential courses [5].
Qualitative research indicates that community peer-based programmes are beneficial and important for individuals with SCI [6, 7]. In particular, individuals with SCI describe these peer-led programmes as a life changing experience that have helped them realise what is possible to achieve, develop important skills, become more independent and improve their self-management skills [6, 7]. Despite available positive qualitative and anecdotal evidence, there is a lack of scientific studies that employ standardised outcome measures to explore the effects of residential community peer-based training programmes.
The primary aim of this study was therefore to measure the effects of the inaugural AR training programme for community-dwelling individuals with SCI in Botswana in terms of physical independence, wheelchair mobility and self-efficacy. The secondary aim was to explore the effects on life satisfaction, level of physical activity and community participation.
Methods
This prospective cohort study evaluated the effects of the inaugural AR training programme in Botswana on participants with SCI. Participants were evaluated in the beginning and at the end of the programme, and at 5 months follow-up. The reporting is informed by the STROBE statement for cohort studies [8]. The study protocol was reviewed and approved by the Health Research and Development department, Ministry of Health in Botswana (HPDME 13/18/1). Informed consent was obtained from all included participants. The current study is based on an ongoing collaboration between an international team of researchers and the organisation “RG Active Rehabilitation” in Sweden, aiming to internationally evaluate the effects of the AR concept.
Context
The first AR training programme in Botswana took place in 6–13 December 2017 at the Camphill Community Trust, Otse. The initiative was led by a team from the Swedish organisation RG Active Rehabilitation and the Polish organisation Foundation for Active Rehabilitation (FAR). The team comprised 8 peer mentors with SCI (3 from Sweden, 3 from Poland, 2 local) and 6 non-disabled members from Sweden (1 medical doctor, 1 physiotherapist, 1 occupational therapist, 1 nurse, 2 others) and 2 local non-disabled members (Supplementary Table 1).
The programme was implemented in accordance with the 10 key elements of the AR concept [5]. At the beginning of the programme, the participants were divided into four groups. Similar to AR programmes in other countries, grouping of participants was primarily based on level of physical independence, and it was influenced by sex and age. During the 7-day programme, each group of participants took part in 10 training sessions (overall for 16 h) on wheelchair skills, cardiorespiratory fitness, strengthening and ball sports. In addition, there were 6 workshop-type sessions on the following topics: anatomy and sequelae of SCI; bowel and bladder function and management; pressure ulcers; fertility, sexuality and relationships; health promotion and lifestyle; and the Convention on the Rights of Persons with Disabilities. As in all AR programmes, training of activities of daily living (ADL) was incorporated in the daily schedule as needed, and took place at the natural time and environment.
Inclusion and exclusion criteria
Individuals from Botswana were invited to participate in the AR programme if they met the following inclusion criteria: (1) had a SCI; (2) were using a manual wheelchair as their main mode of mobility and were able to push it for a few metres on an even surface; (3) were at least 18 years of age; (4) were residing in Botswana; and (5) were free of any serious complications such as pressure ulcers. Potential participants were identified through a snowballing method (i.e. word of mouth) and were invited to submit an expression of interest. An on-site project co-ordinator with SCI communicated with these individuals and determined whether they met the inclusion criteria. All information were self-reported and were not confirmed by any medical or physical examination. In terms of the outcome evaluation, participants were excluded from the self-report part of the evaluation if they were not able to understand or speak English.
Outcome measures, procedures and participants
In addition to demographic information, the evaluation included the following primary outcome measures: Spinal Cord Independence Measure self-report (SCIM-SR) [9]; the Queensland Evaluation of Wheelchair Skills practical test (QEWS) [10]; the Wheelchair Skills Test Questionnaire version 4.3 (WST-Q) [11] comprising questions related to capacity and confidence; and the Moorong Self-efficacy Scale (MSES) [12, 13]. The secondary outcome measures included: the Life Satisfaction Questionnaire-11 (LiSat-11) [14]; the Leisure Time Physical Activity Questionnaire for people with SCI (LTPAQ-SCI) [15]; and the Utrecht Scale for Evaluation of Rehabilitation Participation (USER-Participation) [16]. All outcome measures are self-reported except the QEWS that is a short skill-based evaluation. In alignment with the study aims, the outcome measures were identified as primary and secondary [6] based on previous qualitative research findings from community peer-based programmes, and also on what is realistic to achieve in such a short period of follow-up. All self-reported outcome measures were administered in English which is the official language in Botswana.
Consenting participants were invited to complete an online survey administered using the online platform Survey Monkey or the equivalent paper version. Nineteen persons with SCI started the inaugural AR training programme in Botswana, out of whom one dropped out on the third day (n = 18). The number of participants included in the subsequent parts of the analysis varied. Fourteen participants completed all three timepoints of the survey (n = 14); three participants were excluded from this part due to poor English literacy and one dropped out at 5-month follow-up. The QEWS was completed by 17 participants. An on-site research co-ordinator, who is an academic with experience in research, guided participants with completing the survey, and oversaw the administration of the QEWS.
Statistical analysis
The assumption of normality was tested by visually inspecting histograms and by using the Kolmogorov-Smirnov test. In case of normal distribution, a mixed model analysis of variance (ANOVA) for repeated measures with auto-regressive covariance structure was used for variables with three measurements and the paired t-test for variables with two measurements. In case of non-normal distribution, the ANOVA non-parametric Friedman test of variance was performed for variables with three measurements and the Wilcoxon signed-rank test for variables with two measurements (Friedman post-hoc Wilcoxon test with Bonferroni correction). To describe the magnitude of the difference between different times of measurement, the effect sizes (d) were calculated as the difference between means divided by the within standard deviation of the difference. Using Cohen’s [17] criteria, an effect size ≥0.20 and <0.50 was considered small, ≥0.50 and <0.80 medium and ≥0.80 large. All statistical analyses were performed using the IBM Statistical Package for Social Sciences (IBM SPSS Statistics version 24).
Results
Demographics
Among the 19 participants, there were 10 females. Participants presented predominantly with a complete lesion (n = 14) and with an injury resulting in paraplegia (n = 16). On average, they were 31 years of age and had sustained their injury 4 years prior to the AR programme. The group of participants had a wide spread of educational level. Only a small proportion of participants had a paid or unpaid work or studied, with only 3 individuals being engaged in such activities full-time. Table 1 presents demographic information for all participants.
Physical independence and self-efficacy
Participants achieved a higher level of overall physical independence on completion of the programme compared to baseline (p = 0.019, d = 0.79) as indicated by their total SCIM-SR scores (Table 2). These improvements were observed primarily in the mobility subscale where participants achieved an average of 14% improvement in mobility in room and toilet during the programme (p = 0.011, d = 0.85), which was further increased to 20% at 5 months follow-up (p = 0.005, d = 0.93).
In regard to self-efficacy, there were no changes in the total MSES score, or in two out of three constructs of the scale (i.e. general and social constructs). Participants achieved medium size improvements in the personal function construct of the MSES at completion (p = 0.004, d = 0.76) and at 5-month follow-up (p = 0.04, d = 0.63) as compared to baseline. The personal function construct includes seven items that are related to maintaining good health, fulfilling lifestyle, personal hygiene, a satisfying sexual relationship, household participation and getting out of the house [13].
Wheelchair skills
Participants achieved large improvements in their total QEWS score on completion compared to baseline (p = 0.001; d = 0.86) (Table 3). More specifically, participants improved their ability to maintain balance on the back wheels (p = 0.003; d = 0.87), ascend and descend a gutter (p = 0.045; d = 0.72) and covered longer distances during a 6-minute push test (p = 0.003; d = 0.71). A ceiling effect was observed in the first item (negotiating an indoor circuit) which was expected given that the recruitment requirements for the programme mandated that the participants were able to push a manual wheelchair independently.
Similarly, participants reported improvements in both their ability and confidence to handle their wheelchair, as indicated by their WST-Q scores. More specifically, participants reported that their wheelchair skills capacity was improved by an average of 11% between baseline and completion (p = 0.014; d = 0.82), and by 13.5% between baseline and follow-up (p = 0.021; d = 0.77). They also reported a 14% increase in their wheelchair skills confidence between baseline and completion (p = 0.092; d = 0.61), which reached a 25% improvement at 5-month follow-up (p = 0.003; d = 0.96).
Secondary outcomes
There were no significant differences between baseline and 5-month follow-up with regard to the secondary outcomes i.e. life satisfaction (LiSat-11) and community participation (USER-Participation Frequency, USER-Participation Restrictions) (Table 4). Data from LTPAQ-SCI were not analysed as the participants had troubles understanding the concept of leisure time physical activity (LTPA).
Discussion
This study found that the inaugural AR training programme in Botswana had positive effects on participants with SCI on completion and at 5-month follow-up. Participants improved aspects of their mobility in room and toilet (mobility subscale of SCIM-SR) and their self-efficacy in managing their condition (physical function domain of MSES). Participants also advanced their wheelchair mobility as assessed both through a practical test (QEWS) and a self-reported survey (WST-Q). Findings of the current study support those from qualitative studies [6, 7] about the large and important benefits of residential community peer-based training programmes for individuals with SCI.
The inaugural AR programme in Botswana offered a unique opportunity to 19 community-dwelling individuals with SCI to network and interact with an international team of peer mentors. Preliminary evidence suggests that effective peer mentorship employes key transformational leadership behaviours, that is inspirational motivation, idealised influence, individualised consideration and intellectual stimulation [18, 19]. Other studies have associated effective peer mentorship as that fullfiling all three basic psychological needs from the self-determination theory, that is autonomy, competence and relateness [20]. While both frameworks seem highly relevant in the AR conext, the exact repertoire of behaviours and attributes employed by peer mentors in AR programmes have not been explored.
Independence
Despite being 4 years since injury on average, community-dwelling participants of the AR training programme achieved an average improvement of 4.9 points in SCIM-SR between baseline and completion of programme, and further improved for another 0.5 point at 5-month follow-up. According to Scivoletto et al. [21], an improvement of at least 4 points in the total SCIM-III score is considered a small significant improvement and of 10 points a substantial improvement. These scale of improvements in SCIM-III are generally seen during initial in-patient rehabilitation [22]. We could therefore speculate that improvements of the community-dwelling participants with SCI in the current study could be considered as substantial and attributed to the AR programme, despite the lack of a control group.
Lofvenmark et al. [4] reported that individuals with SCI in Botswana achieved no or minimal progress in their median Functional Independence Measure (FIM) score between discharge from the specialised SCI centre and their 2-year follow-up. Findings of the current study indicate that community-dwelling individuals with SCI have the potential to further improve their independence by participating in the AR programme. These findings are in line with qualitative evidence from a community peer-led programme for people with SCI in Fiji, where one of the participants reported “from this course I had big changes… how to live independently; how to push the wheelchair” [7].
Participants also achieved a substantial improvement in mobility in room and toilet between baseline and completion, that was further improved at 5-month follow-up. It has been reported previously that most people attending yearly controls at Spinalis Botswana SCI Rehabilitation Centre in Botswana had access only to an outside toilet and bathroom, and did not return to the home where they lived prior to their injury, but rather moved in with extended relatives [2]. Because of that, they are often not used to that new environment and may have a high need for training addressing specifically those aspects. While this constitutes part of the training during initial in-patient rehabilitation, at 4 years after injury, participants may be more motivated and aware of what exactly they need to improve on.
Self-efficacy
Findings of this study indicate strong improvements in personal function self-efficacy which includes areas that are specific to confidence managing SCI. These results on self-efficacy complement and support the positive gains related to mobility in the room and toilet domain of SCIM-SR. Also, improvements in the SCIM-SR combined with improvements in SCI-specific self-efficacy suggest that participants may be likely to maintain their level of independence in the future.
No improvements were observed in the social function and general self-efficacy. These areas may take longer to improve, similarly to participation and psychological well-being. In a cohort of people with a long-standing SCI (mean of 24 years and range 10–47 years since injury), Cijsouw et al. [23] reported that higher disability-management specific self-efficacy was associated with higher participation and life satisfaction [23]. Furthermore, another study on people with a long-standing SCI reported that fulfilment of peer support need has been positively associated with life satisfaction and specific aspects of participation (i.e. outdoors; health; work/education) [24]. Given that the cohort of the current study was at an earlier point after injury, we could speculate that the increase in the personal function of self-efficacy could potentially contribute to an increase in participation and life satisfaction at a later point and under the condition that the need for peer support is still met.
This mechanism is also supported by qualitative evidence suggesting that participants in this type of community peer-based programmes first improve their knowledge and skills, push their boundaries; then build confidence and engage in self-discovery; and last achieve benefits that are relevant to participation and real life [25]. In this case, it may take longer to improve in regard to self-efficacy in relation to social function and general areas (e.g. making first contact; be persistent when learning something; dealing with unexpected problems; determination in accomplishing something), which may also be more dependent on personal pre-injury core characteristics.
Wheelchair skills
Participants in the current study improved their wheelchair mobility skills, especially in relation to their ability to perform a wheelie, ascend and descend a gutter and also the distance covered during a 6-minute Push Test. Improvements in the practical test were consistent with the positive gains assessed through the self-reported scale. Such findings highlight the importance and benefits from training wheelchair skills even many years after injury. Wheelchair skills are very important for community mobility and have been associated with community participation [26]. Specifically for Botswana, community-dwelling individuals with SCI reported experiencing limitations in accessibility due to lack of ramps, inaccessible public transport, and sandy environments, which had negative implications in social life, work and accessing medical care [3].
The Botswana cohort reported relatively lower baseline scores and gains in wheelchair skills capacity (13.5%) as compared to other studies [27,28,29]. One potential reason is that some participants were using a sub-optimal wheelchair, often related to the wheelchair being too large or too heavy, and to inappropriate accessories such as size and material of front wheels. Also, the psychometric properties of WST-Q may be different in African countries as compared to western-type countries. The high proportion of females in the current study could also explain this discrepancy, as females were previously found to have twice as high odds for unmet needs related to wheelchair skills compared to males in community-dwelling individuals with SCI in Sweden [30]. Nevertheless, findings of the current study indicate that participants improved their wheelchair skills capacity and confidence after completing the AR programme, and that benefits improved further at 5 months follow-up. This implies that the participants continued to practice skills learnt during the programme in their home environment which is required if AR is to have an impact on the participants’ daily life in a long-term perspective.
Large effects were observed on performing a wheelie and on ascending and descending a gutter. These are important skills for community wheelchair mobility that often take a lot of the training time [27]. Large effects were also observed in the distance covered during the 6-minute Push Test. Typically, the training during an AR programme is demanding and includes ball sports and other activities that aim to improve cardiorespiratory capacity and sitting balance. Improvements in distance covered during the 6-minute Push Test could also be associated to better adjustment of the wheelchair and sitting position, as well as more efficient wheelchair technique, all of which are important parts of the AR programme.
Problems with LTPAQ-SCI and USER-Participation in the Botswana context
Many participants in the current study experienced difficulties relating to the concept of LTPA, as well as to some items from the USER-Participation. Both instruments were developed in high income countries, where the concept of leisure is well established. For example, “eating out” and “going to the beach” and “visiting a cafe” may represent very different constructs in a country such as Botswana, especially for people living in more rural areas. Even “going to visit family and friends” and “family or friends coming to visit at your home” may have very different meanings, especially if the constructs of family and home have different meaning. From the discussion between the on-site research co-ordinator and participants of this inaugural AR camp in Botswana it was found that some individuals with SCI considered the term LTPA to be abstract – they undertake physical activities only if they are connected to work or family commitments; never for leisure. For these communities, participation in LTPA would need to be assessed in alternative ways. Future research could explore how to assess participation and LTPA in such contexts, and also in exploring how outcome measures that have been developed in western-type countries can be further adapted in countries within very different contexts.
Strengths and limitations
There are several strengths of this study. It is the first comprehensive and scientifically sound outcome evaluation of community peer-based training programmes for people with SCI in Africa. As such, the project is the first to evaluate the effects of the AR concept in a resource-constrained country. This research project contributes to available [31] and much-needed efforts to evaluate outcomes in residential peer mentoring programmes in a systematic, comprehensive and standarised manner. Another strength is the involvement of persons with SCI throughout the design and conduction of the evaluation. Moreover, the study had a good retention rate at follow-up.
There are also some limitations to the present study. Participants of the inaugural training programme were not entirely representative of people with SCI in Botswana. The cohort comprised predominately women, well-educated individuals who were free of major complications, who could cover transportation expenses and who were motivated to participate in the training programme. This was largely influenced by the snowballing method for recruiting participants, as the on-site project co-ordinator was a woman with SCI who was an activist in gender equality issues. Also, non-English speaking persons were excluded from completing the self-reported part of the study.
The design of the current study could be further improved and adapted to the African context. Given the problems we encountered with the use of specific outcome measures, we propose the use of “Social” and “Empowerment” questions from the World Health Organisation (WHO) community-based rehabilitation (CBR) matrix and indicators [32, 33].
Generalizing results to other African countries, or even to non-metropolitan parts of Botswana must be done with caution. Botswana is rated as a middle-income country and has a relatively well-developed healthcare system and initial SCI management. Also, future programmes may provide a different experience given that they will involve more local leaders and may be better adapted to the Botswana context. Future studies should explore the key behaviours and attributes employed by peer mentors in the AR context, especially in relation to transformational leadership and self-termination theories, whether they are expressed differently depending on peer mentor level of experience, and also how they affect outcomes. Long-term monitoring of the effects of the programmes can indicate whether the outcomes presented in the study can be maintained and even improved in the future when the AR programmes run primarily on local resources.
Last, the lack of a comparable control group limits our ability to claim causality between the AR programme and the observed outcomes. However, the participants had a rather long time since injury, there was a short period between the measurements, and previous evidence from Botswana show lack of improvements in physical independence between discharge from the specialised SCI centre and the 2-year follow-up [4]. It is therefore reasonable to suggest that the outcomes were attributed largely to participation in the AR programme rather than on any other factor. Future studies should employ more robust research designs that should include, but not be limited to, using wider recruitment strategies and finding appropriate methods to use a control group.
Conclusion
Findings of the current study suggest that there is a potential for improvement and a great need for structured training and rehabilitation after discharge for individuals with SCI in Botswana. Participants achieved substantial improvements in their physical independence that are comparable with those in the early period after injury. Peer-based interventions have been described as an overlooked opportunity [34], which can make a difference especially in settings with a shortage of skilled healthcare professionals. Findings of this study indicate that community peer-based programmes in low-resource countries can play a crucial role in promoting healthy and independent active living by providing ongoing support, education and skills training.
Data archiving
All data will be handled and archived to attain confidentiality and will be available from the principal investigator upon reasonable request.
References
Lofvenmark I, Norrbrink C, Nilsson-Wikmar L, Hultling C, Chakandinakira S, Hasselberg M. Traumatic spinal cord injury in Botswana: characteristics, aetiology and mortality. Spinal Cord. 2015;53:150–4.
Lofvenmark I, Hasselberg M, Nilsson Wikmar L, Hultling C, Norrbrink C. Outcomes after acute traumatic spinal cord injury in Botswana: from admission to discharge. Spinal Cord. 2017;55:208–12.
Lofvenmark I, Norrbrink C, Nilsson Wikmar L, Lofgren M. ‘The moment I leave my home - there will be massive challenges’: experiences of living with a spinal cord injury in Botswana. Disabil Rehabil. 2016;38:1483–92.
Lofvenmark I, Wikmar LN, Hasselberg M, Norrbrink C, Hultling C. Outcomes 2 years after traumatic spinal cord injury in Botswana: a follow-up study. Spinal Cord. 2017;55:285–9.
Divanoglou A, Tasiemski T, Augutis M, Trok K. Active Rehabilitation-a community peer-based approach for persons with spinal cord injury: international utilisation of key elements. Spinal Cord. 2017;55:545–52.
Divanoglou A, Georgiou M. Perceived effectiveness and mechanisms of community peer-based programmes for Spinal Cord Injuries-a systematic review of qualitative findings. Spinal Cord. 2017;55:225–34.
Chaffey L, Bigby C. I Feel Free’: the Experience of a Peer Education Program with Fijians with Spinal Cord Injury. J Dev Phys Disabil. 2018;30:175–88.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8.
Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Luthi H, et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2013;51:40–7.
Gollan EJ, Harvey LA, Simmons J, Adams R, McPhail SM. Development, reliability and validity of the queensland evaluation of wheelchair skills (QEWS). Spinal Cord. 2015;53:743–9.
Kirby R, Rushton P, Smith C, Routhier F, Best KL, Cowan R, et al. The wheelchair skills program manual. Halifax, Nova Scotia, Canada: Dalhousie University. https://wheelchairskillsprogram.ca/en/. Accessed Nov 2017.
Middleton JW, Tate RL, Geraghty TJ. Self-efficacy and spinal cord injury: psychometric properties of a new scale. Rehabil Psychol. 2003;48:281–8.
Middleton JW, Tran Y, Lo C, Craig A. Reexamining the validity and dimensionality of the moorong self-efficacy scale: improving its clinical utility. Arch Phys Med Rehabil. 2016;97:2130–6.
Post MW, van Leeuwen CM, van Koppenhagen CF, de Groot S. Validity of the Life Satisfaction questions, the Life Satisfaction Questionnaire, and the Satisfaction With Life Scale in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:1832–7.
Martin Ginis KA, Phang SH, Latimer AE, Arbour-Nicitopoulos KP. Reliability and validity tests of the leisure time physical activity questionnaire for people with spinal cord injury. Arch Phys Med Rehabil. 2012;93:677–82.
Post MW, van der Zee CH, Hennink J, Schafrat CG, Visser-Meily JM, van Berlekom SB. Validity of the utrecht scale for evaluation of rehabilitation-participation. Disabil Rehabil. 2012;34:478–85.
Cohen JW Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Hillsdale, NJ: Erlbaum; 1988.
Beauchamp MR, Scarlett LJ, Ruissen GR, Connelly CE, McBride CB, Casemore S, et al. Peer mentoring of adults with spinal cord injury: a transformational leadership perspective. Disabil Rehabil. 2016;38:1884–92.
Shaw RB, McBride CB, Casemore S, Martin Ginis KA. Transformational mentoring: Leadership behaviors of spinal cord injury peer mentors. Rehabil Psychol. 2018;63:131–40.
Chemtob K, Caron JG, Fortier MS, Latimer-Cheung AE, Zelaya W, Sweet SN. Exploring the peer mentorship experiences of adults with spinal cord injury. Rehabil Psychol. 2018;63:542–52.
Scivoletto G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: how much change is clinically significant for spinal cord injury subjects. Disabil Rehabil. 2013;35:1808–13.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K, et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2011;49:880–5.
Cijsouw A, Adriaansen JJ, Tepper M, Dijksta CA, van Linden S, de Groot S, et al. Associations between disability-management self-efficacy, participation and life satisfaction in people with long-standing spinal cord injury. Spinal Cord. 2017;55:47–51.
Sweet SN, Noreau L, Leblond J, Martin Ginis KA. Peer support need fulfillment among adults with spinal cord injury: relationships with participation, life satisfaction and individual characteristics. Disabil Rehabil. 2016;38:558–65.
Conway T. Exploration of the experiences and perceptions of spinal cord injured people who attend outdoor recreation programmes. Dunedin, NZ: University of Otago; 2010. http://hdl.handle.net/10523/626.
Kilkens OJ, Post MW, Dallmeijer AJ, van Asbeck FW, van der Woude LH. Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 year after discharge from inpatient rehabilitation. J Rehabil Res Dev. 2005;42(3Suppl 1):65–73.
Worobey LA, Kirby RL, Heinemann AW, Krobot EA, Dyson-Hudson TA, Cowan RE, et al. Effectiveness of group wheelchair skills training for people with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2016;97:1777–84.e3.
Kirby RL, Mitchell D, Sabharwal S, McCranie M, Nelson AL. Manual wheelchair skills training for community-dwelling veterans with spinal cord injury: a randomized controlled trial. PLoS ONE. 2016;11:e0168330-e.
Tu CJ, Liu L, Wang W, Du HP, Wang YM, Xu YB, et al. Effectiveness and safety of wheelchair skills training program in improving the wheelchair skills capacity: a systematic review. Clin Rehabil. 2017;31:1573–82.
Divanoglou A, Augutis M, Sveinsson T, Hultling C, Levi R. Self-reported health problems and prioritized goals in community-dwelling individuals with spinal cord injury in Sweden. J Rehabil Med. 2018;10:872–78.
Gassaway J, Jones ML, Sweatman WM, Hong M, Anziano P, DeVault K. Effects of Peer mentoring on self-efficacy and hospital readmission after inpatient rehabilitation of individuals with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2017;98:1526–34.e2.
Mason C, Weber J, Atasoy S, Sabariego C, Cieza A. Development of indicators for monitoring Community-Based Rehabilitation. PLoS ONE. 2017;12:e0178418.
World Health Organisation. Community-based rehabilitation (CBR) 2018. https://www.who.int/disabilities/cbr/en/.
Ginis K, Nigg C, Smith A. Peer-delivered physical activity interventions: an overlooked opportunity for physical activity promotion. Transl Behav Med. 2013;3:434–43.
Acknowledgements
We thank all participants, peer mentors and non-disabled members of the team for their involvement in the study. We also thank Inka Lõfvenmark for providing feedback on the manuscript.
Author information
Authors and Affiliations
Contributions
AD is the principal investigator and designed the study in collaboration with TT and SJ. AD conducted the data analysis and prepared the draft of the manuscript. KT was the programme organizer and collected data at follow-up; SJ contributed to data analysis; CH contributed to organising the programme; KS collected data at follow-up; TT collected data at start and completion, and contributed to data analysis. All authors contributed to the design of the study and ethics application. All authors reviewed the manuscript, provided comments and approved final version of the manuscript.
Corresponding author
Ethics declarations
Statement of ethics
The study protocol was reviewed and approved by the Health Research and Development department, Ministry of Health in Botswana (HPDME 13/18/1). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Divanoglou, A., Trok, K., Jörgensen, S. et al. Active Rehabilitation for persons with spinal cord injury in Botswana – effects of a community peer-based programme. Spinal Cord 57, 897–905 (2019). https://doi.org/10.1038/s41393-019-0300-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0300-6
This article is cited by
-
Relationship between secondary health conditions and life satisfaction in persons with spinal cord injury: study across twenty-one countries
Quality of Life Research (2023)
-
Effects of a rehabilitation program for individuals with chronic spinal cord injury in Shanghai, China
BMC Health Services Research (2020)
-
Understanding how a community-based intervention for people with spinal cord injury in Bangladesh was delivered as part of a randomised controlled trial: a process evaluation
Spinal Cord (2020)