Abstract
Study design
Systematic review and meta-analysis.
Objectives
The objective was to investigate nutritional status in chronic spinal cord injury (SCI), and compare macronutrient and micronutrient intake to the recommended values by the United States Department of Agriculture (USDA) 2015–2020 Dietary Guidelines for Americans.
Setting
United States of America.
Methods
A MEDLINE/PubMed, Google Scholar, Scopus, and Web of Science search was performed, identifying 268 papers. All papers included were English-language papers examining adults with chronic SCI. A meta-analysis was performed to produce weighted averages and 95% confidence intervals (CI) when summary statistics were provided.
Results
The systematic review included 15 articles, while the meta-analysis included 12. Resting metabolic rate (1492 kcal/day; CI: 1414–1569) fell below the able-bodied average, and total energy (1876 kcal/day; CI: 1694–2059) and fiber (17 g/day; CI: 14–20) intake were below USDA guidelines. Protein (319 kcal/day; CI: 294–345) and carbohydrate (969 kcal/day; CI: 851–1087) intake were above guidelines. Fat intake (663 kcal/day; CI: 590–736) was within USDA guidelines. Vitamins A, B5, B7, B9, D, E, potassium, and calcium were deficient, while vitamins B1, B2, B3, B12, C, K, sodium, phosphorus, copper, and zinc were in excess according to USDA guidelines. Vitamin B6, iron, and magnesium were within USDA guidelines.
Conclusion
Findings indicate greater energy intake relative to energy needs in those with chronic SCI, and an imbalance in fiber intake and micronutrients compared to the USDA guidelines. Future research examining nutritional health status is needed in order to establish evidence-based, SCI-specific dietary guidelines.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) results in the loss of neurological function below the level of injury (LOI) and an increased risk of morbidity and mortality. The neurological impairment leads to deterioration in body composition, characterized by a profound reduction of lean body mass (LBM) and an increase in adipose tissue below the LOI [1]. Loss of LBM results in reductions in resting metabolic rate (RMR), which in turn significantly decreases total daily energy expenditure (TDEE). These changes accelerate the accumulation of adipose tissue, contributing to an obesity epidemic in the SCI population [2]. Recently, advancements in acute medical care and a greater understanding of long term, chronically acquired complications of SCI have increased life expectancy [3], but are associated with increased risk for developing chronically acquired metabolic disease, such as type two diabetes mellitus and cardiovascular disease [1, 2, 4, 5].
Adoption of a healthy diet is generally recommended to individuals with SCI because of the protective function on body composition and cardiometabolic profiles. However, despite the publication of numerous, somewhat contentious recommendations [5,6,7,8,9,10], there are currently no evidence-based nutritional guidelines for individuals with chronic SCI. The lack of agreement on nutritional guidelines may arise from the inability to accurately measure the energy intake and needs of individuals with SCI relative to alterations in body composition following the injury [11,12,13]. Despite an understanding of accelerated aging in this population and the impact of a high caloric diet on obesity, much of the available nutritional research has only been conducted during the acute phase of the injury [10, 14, 15]. Evaluating the available body of literature examining nutritional health status in individuals with chronic SCI may ultimately help establish evidence-based dietary guidelines for persons with SCI.
The aim of this systematic review and meta-analysis was to investigate nutritional status in adults with chronic SCI, focusing on RMR and the intake of total energy, carbohydrate, protein, fat, alcohol, and fiber, as well as intake of vitamins and minerals. Additionally, we aimed to compare the weighted averages for macronutrients and micronutrients to the United States Department of Agriculture (USDA) 2015–2020 Dietary Guidelines for Americans [16]. In this review, we define chronic SCI as one or more years after the injury, to ensure that stabilization of body composition, hormonal profiles, residual neurological function, and the inflammatory environment of the spinal cord is significantly decreased or no longer present [1, 2].
Methods
Database search and article selection
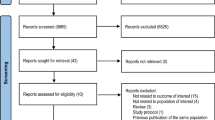
This review was conducted according to guidelines set forth by the National Academy of Medicine [17]. All articles were identified through a comprehensive literature search. The search was completed through MEDLINE/PubMed, Google Scholar, Scopus, and Web of Science utilizing the following limits: English language only, human subjects/patients, and adult participants ≥ 18 years. Search terms were selected from known original research studies and the Medical Subject Headings in MEDLINE/PubMed relevant to the title and/or abstracts. Search terms included: spinal cord injury, tetraplegia, and paraplegia; basal metabolic rate, resting metabolic rate, and resting energy expenditure; diet, energy intake, nutrition, food, foodstuffs; macronutrients, carbohydrates, fat, protein, alcohol, fiber; micronutrients; vitamins A, B1, B2, B3, B5, B6, B7, B9, B12, C, D, E, and K, niacin, folic acid, pantothenic acid, biotin; minerals, sodium, potassium, calcium, magnesium, copper, phosphorous, iron, zinc, and selenium (see supplemental file 1 for the search strategy). Study selection was made by first reviewing the title and abstract, followed by the full text of the articles (carried out by GJF and MAP) (Fig. 1). The above-mentioned databases were searched for articles published since the inception of the database to February 2018. Reference lists of identified articles and relevant review papers were also reviewed to find any additional relevant articles.
Exclusion and inclusion criteria
Article exclusion criteria were as follows: titles or texts of research articles not in the English language; articles without abstracts; case studies because of low level of IV evidence [18]; review and duplicate articles, and commentaries; articles in which demographic information of the study participants were not sufficiently indicated; articles with non-human samples (i.e., animal or cell studies); articles with acute SCI (i.e., <1 year post injury); and participants with SCI < 18 years of age. Participants under one-year of injury were excluded because at this time there is a higher incidence of injury-related complications [1], a period of catabolic stress [19] and negative nitrogen balance that is characterized as a loss of fat free mass [20, 21]. Full articles that were inaccessible through database searches were retrieved through Interlibrary Loan services (a literature borrowing service; n = 5). If articles by the same lead authors were identified and discovered to include similar participants and dietary values, the study with the largest sample size was included [22]. The first two authors independently assessed the quality of the papers included in this review according to the Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields (supplemental file 2) [23].
Data extraction
When studies fulfilled the eligibility criteria, data were extracted from full text studies by a single reviewer (GJF) and verified by a second reviewer (MAP). Data were extracted regarding study design; country of study origin; time since injury; injury completeness; LOI; RMR; total intake of energy, protein, fat, carbohydrate, alcohol, and fiber; total intake of vitamins A, B, C, D, E, and K; and total intake of minerals calcium, copper, iron, magnesium, phosphorus, potassium, sodium, and zinc. Baseline data were extracted from longitudinal studies (i.e., prospective analysis) and included in this review. When relevant data were unavailable, we contacted the corresponding and/or senior authors.
Data and statistical analysis
All nutritional data are reported as mean ± standard deviation (SD) as a measure to be consistent with published research. However, when articles published their results as mean ± standard error of the mean, the standard error of the mean was converted to a SD using the following formula:
where SD is the standard deviation, SEM is the standard error of the mean, and n is the sample size from the article [22]. When articles presented their findings by subgroup analysis (i.e., male and female), a weighted group mean and pooled SD was calculated for each article using the following formula:
where w is the weighted mean, s is the number of subgroups, x is the mean, n is the subgroup size, and N is the whole cohort size [24]. The conversion factors of 4, 4, 7, and 9 were used to convert grams of carbohydrates, protein, alcohol, and fat to calories, respectively. When articles presented micronutrients in International Units (IU), they were converted to their metric equivalent using the National Institutes of Health’s previously published conversion factors [25].
The inter-reliability of the quality ratings of the papers was examined with the intraclass correlation coefficient using thresholds according to Landis and Koch [26]. A linear mixed-effects model, using the R package metafor [27], was used to conduct the meta-analysis. The random effects were fitted with a restricted maximum-likelihood estimator. Forest plots are provided for specific variables that include summary-level effects and 95% confidence intervals (CI) as provided by the random effects meta-analysis. Heterogeneity was calculated via the linear mixed-effects model and was examined using the Q statistic, while inconsistency was assessed using I2. All statistical analyses were conducted using R (R Foundation for Statistical Computing, Vienna, Austria) version 3.4.3.
Results
Description of the included studies
The literature search produced 268 articles investigating nutritional status in SCI. Thirty-six (13%, 36/268) of these articles were selected for a more detailed review (Fig. 1). Seven of these articles (19%, 7/36) were eliminated because participants were less than one-year post injury [28,29,30,31,32,33,34]. Six additional articles (17%, 6/36) did not report time since injury and were therefore excluded [35,36,37,38,39,40]. One study (3%, 1/36) was excluded because the authors did not report macronutrient or micronutrient values for their participants [41], whereas another study (3%, 1/36) inadequately reported research methodology and characteristics of the study population [42]. Three articles (8%, 3/36) were excluded because they were commentary or review articles. Four articles (11%, 4/36) with the same leading author included similar participant characteristics and mean dietary values [22, 43,44,45], so the study with the largest sample size was included while the remaining articles were excluded (Fig. 1) [22]. The remaining 15 articles (42%, 15/36) were included for analysis in this review (Fig. 1). Inter-observer agreement for the total score of the quality ratings was 0.69, denoting substantial agreement [26].
Table 1 presents study and demographic and injury characteristics across SCI nutrition literature. Twelve of the identified articles were cross-sectional (80%, 12/15), while three articles were longitudinal (20%, 3/15) [46,47,48]. Over half of the articles (53%, 8/15) were carried out in the United States of America and the remaining articles were performed in Canada (20%, 3/15) [49,50,51], Iran (13%, 2/15) [22, 52], United Kingdom (7%, 1/15) [47], and Switzerland (7%, 1/15) [53]. Time since injury ranged from 1 to 40 years post injury. LOI ranged from C1 to L4 [12, 13, 22, 46, 47, 49, 53,54,55,56]; however, six articles (40%, 6/15) did not indicate the specific injury levels of their participants [11, 22, 48, 50,51,52]. Six of the articles (40%, 6/15) reported their participants as motor complete injuries (ISNCSCI A and B) [12, 46, 47, 53,54,55], while five articles (33%, 5/15) included samples with complete and incomplete injuries [11, 22, 49, 50, 52]. Four articles did not report injury completeness (27%, 4/15) (Table 1) [13, 48, 51, 56].
Resting metabolic rate, energy intake, and macronutrients
Table 2 presents RMR and caloric intake data across SCI nutrition literature. Only Gorgey et al. [55], Gorgey et al. [46], Lee et al. [56], Nightingale et al. [47], and Perret and Stoffel-Kurt [53] (33%, 5/15) reported a measured RMR value (Table 2). The majority of the articles (87%, 13/15) reported energy intake [11,12,13, 22, 46,47,48, 50, 51, 53,54,55,56]. Twelve articles (80%, 12/15) reported daily fat and carbohydrate intake [11,12,13, 22, 46,47,48, 50, 51, 53,54,55], while protein intake was assessed in 13 articles (87%, 13/15) [11,12,13, 22, 46,47,48,49,50,51, 53,54,55]. Four articles (27%, 4/15) reported daily fiber intake [13, 22, 48, 51]. Daily alcohol intake was only assessed by two articles (13%, 2/15) (Table 2) [12, 47].
Vitamins
Three articles (20%, 3/15) evaluated the daily intake of vitamin A (mean range [lowest to highest mean]: 1.1–6.3 mg/day) [12, 48, 53], while vitamin D was investigated in six articles (mean range: 1.5–5.6 µg/day) [11, 12, 49, 51, 53, 54]. Doubelt et al. [49] and Perret and Stoffel-Kurtet [53] reported daily vitamin K values of 193 ± 212 and 195 ± 51.2 µg/day, respectively. Daily vitamin C intake was assessed in six articles (40%, 6/15), where a mean range of the vitamin was 73.1 to 195 mg/day [11,12,13, 48, 51, 53]. Levine et al. [48] and Perret and Stoffel-Kurt [53] (14%, 2/15) examined daily intake of vitamins E (8.7 ± 5.1 and 8.9 ± 2.4 mg/day) and B5 (4.0 ± 2.2 and 4.5 ± 1.2 mg/day). Vitamins B1 (mean range: 1.3–1.7 mg/day), B2 (mean range: 1.5–1.9 mg/day), and B3 (mean range: 14.5–20.9 mg/day) were reported by three articles (20%, 3/15). Daily intake of vitamins B6 and B12 were reported by four articles (27%, 4/15) with a mean range of 1.3 to 2.1 mg/day and 3.0 to 5.0 μg/day, respectively [12, 48, 51, 53], while Perret and Stoffel-Kurt [53] evaluated vitamin B7 and presented a mean value of 36.2 ± 18.0 µg/day. Vitamin B9 was assessed in six articles (40%, 6/15), where the mean range was 163.4 to 535.9 µg/day [11,12,13, 48, 51, 53]. Walters et al. [50] examined vitamins A, B1, B6, B9, and C, but did not report mean values.
Minerals
Daily calcium intake was assessed in over half of the articles (60%, 9/15). The mean range for daily calcium intake was 543.2 to 1077 mg/day [11,12,13, 48, 49, 51,52,53,54]. Five articles (33%, 5/15) evaluated daily intake of sodium (mean range: 1949–3582 mg/day) [12, 13, 48, 51, 53], phosphorus (mean range: 959.7–1563.0 mg/day) [12, 48, 51,52,53], and iron (mean range: 11.8–19.7 mg/day) [12, 13, 48, 51, 52]. Four articles (27%, 4/15) evaluated zinc where the mean ranged from 8.4 to 10.3 mg/day [48, 49, 51, 53]. Three articles (20%, 3/15) reported daily intake of potassium and magnesium with a mean range of 1935–3478 mg/day and 224–372 mg/day, respectively [48, 51, 53]. Only Levine et al. [48]. evaluated daily intake of copper (1.1 ± 0.3 μg/day) and selenium (94.7 ± 31.6 μg/day). Walters et al. [50], evaluated magnesium and iron; however, the authors did not report the values.
Meta-analysis
Of the 15 articles included in this review, summary statistics were provided in 12 articles and were therefore included in the meta-analysis. Weighted averages for age, weight, body mass index, and time since injury were 38.7 y (95% CI: 35.1, 42.3; n = 573), 75.8 kg (95% CI: 70.4, 81.3; n = 207), 24.2 kg/m2 (95% CI: 21.8, 26.5; n = 166), and 12.4 y (95% CI: 9.7, 15.1; n = 557), respectively. Random effects summary results are presented in Fig. 2 for RMR. Figure 2 and Table 3 present random effects summary results for total energy, protein, carbohydrate, fat, and fiber intake, while Table 4 presents findings for vitamins and minerals. Daily alcohol intake is presented in Table 3.
Forest plots of resting metabolic rate (RMR), energy intake, macronutrients (protein, fat, and carbohydrates), and fiber in individuals with chronic SCI. Black squares indicate the weight of the evidence from each of the studies, the black diamond is the total mean difference, and the width of the diamond indicates the 95% confidence intervals (CI). Total number of participants (N) and the weighted averages with 95% CI are provided for each variable
Discussion
Individuals with SCI are at risk for multiple nutritional deficiencies. The causes are often multifactorial [2, 55], and result in an elevated risk of obesity and obesity-related diseases [1]. Results from this review provide weighted averages for variables associated with the nutritional status of individuals with chronic SCI. They also demonstrate that the majority of the available literature focuses solely on the role of total energy intake, with only a few inconsistent studies evaluating vitamins and minerals. Furthermore, results reported among the articles demonstrated high heterogeneity likely due to LOI, injury completeness, sex, and time since injury among participants. While no fewer than 24 developed countries and the World Health Organization have published separate dietary guidelines, the authors have selected the USDA 2015–2020 Dietary Guidelines for Americans as their reference point since the majority of the study populations represent U.S.A. participants and many of the articles also reference the widely distributed and accepted guidelines [6, 16, 57].
Resting metabolic rate, energy intake, and macronutrients
Previous literature suggests that many individuals with SCI have excessive caloric intake relative to their energy needs [12, 13, 22]. This discrepancy suggests that positive energy balance is leading to a state of obesity and associated cardiometabolic dysfunction [4]. Studies comparing RMR between individuals with chronic SCI and the able-bodied (AB) population note that those with SCI require 10% fewer calories than their AB counterparts [58,59,60]. However, in a 2000 kcal/day diet, this equates to a caloric restriction of 200 kcal/day, which arguably is insufficient to promote negative energy balance [2], and an additional 100 to 200 kcal/day (totaling 300 to 400 kcal) should be restricted [2, 46]. In this review, we demonstrate a mean RMR of 1492 kcal/day. This number fell below the normal range of 1593.5–2248.8 kcal/day for RMR reported within the AB population [61,62,63], and is likely due to a decrease in metabolically active tissue [1, 59, 64, 65]. Mean energy intake was 1876 kcal/day, which was under the total energy intake for all age groups except for females over 31-years of age, according to the USDA guidelines [16]. Individuals with SCI often consume significantly fewer calories than their AB counterparts, not only due to decreased metabolic needs but also as a means to control bowel and bladder programs [66, 67]. Given the greater prevalence of males with SCI than females [68, 69], the averages presented in this review may not accurately reflect the total energy intake of females with SCI. Therefore, these results should be interpreted with caution and promote future investigations.
Interestingly, using the product of RMR and the correction factor of 1.2 to estimate TDEE, a method commonly used in the AB population, yields an energy expenditure of 1790.4 kcal/day. When compared against the mean energy intake calculated for the SCI population of 1876 kcal/day, this value equates to an excess caloric intake of 85.6 kcal/day. These additional calories, seemingly inconsequential, add up to almost 600 kcal/week. Furthermore, this equation likely overestimates TDEE, as it is only validated for the AB population and does not account for the significant loss of LBM affecting energy expenditure and a sedentary lifestyle following SCI. A caloric deficit of 15 to 20% may provide the necessary energy restriction to manage body fat and cardiometabolic profiles following SCI. Of note, injury level and completeness of injury significantly impact caloric needs. Those with tetraplegia and complete injuries require less energy compared to individuals with paraplegia and incomplete injuries [12, 22, 52]. Nonetheless, for the SCI population, these data indicate that excessive energy intake in the presence of diminished LBM and RMR leads to improper energy balance and contributes to a state of obesity and obesity-related comorbidities.
Protein intake in individuals with SCI exceeds current USDA guidelines [16]. This finding is in agreement with previous literature, as most individuals in the United States consume either an adequate or above average amount of protein [12, 13]. Regardless of age, individuals with SCI also consume a significantly greater quantity of carbohydrates than what is recommended values (Table 4) [16]. Ingested carbohydrates not immediately metabolized for energy are stored as fat in visceral, subcutaneous, and inter-muscular and intra- muscular locations [8], which could contribute to the high prevalence of obesity and disorders of carbohydrate metabolism, such as insulin resistance and type two diabetes mellitus, in this population [1, 2, 64]. With regards to fat, we have demonstrated that fat intake remains within the recommended daily allowance for men with chronic SCI. Females over 31-years of age, however, may be consuming a greater quantity, which contrasts previous literature suggesting that individuals with chronic SCI consume an amount of fat that approaches or exceeds that recommended by the USDA guidelines [11,12,13, 16, 22, 53].
Fiber intake in this population has been demonstrated as low [13, 22, 48]. In the current review, we report a mean fiber intake of 176 g/day, which fell below the USDA recommended value of 22.4–33.6 g/day (age and sex dependent) [16]. These guidelines, however, conflict with the Academy of Nutrition and Dietetics Evidence Analysis Library (ANDEAL) recommendations to consume 15 g of fiber per day and increase up to 30 g/day as tolerated following a SCI [7]. Regardless of the chosen guidelines, the results from the present review demonstrate individuals with chronic SCI are either below the recommended intake of fiber per day according to the USDA, or at the lower margin of the ANDEAL recommendations. The ANDEAL guidelines do not differentiate acute versus chronic SCI and are almost ten years old, which may not adequately reflect the aging SCI population and advances in science [70,71,72,73,74]. A likely explanation for a low fiber diet in individuals with SCI is that high fiber diets may cause negative consequences on bowel function and bowel care programs. Fiber consumption that is too high without commensurate fluid intake can lead to constipation with an already decreased bowel motility.
Alcohol consumption also fell below the guidelines. The USDA guidelines limit alcohol intake to no more than two drinks/day for men and one drink/day for women, where a drink of beer (5% alcohol) is 12 fl. oz., a drink of wine (12% alcohol) is 5 fl. oz., and a drink of 80 proof distilled spirits (40% alcohol) is 1.5 fl. oz [16]. According to these guidelines, an alcoholic drink-equivalent is described as containing 98 kcal (0.6 fl. oz.) of pure alcohol [16]. In the present review, daily alcohol intake was 57 kcal/day. This was conducted in a small sample of 33 individuals, and is likely very low given the reports of high alcohol consumption in the SCI population [75,76,77]. Participants are also likely to underreport their true alcohol consumption given the stigma that is often associated with alcohol consumption and its effects on weight and health [77].
Micronutrients
Several vitamins and minerals were below daily recommended 2015–2020 guidelines set by USDA [16]. This review demonstrates deficiencies in vitamins A, B5, B7, B9, D, and E, and the minerals potassium and calcium. Previous research has similarly demonstrated below-recommended intake values of vitamins A, B5, B7, C, D, and E in individuals with chronic SCI [12, 13, 50, 53], as well as deficiencies in the minerals calcium, magnesium, and potassium [12, 16, 48, 50, 53]. Many of these micronutrients are linked to carbohydrate, lipid, and/or vascular dysfunction, which are prevalent in individuals with chronic SCI, and are needed to ensure proper cellular health, water and nutrient transport, and acid-base balance [2, 4, 64]. A potential mechanism driving these deficiencies in micronutrients may be a consequence of a caloric intake below-recommended values. However, previous literature indicates vitamin and mineral supplementation in the SCI population is common, although concrete evidence on this matter is scarce [8]. Nonetheless, as indicated in this review, those with chronic SCI are deficient or in excess of several micronutrients according to USDA guidelines [16], and therefore future research needs to determine adequate intake of vitamins and minerals for this population to counteract any deficiencies and potential toxicities.
Limitations and strengths of this review
This review is not without limitations. First, our search strategy was limited to articles only in the English language, which may have resulted in exclusion of studies that otherwise met our study criteria. Second, many of the articles had small samples and heterogeneous data as indicated by our Q and I2 statistics. We did not account for injury completeness and level and sex-based differences in energy consumption, and acknowledge both variables impact nutrition [16, 68]. However, given the limited number of studies evaluating nutrition in chronic SCI the authors of this review felt pooling samples would provide more power. Third, many articles reported incomplete characteristics in their study population with respect to time since injury, injury classification, RMR, energy intake, macronutrients, and micronutrients. These limitations affected the accuracy and proficiency of the review to unequivocally identify representative values for the SCI population, and thus limit the meaning and significance of our findings. Nonetheless, to the authors’ knowledge, this is the first comprehensive evaluation of nutritional health status in chronic SCI.
There are many strengths of this systematic review and meta-analysis. First, to the best of our knowledge, we are the first to quantitatively assess nutritional health following SCI given previous reviews have been qualitative in nature [6, 8, 57, 78]. Second, although the total number of articles included in the meta-analysis was relatively low, the number of participants was relatively high. Third, full text articles were assessed and evaluated, with substantial agreement, by two authors. Fourth, we performed a comprehensive literature search through multiple databases with strict inclusion and exclusion criteria. Lastly, we focused on chronic SCI to ensure changes in body composition had stabilized to limit the impact of an acute SCI (<1-year post injury) on nutritional health.
Nutritional assessment and recommendations in chronic SCI
A concern in SCI is inadequate assessment of nutritional intake. Numerous studies use dietary recall and food frequency questionnaires with inconsistent collection frequencies. This may lead to the underreporting of energy intake in studies assessing nutritional health following SCI [11,12,13, 55, 79], and therefore the inadequate estimation of energy intake. Additionally, individuals with tetraplegia may have significant difficulty estimating, performing, and reporting standard dietary measurements on survey instruments due to impaired hand function. Utilizing a system where a dietitian calls a participant and collects a 24-h dietary recall over the phone, and/or implementation of assistive technology, such as the Automated Self-Administered 24-h (ASA24) dietary assessment tool, may help minimize the potential to underreport in research trials.
Professional dietary evaluation is a vital tool in preventing and managing nutritional inadequacies in this special population. However, individuals with chronic SCI may not need the USDA recommended values given the anatomical and physiological changes that occur following the injury. These changes include a reduction in neurotrophic influences, sympathetic nervous system blunting, loss of LBM with a commensurate loss of energy expenditure, a decrease in anabolic hormones, and an increase in catabolic hormones [1, 2, 80]. In fact, the USDA guidelines have not been validated in the SCI population given these aforementioned changes [16]. Therefore, we should recognize the significance of dietary assessments and nutrition education and counseling, and recommend to health care professionals that an initial evaluation of diet and subsequent routine visits from a registered dietitian (RD) be a repetitive part of the annual medical assessment and standard of care for individuals with SCI. RD can explore SCI-related dietary issues including the avoidance of food groups, which may affect bowel and/or bladder programs, gluten, glucose, acid reflux, and changes in taste acuity. Moreover, nutritional evaluations by RD often discover psychosocial factors that can have direct or indirect adverse consequences on nutrition. These factors include disordered eating due to impulse control issues or to body dysmorphia, a lack of education regarding nutrition following a SCI or even basic nutritional needs, anxiety and/or depression regarding eating skills and abilities, lack of transportation and assistance to buy and/or use foodstuffs, and substance abuse displacing nutrition [81].
Future direction
Nutritional health in individuals with chronic SCI remains an area of medicine that requires additional research. Future research needs to examine energy needs in relation to energy expenditure (through the assessment of RMR) and body composition among those with paraplegia and tetraplegia compared to the AB population. Prospective studies are also needed to assess the impact of exercise-based and dietary-based interventions, aiming to improve cardiometabolic profiles by increasing LBM and attenuating adipose tissue through functional electrical leg cycle ergometry and caloric restriction [46, 80, 82, 83]. With these studies it is not only imperative to provide high nutrient-dense foods, but also palatable foods to ensure participants adhere to the study protocol. Modeling diets after the Mediterranean, Ketogenic, or Atkins diet may provide models to create an SCI-specific diet plan that allows for palatable and sufficient nourishment in the presence of caloric restriction.
To allow for comparisons, it is of utmost importance that these studies provide detailed descriptions of their participants, and that dietary recalls are standardized to ensure accurate reporting of energy intake. Finally, in the authors’ opinion and given the degree of article heterogeneity, there are insufficient data to establish evidence-based nutritional recommendations for individuals with chronic SCI. Additional research is crucial to improve our understanding of how dietary habits sustained in chronic SCI relate to the drastic changes in body composition and cardiometabolic profiles seen in this population [4].
Conclusion
The current review aimed to quantitatively summarize results from many articles and compare these results to current USDA 2015–2020 dietary guidelines for Americans. The results presented in this review demonstrate greater energy intake relative to energy needs in individuals with chronic SCI, as well as an imbalance in the intake of fiber and micronutrients compared to the AB population. However, the USDA 2015–2020 dietary guidelines may not necessarily reflect the needs of those living with SCI, given the anatomical and physiological changes that occur following the injury. Future research examining nutritional health status relative to body composition and energy expenditure is needed in order to establish evidence-based, SCI-specific dietary guidelines.
Change history
11 February 2019
The authors noted that there were two typographical errors in Table 2. Under the ‘Tetraplegia’ group of ‘Gorgey et al. [55]’ the ‘RMR’ value was originally given as ‘14,101 ± 10’. This has now been corrected to ‘1411 ± 10’. Under the ‘Tetra’ group of ‘Sabour et al. [22]’ the ‘Energy intake’ was originally given as ‘20,123 ± 681’. This has now been corrected to ‘2013 ± 681’. This has been corrected in both the PDF and HTML versions of the Article.
References
Farkas GJ, Gater DR. Neurogenic obesity and systemic inflammation following spinal cord injury: a review. J Spinal Cord Med. 2018;41:378–87.
Gater DR. Obesity after spinal cord injury. Phys Med Rehabil Clin N Am. 2007;18:333–51.
Devivo M. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Gater DR, Farkas GJ, Berg AS, Castillo C. Prevalence of metabolic syndrome in veterans with spinal cord injury. J Spinal Cord Med 2018:1–8.
Nash MS, Mendez AJ. A guideline-driven assessment of need for cardiovascular disease risk intervention in persons with chronic paraplegia. Arch Phys Med Rehabil. 2007;88:751–7.
Bigford G, Nash MS. Nutritional health considerations for persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23:188–206.
Academy of Nutrition and Dietetics. Spinal Cord Injury (SCI) Guidelines Chicago, Illinois. 2009. https://andeal.org/topic.cfm?menu=5292&pcat=3487&cat=5448.
Khalil RE, Gorgey AS, Janisko M, Dolbow DR, Moore JR, Gater DR. The role of nutrition in health status after spinal cord injury. Aging Dis. 2012;4:14–22.
Barber D, Foster D, Rogers S. The importance of nutrition in the care of persons with spinal cord injury. J Spinal Cord Med. 2003;26:122–3.
Dionyssiotis Y. Malnutrition in spinal cord injury: more than nutritional deficiency. J Clin Med Res. 2012;4:227–36.
Lieberman J, Goff D Jr., Hammond F, Schreiner P, Norton HJ, Dulin M, et al. Dietary intake and adherence to the 2010 Dietary Guidelines for Americans among individuals with chronic spinal cord injury: a pilot study. J Spinal Cord Med. 2014;37:751–7.
Groah SL, Nash MS, Ljungberg IH, Libin A, Hamm LF, Ward E, et al. Nutrient intake and body habitus after spinal cord injury: an analysis by sex and level of injury. J Spinal Cord Med. 2009;32:25–33.
Tomey KM, Chen DM, Wang X, Braunschweig CL. Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Arch Phys Med Rehabil. 2005;86:664–71.
Thibault-Halman G, Casha S, Singer S, Christie S. Acute management of nutritional demands after spinal cord injury. J Neurotrauma. 2011;28:1497–507.
Blissitt PA. Nutrition in acute spinal cord injury. Crit Care Nurs Clin North Am. 1990;2:375–84.
2015-2020 dietary guidelines for Americans. Washington, D.C.: U.S. Department of Health and Human Services and U.S. Department of Agriculture; 2015.
Institute of Medicine of the National Academy of Medicine. Finding what works in health care standards for systematic reviews; 2011. p. 1–4.
Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128:305–10.
Grossman RG, Frankowski RF, Burau KD, Toups EG, Crommett JW, Johnson MM, et al. Incidence and severity of acute complications after spinal cord injury. J Neurosurg Spine. 2012;17(1 Suppl):119–28.
American Dietetic Association. Spinal cord injury (SCI) evidenced-based nutrition practice guideline. Chicago, IL: American Dietetic Association; 2009.
Rodriguez DJ, Clevenger FW, Osler TM, Demarest GB, Fry DE. Obligatory negative nitrogen balance following spinal cord injury. JPEN J Parenter Enter Nutr. 1991;15:319–22.
Sabour H, Javidan AN, Vafa MR, Shidfar F, Nazari M, Saberi H, et al. Calorie and macronutrients intake in people with spinal cord injuries: an analysis by sex and injury-related variables. Nutrition. 2012;28:143–7.
Kmet L, Lee, RC, Cook, LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta, Canada: Alberta Heritage Foundation for Medical Research; 2004.
Altman DG, Bland JM. Standard deviations and standard errors. BMJ. 2005;331:903.
Nutrient Unit Conversion Factors: National Institutes of Health Office of Dietary Supplements and National Library of Medicine; 2017. https://www.dsld.nlm.nih.gov/dsld/unitconversion.jsp.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48.
Barboriak JJ, Rooney CB, El Ghatit AZ, Spuda K, Anderson AJ. Nutrition in spinal cord injury patients. J Am Paraplegia Soc. 1983;6:32–6.
Laven GT, Huang CT, DeVivo MJ, Stover SL, Kuhlemeier KV, Fine PR. Nutritional status during the acute stage of spinal cord injury. Arch Phys Med Rehabil. 1989;70:277–82.
Peiffer SC, Blust P, Leyson JF. Nutritional assessment of the spinal cord injured patient. J Am Diet Assoc. 1981;78:501–5.
Cameron KJ, Nyulasi IB, Collier GR, Brown DJ. Assessment of the effect of increased dietary fibre intake on bowel function in patients with spinal cord injury. Spinal Cord. 1996;34:277–83.
Moussavi RM, Ribas-Cardus F, Rintala DH, Rodriguez GP. Dietary and serum lipids in individuals with spinal cord injury living in the community. J Rehabil Res Dev. 2001;38:225–33.
Pellicane AJ, Millis SR, Zimmerman SE, Roth EJ. Calorie and protein intake in acute rehabilitation inpatients with traumatic spinal cord injury versus other diagnoses. Top Spinal Cord Inj Rehabil. 2013;19:229–35.
Aquilani R, Boschi F, Contardi A, Pistarini C, Achilli MP, Fizzotti G, et al. Energy expenditure and nutritional adequacy of rehabilitation paraplegics with asymptomatic bacteriuria and pressure sores. Spinal Cord. 2001;39:437–41.
VLRA ElizabeteAlexandredosSantos, Ramos Silvia, Frangella VeraSilvia. Analysis of the dietary habits and nutritional status of patients with spinal cord injury after nutritional intervention. Acta Fisiatr. 2014;21:121–1.
Grams L, Garrido G, Villacieros J, Ferro A. Marginal micronutrient intake in high-performance male wheelchair basketball players: a dietary evaluation and the effects of nutritional advice. PLoS ONE. 2016;11:e0157931.
Gerrish HR, Broad E, Lacroix M, Ogan D, Pritchett RC, Pritchett K. Nutrient intake of elite canadian and american athletes with spinal cord injury. Int J Exerc Sci. 2017;10:1018–28.
Wyse DM, Pattee CJ. Diet and metabolic alterations in paraplegia. Can Med Assoc J. 1954;71:235–8.
Pritchett K, Pritchett R, Ogan D, Bishop P, Broad E, LaCroix M. 25(OH)D status of elite athletes with spinal cord injury relative to lifestyle factors. Nutrients. 2016;8:6.
Ferro A, Garrido G, Villacieros J, Perez J, Grams L. Nutritional habits and performance in male elite wheelchair basketball players during a precompetitive period. Adapt Phys Act Q Apaq. 2017;34:295–310.
Knight KH, Buchholz AC, Martin Ginis KA, Goy RE. Leisure-time physical activity and diet quality are not associated in people with chronic spinal cord injury. Spinal Cord. 2011;49:381–5.
Sabour H, Larijani B, Vafa MR, Hadian MR, Heshmat R, Meybodi HA, et al. The effects of n-3 fatty acids on inflammatory cytokines in osteoporotic spinal cord injured patients: a randomized clinical trial. J Res Med Sci. 2012;17:322–7.
Sabour H, Soltani Z, Latifi S, Javidan AN. Dietary pattern as identified by factorial analysis and its association with lipid profile and fasting plasma glucose among Iranian individuals with spinal cord injury. J Spinal Cord Med. 2016;39:433–42.
Sabour H, Norouzi-Javidan A, Soltani Z, Mousavifar SA, Latifi S, Emami-Razavi SH, et al. The correlation between dietary fat intake and blood pressure among people with spinal cord injury. Iran J Neurol. 2016;15:121–7.
Sabour H, Nazari M, Latifi S, Soltani Z, Shakeri H, Larijani B, et al. The relationship between dietary Intakes of amino acids and bone mineral density among individuals with spinal cord injury. Oman Med J. 2016;31:22–8.
Gorgey AS, Mather KJ, Cupp HR, Gater DR. Effects of resistance training on adiposity and metabolism after spinal cord injury. Med Sci Sports Exerc. 2012;44:165–74.
Nightingale TE, Williams S, Thompson D, Bilzon JLJ. Energy balance components in persons with paraplegia: daily variation and appropriate measurement duration. Int J Behav Nutr Phys Act. 2017;14:132.
Levine AM, Nash MS, Green BA, Shea JD, Aronica MJ. An examination of dietary intakes and nutritional status of chronic healthy spinal cord injured individuals. Paraplegia. 1992;30:880–9.
Doubelt I, de Zepetnek JT, MacDonald MJ, Atkinson SA. Influences of nutrition and adiposity on bone mineral density in individuals with chronic spinal cord injury: a cross-sectional, observational study. Bone Rep. 2015;2:26–31.
Walters JL, Buchholz AC, Martin Ginis KA. Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord. 2009;47:318–22.
Krempien JL, Barr SI. Risk of nutrient inadequacies in elite Canadian athletes with spinal cord injury. Int J Sport Nutr Exerc Metab. 2011;21:417–25.
Javidan AN, Sabour H, Latifi S, Vafa M, Shidfar F, Khazaeipour Z, et al. Calcium and vitamin D plasma concentration and nutritional intake status in patients with chronic spinal cord injury: a referral center report. J Res Med Sci. 2014;19:881–4.
Perret C, Stoffel-Kurt N. Comparison of nutritional intake between individuals with acute and chronic spinal cord injury. J Spinal Cord Med. 2011;34:569–75.
Beal C, Gorgey A, Moore P, Wong N, Adler RA, Gater D. Higher dietary intake of vitamin D may influence total cholesterol and carbohydrate profile independent of body composition in men with chronic spinal cord injury. J Spinal Cord Med. 2018;41:459–70.
Gorgey AS, Caudill C, Sistrun S, Khalil RE, Gill R, Castillo T, et al. Frequency of dietary recalls, nutritional assessment, and body composition ssessment in men with chronic spinal cord injury. Arch Phys Med Rehabil. 2015;96:1646–53.
Lee BY, Agarwal N, Corcoran L, Thoden WR, Del Guercio LR. Assessment of nutritional and metabolic status of paraplegics. J Rehabil Res Dev. 1985;22:11–7.
Nash MS, Cowan RE, Kressler J. Evidence-based and heuristic approaches for customization of care in cardiometabolic syndrome after spinal cord injury. J Spinal Cord Med. 2012;35:278–92.
Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371–8.
Bauman WA, Spungen AM, Wang J, Pierson RN. The relationship between energy expenditure and lean tissue in monozygotic twins discordant for spinal cord injury. J Rehabil Res Dev. 2004;41:1–8.
Monroe MB, Tataranni PA, Pratley R, Manore MM, Skinner JS, Ravussin E. Lower daily energy expenditure as measured by a respiratory chamber in subjects with spinal cord injury compared with control subjects. Am J Clin Nutr. 1998;68:1223–7.
Johnstone AM, Murison SD, Duncan JS, Rance KA, Speakman JR. Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am J Clin Nutr. 2005;82:941–8.
Arciero PJ, Goran MI, Poehlman ET. Resting metabolic rate is lower in women than in men. J Appl Physiol. 1993;75:2514–20.
Haugen HA, Melanson EL, Tran ZV, Kearney JT, Hill JO. Variability of measured resting metabolic rate. Am J Clin Nutr. 2003;78:1141–5.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR. Effects of spinal cord injury on body composition and metabolic profile -part I. J Spinal Cord Med. 2014;37:693–702.
Gorgey AS, Farkas GJ, Dolbow DR, Khalil RE, Gater DR. Gender dimorphism in central adiposity may explain metabolic dysfunction after spinal cord injury. PM & R. 2017;10:338–48.
[No authors listed]. Clinical practice guidelines: neurogenic bowel management in adults with spinal cord injury. Spinal Cord Medicine Consortium. J Spinal Cord Med. 1998;21:248–93.
Pryor J, Fisher M, Middleton, J. Management of the neurogenic bowel for Adults with spinal cord injuries. ACI NSW Agency for Clinical Innovation; 2013. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0019/155215/Management-Neurogenic-Bowel.pdf.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Farkas GJ, Gorgey AS, Dolbow DR, Berg AS, Gater DR. Sex dimorphism in the distribution of adipose tissue and its influence on proinflammatory adipokines and cardiometabolic profiles in motor complete spinal cord injury. J Spinal Cord Med. 2018:1–15.
Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:749–56.
Bauman WA, Spungen AM. Body composition changes and anabolic hormone considerations with advancing age and in persons with spinal cord injury. Wounds . 2001;13:22D–31D.
Bauman WA, Spungen AM, Adkins RH, Kemp BJ. Metabolic and endocrine changes in persons aging with spinal cord injury. Assist Technol. 1999;11:88–96.
Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Dolbow JD, Dolbow DR, Gorgey AS, Adler RA, Gater DR. The effects of aging and electrical stimulation exercise on bone after spinal cord injury. Aging Dis. 2013;4:141–53.
Garrison A, Clifford K, Gleason SF, Tun CG, Brown R, Garshick E. Alcohol use associated with cervical spinal cord injury. J Spinal Cord Med. 2004;27:111–5.
Frisbie JH, Tun CG. Drinking and spinal cord injury. J Am Paraplegia Soc. 1984;7:71–3.
Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: risk factors and correlates. Arch Phys Med Rehabil. 2004;85:1837–47.
Kressler J, Cowan RE, Bigford GE, Nash MS. Reducing cardiometabolic disease in spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25:573–604.
Cox SA, Weiss SM, Posuniak EA, Worthington P, Prioleau M, Heffley G. Energy expenditure after spinal cord injury: an evaluation of stable rehabilitating patients. J Trauma. 1985;25:419–23.
Gater DR, Farkas GJ. Alterations in body composition after SCI and the mitigating role of exercise. In: Taylor J, editor. The physiology of exercise in spinal cord injury. Physiology in health and disease. Boston, MA: Springer; 2016. p. 175–98.
Morgan K. Socioeconomic factors affecting dietary status: an appraisal. Am J Agric Econ. 1986;68:1240–6.
Gorgey AS, Shepherd C. Skeletal muscle hypertrophy and decreased intramuscular fat after unilateral resistance training in spinal cord injury: case report. J Spinal Cord Med. 2010;33:90–5.
Gorgey AS, Harnish CR, Daniels JA, Dolbow DR, Keeley A, Moore J, et al. A report of anticipated benefits of functional electrical stimulation after spinal cord injury. J Spinal Cord Med. 2012;35:107–12.
Author information
Authors and Affiliations
Contributions
GJF devised the study idea and was responsible for designing the review protocol, writing the initial manuscript, conducting the search, screening potentially eligible studies, extracting data, performing quality ratings of articles, and interpreting results. MAP was responsible for conducting the search, screening potentially eligible studies, extracting data, performing quality ratings of articles, and assisting with manuscript editing. GJF and ASB performed the data analyses. DRG mediated potentially eligible studies, provided feedback on the manuscript, and contributed to the study idea. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of ethics
We ensure this research was carried out with the highest ethical standards.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Farkas, G.J., Pitot, M.A., Berg, A.S. et al. Nutritional status in chronic spinal cord injury: a systematic review and meta-analysis. Spinal Cord 57, 3–17 (2019). https://doi.org/10.1038/s41393-018-0218-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0218-4
This article is cited by
-
Correlates of metabolic syndrome in people with chronic spinal cord injury
Journal of Endocrinological Investigation (2024)
-
Impact of malnutrition on mortality and neurological recovery of older patients with spinal cord injury
Scientific Reports (2024)
-
Neurological recovery rate and predictive factors of incomplete AIS grade C spinal cord injury in the older aged population
Spinal Cord (2024)
-
Metal-organic framework materials promote neural differentiation of dental pulp stem cells in spinal cord injury
Journal of Nanobiotechnology (2023)
-
Mapping of Dietary Interventions Beneficial in the Prevention of Secondary Health Conditions in Spinal Cord Injured Population: A Systematic Review
The Journal of nutrition, health and aging (2023)