Abstract
Study Design
Psychometrics study.
Objective
The objective of this study was to introduce a novel tool for pinprick sensation examination and validate its usefulness in patients with spinal cord injury (SCI).
Setting
China Rehabilitation Research Center, Capital Medical University School of Rehabilitation Medicine, China.
Methods
A set of cone tools with different tapers (22.5°, 45°, 67.5°, 90°, 112.5°, 135°, 157.5°, and 180°) was made. The cone tool was validated first in 91 able-bodied individuals and then in 30 patients with SCI. The reliability and validity of the cone tool were analyzed by comparing the results of a pinprick sensation examination with the results of the International Standards for the Neurological Classification of SCI (ISNCSCI), the cone tool, and the thermal analyzer.
Results
The intraclass correlation coefficient (ICC) of the cone tool in able-bodied individuals was between 0.48 and 0.94 while that of the cone tool and the ISNCSCI tool ranged between 0.43 and 0.78. Pinprick sensation in patients with SCI can be graded into five levels using four tapers (22.5°, 45°, 67.5°, and 90°): normal, slight impairment, moderate impairment, severe impairment, and complete loss of sensation.
Conclusion
This easy-to-use cone tool can produce a reliable semi-quantitative pinprick test result and is useful for pinprick sensation examination in patients with SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) often impairs nerve conduction and results in reduced or even loss of pain, temperature, and touch sensation [1, 2]. The International Standards for the Neurological Classification of SCI (ISNCSCI) is used in the diagnosis of SCI by examining the pinprick sensation and light touch sensation of key sensory points in combination with the strength of key muscles. To perform a pinprick sensation, a safety pin is used to prick the skin while observing the function of sharp/dull sensation (pain). On the other hand, to test for light touch sensation, a cotton swab is used. The present classification uses a 0–2 scale for pinprick sensation examination of SCI: 0 (no pinprick sensation), 1 (impaired pinprick sensation), and 2 (normal pinprick sensation) [1]. Some merits of this scale include the fact that it is easy to learn and use. A shortcoming of the scale, however, is that it can only provide information about the presence or complete loss of normal function, making it difficult to quantify the results of conditions falling between the two extremes. The scale, therefore, is limited in its ability to evaluate the extent of pinprick sensory dysfunction and the response to treatment [2].
The effective practice of medicine relies on the ability to conduct proper examination and instituting the appropriate treatment. These principles have motivated the development of diagnostic tools and equipment [3]. In the field of neuroscience, a variety of monitoring instruments have been developed to facilitate the measurement and evaluation of sensory function. Rapid technological advancements witnessed in the last three decades have played an important role in the establishment of computerized methods of quantitative sensory testing (QST) comprising classic QST and modern QST [4, 5]. Classic QST includes evaluating temperature, pain and vibration modalities. On the other hand, modern QST involves the measurement of current perception threshold (CPT). Unlike with classic QST measurements, the accuracy and repeatability of CPT measurement is not affected by the skin thickness, elasticity, and general skin temperature variation. Some of the clinical applications of CPT is in the early detection of multiple neuropathies caused by diabetes or HIV. In contrast, classic QST can only detect neuropathies during the hypoesthesia stage in advanced conditions. Although CPT and QST are easy-to-use and have good sensitivity and specificity, these examinations require expensive and bulky instruments, rendering them unsuitable for bedside use.
The Semmes-Weinstein’s monofilament, comprising different diameters, can be used to quantitatively evaluate touch sensation. The monofilament examination was first used in 1954 to examine touch sensation in patients with brain injury [6]. Afterwards, the method was used for screening diabetic foot [7,8,9,10,11]. In recent years, the monofilament examination was used for the quantitative examination of sensory impairment and neuropathic pain in patients with SCI [12,13,14,15,16,17]. We observed 84 cases of SCI from June 2010 to July 2013 and found that the monofilament examination method better reflects the residual light touch sensation than the ISNCSCI examination method [18]. However, the light touch sensation is not comparable to the pinprick sensation in predicting SCI prognosis [2]. Therefore, our study aimed to develop a new examination method of pinprick sensation capable of providing more accurate results.
Methods
Participants
Study approval was granted by the ethics committee of the Capital Medical University School of Rehabilitation Medicine. Written informed consent was obtained from all participants. A total of 91 able-bodied individuals (median age, 28 years; IQR, 25–40 years) were recruited from June 2015 to December 2015 (Supplementary Table 1). A further 33 participants with SCI treated at the China Rehabilitation Research Center were included in the study from June 2016 to July 2016 (Supplementary Table 2). They were diagnosed as having SCI according to the International Standards of Neurological Classification of 2011. The exclusion criteria were: <12 years or >75 years, inability to understand the test instructions; cardiovascular or cerebrovascular diseases; peripheral nerve injuries; skin lesions or scars.
Participants with SCI were aged 12–65 years (median 40 years; IQR, 28 to 48 years) at the time of injury and comprised 29 males and 4 females. The time from injury to the examination ranged from 3 months to 4 years (median 5 months; IQR, 4–15 months). The distribution of participants across the AIS scale, based on the ISNCSCI, was as follows: AIS A (16), AIS B (1), AIS C (9), and AIS D (7). Additionally, 16 participants had paraplegia while 17 had tetraplegia.
Testing of Pinprick sensation
The cone tool has different tapers of 22.5°, 45°, 67.5°, 90°, 112.5°, 135°, 157.5°, and 180° (Fig. 1). During each test, either the cone tool or safety pin was attached to a dynamometer to exert a force equivalent to that produced by a mass of 20 g on the skin. The able-bodied individuals were examined in the sitting position with the forearm in the neutral position. Conversely, participants with SCI were examined either in the supine position in the zone of partial preservation (ZPP) in the case of those with an American Spinal Injury Association Impairment Scale (AIS) A or in areas of decreased sensation in the case of participants with AIS B, AIS C and AIS D. The able-bodied individuals were informed before the examination that the examiner would use a tool to stimulate the dorsal skin of the distal phalange of the middle finger. Thereafter, participants were shown the safety pin and asked to score the sharpness of the stimulation tool on a scale from 0 to 10, where 10 reflected the sharpness of the tip and 0 reflected the bluntness of the round end. For each tool, the examination was performed by examiner #1 for the first time, and by examiner #2 for the second time 24 h later, and by examiner #1 again for the third time 48 h later.
Testing of Thermoception
Thermoception was examined using a thermal analyzer (TSA II NeuroSensory Analyzer, Medoc, Israel). Briefly, a 1.6 × 1.6 cm thermopad was firmly pressed onto participants’ skin. The baseline temperature of the thermopad was 32 °C and was increased or decreased at a rate of 1 °C per second. The maximum and minimum temperatures of the thermopad were 50 and 0 °C, respectively. Heat and cold thresholds were recorded based on participants’ reaction to temperature changes. If no response to temperature changes was observed, the maximum and minimum temperatures, as described earlier, were recorded as the thresholds. Each test was repeated three times and the mean obtained from these values.
Statistical analysis
Statistical analysis was conducted using MedCalc Version 18.11.3. Unpaired data were compared using an independent samples t-test for the normally distributed data or a Mann–Whitney test for the non-normally distributed data. The reliability was assessed using intraclass correlation coefficients and P < 0.05 was considered statistically significant.
Results
Reliability of the cone tool for pinprick sensation in the able-bodied individuals
There were obvious individual differences in the perceptions of sharp and dull sensation in the able-bodied individuals. As shown in the Table 1, the boundary of the sharp/dull sensation was between taper 112.5° and 157.5°. Most of the able-bodied individuals reported a sensation of dullness when stimulated with the cone tools of taper 135°, 157.5°, and 180° (Supplementary Table 3). Since our study aimed to investigate the usefulness of cone tools for pinprick sensation, the cone tools of taper 135°, 157.5°, and 180° were not analyzed further. The intraclass correlation coefficients (ICCs) of the cone tools of tapers 22.5°, 45°, 67.5°, 90°, and 112.5° in able-bodied individuals were between 0.48 and 0.94 (Table 2).
Scoring of the cone tool examination
Results of the cone tool scoring method are shown in Table 3. From this, comparisons of the safety pin examination with the cone tool examination were made (Table 4) (Supplementary Table 4). The medians of cone tool examination results were calculated for each group with ≥5 participants. From the analysis, a median of 8 was derived for the group that displayed a safety pin result of 9 points. On the other hand, similar medians for cone tool examinations were derived for participants who registered safety pin results of 8, 7, and 6 points thereby suggesting good correlation between the two examination methods in these three groups. Finally, the group that registered a safety pin result of 5 points had a median of 4 points in the cone tool examination.
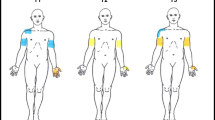
Reliability of the safety pin and cone tool examinations
Among participants with SCI, the ICCs of the different safety pin tests were between 0.73 and 0.78, whereas the ICC of the different cone tools test were between 0.43 and 0.62. Moreover, the ICCs between the results of safety pin and the cone tools was 0.48 for the first test, 0.53 for the second test, and 0.61 for the third test, giving an average ICC value of 0.58 for the three tests (Supplementary Table 5). The average results of safety pin and the cone tools are shown in Fig. 2.
Thermoception examination results
Of the 33 participants with SCI recruited in the study, 3 did not have a thermoception examination due to discomfort they experienced prior to the start of the study. The results of the remaining 30 participants who did have a thermoception examination are shown in Fig. 3 (Supplementary Table 6). The group of participants with safety pin score ≤5 exhibited warm sensation (WS) thresholds of the thermoception examination very close to the maximum 50 °C. Similarly, in the cold sensation (CS) examination, this score revealed CS thresholds ≤5 °C. Moreover, the heat pain (HP) and cold pain (CP) thresholds were very close to the maximum 50 °C and the minimum 0 °C, respectively. Among participants whose safety pin score was ≥8, the median thresholds for the various modalities were: WS (39 °C), CS (25 °C), HP (45 °C) and CP (18 °C). Considering participants whose safety pin score was between 6–7, the median thresholds for all the modalities were between those observed for participants with safety pin scores ≤5 and safety pin ≥8. Further analysis shows that the thermoception examination results for participants with safety pin score between 6 and 7 are statistically different (P < 0.05) from those of participants with safety pin scores of ≤5 and ≥8 (Supplementary Table 7).
Discussion
Our study aimed to develop an easy-to-use tool for determining pinprick sensation with semi-quantitative results. We found that all participants were quick to give a taper score after being stimulated by the safety pin or the cone stool: the able-bodied individuals answered in 1–2 s after stimulation, while those with SCI answered in 1–3 s. We observed individual differences in the perceptions of the boundary of the sharp/dull sensation in the able-bodied individuals (Table 1). The ICCs of the cone tools of tapers 22.5°, 45°, 67.5°, 90°, and 112.5° in able-bodied individuals were between 0.48 and 0.94, suggesting that the reliability was between moderate to high in this class of participants. The average scores for the cone tools with tapers 22.5°, 45°, 67.5°, 90° and 112.5° were very close to 10, 8, 7, 5 and 2, respectively (Table 2). These results imply that the sharpness of the cone tool with taper 22.5° is comparable to the tip end of the safety pin, while the sharpness of the cone tools with tapers 45°, 67.5°, 90° and 112.5° are comparable to safety pin scores of 8, 7, 5 and 2, respectively.
From comparing the results of the safety pin examination with the cone tool examination, the group of participants with SCI who registered a safety pin result of 8, 7, and 6 points had the same median results in the cone tool examination. This signifies good correlation between the two examination methods in these three groups. Overall, towards evaluating the reliability of the two methods in measuring pinprick sensation, ICCs of the safety pin and the cone tool ranged between 0.48 to 0.78. Although less than ideal, these results are, nonetheless, acceptable given that pain is affected by many factors such as emotional, psychological and social [12, 15].
On the basis of the thermoception examination results, impairment in temperature sensation could be graded as: slight impairment (safety pin test results ≥8), moderate impairment (safety pin test results as 6–7) and severe impairment (safety pin test results ≤5). Since pain and temperature sensations are conducted through the same nerve pathways [1, 2], and there was reasonable correlation between the safety pin and the cone tools examinations results, pain sensation (pinprick sensation), therefore, can be categorized into three classes: slight impairment (cone tools test results ≥8), moderate impairment (cone tools test results as 6–7) and severe impairment (cone tools test results ≤5).
Various inferences can be deduced from the results obtained using the cone tools test. A dull sensation to 112.5° and 90° cone tools indicates mild impairment of the pinprick sensation. On the hand, a dull sensation to the 67.5° and 45° cone tools signified moderate and severe impairments, respectively, of the pinprick sensation. Finally, a dull sensation to the 22.5° cone tool represented loss of pinprick sensation.
As reported in Table 2, the inter-examiner reliability was, interestingly, higher than the intra-examiner reliability in the cone tools test. This can, however, be explained by possible changes in the sharpness of the safety pin tip with progression of the study. The safety pin used in our study was made using a regular iron wire which is less durable, and more prone to wearing, than the cone tools made from steel alloy. To prevent systematic errors caused by possible variations in the sharpness of safety pins, we used a single safety pin for all examinations throughout our study. Over the course of the study, it is possible that the safety pin tip experienced some degree of wearing that might have reduced its sharpness. This would potentially result in increased variability in response to pricking as the study continued. Thus, the longer time interval of 48 h, when more wearing would have been experienced, resulted in higher inter-examiner reliability than the intra-examiner reliability. This explanation is also advanced for the observation that there were higher scores of the cone tools during the late phase of the study.
In summary, we have developed a set of cone tools with different tapers of 22.5°, 45°, 67.5°, and 90° for semi-quantitative pinprick sensation examination. Using these tools, impairment in pinprick sensation in patients with SCI can be graded as normal, slight, moderate, severe or complete loss of sensation.
Data archiving
All data used to support the findings of this study are included in this published article.
References
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury. Atlanta, GA, USA: Christopher Reeve Paralysis Foundation; 2008.
Vasquez N, Gall A, Ellaway PH, Craggs MD. Light touch and pin prick disparity in the International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI). Spinal Cord. 2013;5:375–8.
https://en.wikipedia.org/wiki/Precision_medicine, Accessed March 23 2019
Gu S, Du D. Clinical applications and limitations of quantitative sensory testing. Shanghai Med J. 2012;35:341–2.
Shi X, Wang S, Liu X. Thermal quantitative sensory testing and clinical application. Pain Clin J. 2008;4:223–8.
Semmes J, Weinstein S, Ghent L, Teuber HL. Performance on complex tactual tasks after brain injury in man: analyses by locus of lesion. Am J Psychol. 1954;67:220–40.
Lee S, Kim H, Choi S, Park Y, Kim Y, Cho B. Clinical usefulness of the two-site semmes-weinstein monofilament test for detecting diabetic peripheral neuropathy. J Korean Med Sci. 2003;18:103–7.
Kumar S, Fernando DJ, Veves A, Knowles EA, Young MJ, Boulton AJ. Semmes-Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract. 1991;13:63–7.
Hayes KC, Wolfe DL, Hsieh JT, Potter PJ, Krassioukov A, Durham CE. Clinical and electrophysiologic correlates of quantitative sensory testing in patients with incomplete spinal cord injury. Arch Phys Med Rehabil. 2002;83:1612–9.
Ellaway PH, Catley M. Reliability of the electrical perceptual threshold and Semmes-Weinstein monofilament tests of cutaneous sensibility. Spinal Cord. 2013;51:120–5.
Velstra IM, Bolliger M, Baumberger M, Rietman JS, Curt A. Epicritic sensation in cervical spinal cord injury: diagnostic gains beyond testing light touch. J Neurotrauma. 2013;30:1342–8.
Zhang Y, Zhou HJ, Liu GL, Zhang HL, Zheng Y, Hao CX, et al. Treatment of neuropathic pain after spinal cord injury with neurotropin: quantitative sensory testing at the level of human spinal cord injury. Chin J Pain Med. 2014;20:737–40.
Hübscher M, Moloney N, Leaver A, Rebbeck T, McAuley JH, Refshauge KM. Relationship between quantitative sensory testing and pain or disability in people with spinal pain-A systematic review and meta-analysis. Pain. 2013;154:1497–504.
Huang LL, Yu SY. Mechanism of central sensitization in the neuropathic pain. Chin J Pain Med. 2011;8:463–5.
Wang Q, Ni JX. Neuropathic pain after spinal cord injury. Chin J Rehabil Med. 2011;6:588–91.
Cruz-Almeida Y, Felix ER, Martinez-Arizala A, Widerström-Noga EG. Decreased spinothalamic and dorsal column medial lemniscus-mediated function is associated with neuropathic pain after spinal cord injury. J Neurotrauma. 2012;29:2706–15.
Hari AR, Wydenkeller S, Dokladal P, Halder P. Enhanced recovery of human spinothalamic function is associated with central neuropathic pain after SCI. Exp Neurol. 2009;216:428–30.
Liu GL, Li JJ, Zhou HJ, Yun XP, Zheng Y, Zhang Y, et al. The comparison between monofilament test and light touch exam of spinal cord injury and its clinical significance. Chin J Rehabil Theory Pract. 2015;21:990–2.
Acknowledgements
We appreciate the assistance of all participants.
Funding
This study was supported by grants from China Rehabilitation Research Center (NO. 2015CZ-17).
Author information
Authors and Affiliations
Contributions
JL was responsible for designing and writing the study protocol and interpreting the results. GL and HZ were responsible for collecting data and writing the paper. YZ, CH, YZ and BW were responsible for creating “summary of findings” tables and figures. YW, HK and XL were responsible for extracting and analysing data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of ethics
Our study was approved by the ethics committee of Capital Medical University School of Rehabilitation Medicine. Written informed consent was obtained from all participants.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, G., Li, J., Zhou, H. et al. Validation of a novel cone tool for pinprick sensation examination in patients with spinal cord injury. Spinal Cord 57, 747–752 (2019). https://doi.org/10.1038/s41393-019-0283-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0283-3