Abstract
Study design
Replication of previously developed prognostic model.
Objectives
In motor complete injuries at admission to rehabilitation, perform; (1) replication analyses of the relationships between ISNCSCI motor level and motor scores and SCIM and (2) novel analyses to determine if age and/or sex moderate relationship between neurological impairment and function.
Setting
Admission to initial inpatient rehabilitation in the United States.
Methods
Post-Hoc analyses of data collected as part of a separate study. Replication analyses: (1) Pearson’s correlation assessed relationship strength between neurologic impairment and function. (2) Multiple linear regression assessed if center or age influenced functional outcome. Novel analyses: (1) Moderated multiple regression assessed if age and/or sex moderated the lesion level-function relationship.
Results
Of the 406 datasets, 161 were motor complete injuries, and included in the analyses. Median time post injury at admission to rehabilitation was 19 days. Our replication analyses confirmed the neurologic and functional value of each spinal segment reported by the EM-SCI group (all p ≤ 0.018). We failed to confirm their reported age effect (p = 0.05) and non-effect of center (p = 0.037). Our novel analyses indicated that age coded as above/below 50 moderated the relationship between neurologic impairment and function (p = 0.038) in cervical injuries only, but that age coded as above/below 35 (all p ≥ 0.510) and sex (all p ≥ 0.465) did not.
Conclusions
The neurological and functional value of each segment is consistent across very different healthcare settings in early and late sub-acute stages and minimally impacted by age and sex. Differences related to centers and age may confound efficacy trials.
Sponsorship
The Miami Project to Cure Paralysis; The Craig H. Neilsen Foundation (83492)
Similar content being viewed by others
Introduction
Clinical trials testing acute neuroprotective and/or neurorecovery therapies for people with spinal cord injury (SCI) have used components of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) as primary outcomes [1,2,3,4,5]. The ISNCSCI measures neurologic impairment [6, 7], not functional status. Functional status improvements are likely to be necessary to gain approval from regulatory bodies and people living with SCI. Therefore, it would be helpful to better understand the relationship between measures of neurologic impairment and function.
The ISNCSCI is the international gold standard for neurologic impairment evaluation. The Spinal Cord Independence Measure (SCIM) is an SCI-specific functional measure that is valid and sensitive to change [8,9,10,11]. Among persons with motor-sensory complete cervical injuries, ISNCSCI upper extremity motor score is positively related to SCIM total score and self-care subscale [12]. In a European study, the value of each cervical segment, based on regression coefficients, among persons with motor-complete cervical injuries was calculated to be nine ISNCSCI upper extremity motor points and four SCIMmot points [13]. For persons with thoracic injury, the relationship between these assessments was weak to non-existent. The ISNCSCI does not measure thoracic region motor impairment.
Defining the value of each segment in the acute and subacute stages may allow researchers to understand the relative contributions of spontaneous neurologic recovery and/or rehabilitation to functional gains measured at chronic time points. Up to 70% of individuals with cervical motor-complete injuries recover at least one motor level during the first year post-injury [14], but recovery of one motor level does not always confer a significant functional gain [12]. The functional value of each segment is likely to be different before rehabilitation compared to after, as SCIM III scores change during this time period [15]. Since rehabilitation paradigms and durations are vastly different in Europe and the United States (US), it is important to understand if the value of each segment is similar in a US population despite these differences in rehabilitation.
Neurological and functional recovery may also be influenced by age at time of injury and sex [16,17,18]. Two studies report that age negatively affects both neurologic and functional recovery [19, 20] whereas another study indicated that age positively influenced neurologic recovery, but negatively influenced functional outcome [21]. Data from the US Spinal Cord Model Systems database has produced conflicting results regarding sex, with one study reporting a non-effect of sex on neurological impairment or function at rehabilitation admission and discharge [22], while another reported a sex effect for function but not neurological impairment [23]. A better understanding of if and how these factors influence neurological and functional value of each segment will facilitate more accurate sample size estimates for future clinical trials.
A large multi-center trial conducted in the US demonstrated that the SCIM III is a valid and reliable measure of functional outcome in the acute inpatient rehabilitation setting [11]. As a result, there is a large (n = 406), prospective database of ISNCSCI and SCIM III scores from patients at the time of their initial inpatient rehabilitation admission. This database allows further analyses of the relationships between neurological and functional outcomes and potential effect of age and/or sex. Using this database generated in the US healthcare system, we sought to replicate Van Hedel and Curt’s European work [13] that established values for each spinal cord segment. Van Hedel and Curt [13] targeted a small cohort (n = 93) at six months’ post-injury, when initial inpatient rehabilitation had already been completed or was still ongoing. Our cohort is larger (n = 161) and consists of individuals evaluated at their initial admissions to inpatient rehabilitation.
Our first specific goal was to replicate their analyses of the relationships between ISNCSCI single motor level and motor scores and SCIM at admission to rehabilitation. Our second goal was to perform novel analyses to enhance our understanding of how age and/or sex may moderate the relationship between neurological impairment and functional outcome early post-injury.
Methods
No participants were enrolled in this study, which consisted entirely of a retrospective analysis of a de-identified database of prospectively collected data.
Neurological Impairment
Motor level was determined in accordance with ISNCSCI standards as the most caudal level with bilateral normal function. Per van Hedel and Curt [13], we used motor level to represent lesion level for cervical injuries and sensory level to represent lesion level for thoracic injuries. Unlike their cohort, ours included both traumatic and non-traumatic injuries.
Function
Function was assessed by quantifying level of independence using the SCIM-III. Dependent variables include the SCIM total score (SCIM tot); the SCIM motor score (SCIMmot), defined as the sum of the self-care and mobility domains; and the SCIM self-care domain score (SCIMsc). The SCIMtot and SCIMmot were also reported by van Hedel and Curt [13].
Data Reduction
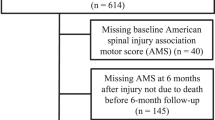
The database included datasets on 406 individuals. Per van Hedel and Curt [13], motor incompletes, lumbar lesions, and sacral lesions were excluded (n = 214, 52.7%). Four others were excluded due to missing ISNCSCI data. Motor incompletes were defined in accordance with ISNCSCI grading standards at the time of initial data collection [6]. After exclusions, n = 161 individuals with motor complete (AIS A or B) cervical or thoracic injuries were available for analysis (Fig. 1).
Flow chart of how the complete dataset was reduced for analyses. *Criteria matches criteria explicitly stated in van Hedel and Curt [13]. **Persons with injuries at or above T11 with any lower extremity motor function and persons with T12 injuries with more than 10 lower extremity motor points were excluded because that represented partial motor preservation more than two levels below the level of injury
Replication data analysis
We replicated van Hedel and Curt’s analyses [13] using their published analytic approach: 1) Influence of lesion level on function; 2) Influence of center and lesion level on function; and 3) Influence of age and lesion level on function. For all analyses, lesion levels were consecutively numbered (C1–4 as 4, C5 as 5, C6 as 6, C7 as 7, C8 as 8, T1 as 9, etc… with T12 as 20), with separate analyses performed for tetraplegia (C1-T1) and paraplegia (T2-T12).
For the first replication analysis (lesion level only), Pearson’s correlation assessed the strength of the relationship between 1) lesion level and each SCIM domain (self-care, respiration & sphincter management, mobility) and 2) between ISNCSCI motor and SCIMtot, SCIMmot, and SCIMsc. In addition, separate linear regressions modeled ISNCSCI total motor score, SCIMtot, SCIMmot, and SCIMsc from lesion level. We included SCIMsc in these analyses, although van Hedel and Curt [13] did not.
For the second replication analysis (center and lesion level), multiple linear regression was used to assess if differences existed between centers, with separate models run for tetraplegia and paraplegia (backward model, probability for entry = 0.05, probability for removal = 0.10). Van Hedel and Curt used three center groups. The two high accrual centers (centers 1 (N = 32) and 3 (N = 26)) were assigned unique codes while the lower accruing centers were collapsed as the third center (N = 40 total). The low accrual centers each enrolled between N = 4 and N = 11 individuals. Following the approach used by van Hedel and Curt [13], we also created three center groups based on accrual. We coded centers as high (coded as +1, N ≥ 31), medium (coded as 0, 11 ≤ N ≤ 30), and low accrual (coded as −1, N < 10) based on total number of participants enrolled (i.e., including persons excluded from this analysis).
For the third replication analysis (age and lesion level), multiple linear regression was used to assess if age at time of injury additionally influenced functional outcome (SCIMtot) (backward model, probability for entry = 0.05, probability for removal = 0.10). Age was input as a continuous variable.
Novel data analysis
We used moderated multiple regression to determine whether age or sex moderated the relationship between lesion level and functional outcome (ISNCSCI motor and SCIMtot) and also whether sex further moderated the age moderation effect [24]. Separate regressions were conducted for each moderator (age, sex, sex × age) and each injury level (tetraplegia and paraplegia). Lesion level was coded as described above for replication analysis. Sex was coded as M = 0 (reference category) and F = 1. Age was first coded as above (1) or below (0) the median age (35 years) of our sample. In addition, due to the increasing number of injuries occurring among persons over age 50 [25,26,27], we then coded age as above (1) or below (0) 50 years. A moderation effect was considered present when the interaction term was significant (i.e., age × lesion level, sex × lesion level, or sex × age × lesion level). For all analyses, significance was set a priori at α = 0.05.
We certify that all applicable institutional and governmental regulations concerning the ethical use of humans were followed during the course of this research. A copy of the dataset used for this analysis can be obtained by contacting the corresponding author.
Results
Participants
One hundred sixty-one individuals with motor complete SCI (76% AIS A) were analyzed (Table 1). Most injuries were of a traumatic etiology (81%) and slightly fewer than half were cervical injuries (45%). Participants were evaluated at initial admission to inpatient rehabilitation, which occurred a median of 19 days post injury (Interquartile range = 10–34).
Replication analysis: influence of lesion level on neurologic and functional outcome
At admission to rehabilitation, lesion level was positively associated with all SCIM subdomains (all p < 0.00) for the entire sample and the cervical subset (Table 2). For persons with thoracic injuries, lesion level was associated only with respiration and sphincter management (p = 0.037, Table 2). All significant associations identified by van Hedel and Curt [13] were present in our analysis. However, our effect sizes [28] were generally stronger [13].
Among cervical but not thoracic injuries, there was a positive association between ISNCSCI motor score and SCIMtot and SCIMmot (Table 2), matching their results. Both studies indicate a strong relationship between ISNCSCI motor score and SCIM scores in cervical but not thoracic injuries [13].
For individuals with cervical injuries, lesion level was a significant predictor of all functional outcomes, but for thoracic injuries, lesion level predicted only ISNCSCI scores (Table 3 and Fig. 2). This matches the results reported by van Hedel and Curt [13]. Among cervical injuries, the value of each cervical segment (b1 coefficient) for ISNCSCI motor score, SCIMtot, SCIMmot, and SCIMsc was 8.89, 3.87, 2.70, and 1.78 pts, respectively. These values fall within the 95% CI reported by van Hedel and Curt [13] (Fig. 3). Among thoracic injuries, the value of each thoracic segment for ISNCSCI motor score was 0.07 (p = 0.018), with no effect present for SCIMtot, SCIMmot, and SCIMsc (all p > 0.07). This also matches results reported by van Hedel and Curt [13].
Mean and 95% confidence interval of the mean of the neurologic and functional value of each spinal segment for the current analyses (light gray) and published analyses (dark gray). For the current analyses the numerical values are located in Table 3. Only significant results are plotted
Replication analysis: Influence of center and lesion level on neurologic and functional outcomes
For both injury groups, center did not influence ISNCSCI motor score (Supplemental Table 1), confirming van Hedel and Curt’s findings [13].
However, for thoracic injuries only, center did influence function (Supplemental Table 1). At admission to rehabilitation, for each thoracic lesion level, SCIMtot scores averaged 5.40 points greater at high accrual versus medium accrual centers (p = < 0.05, Supplemental Fig. 1). The lack of a center effect among cervical injuries matches van Hedel and Curt’s results [13] while the presence of a center effect among thoracic injuries contradicts their findings.
Replication analysis: influence of age and lesion level on functional outcome
For both cervical and thoracic injuries, age did not influence function (Supplemental Table 2). Our results are in contrast to van Hedel and Curt [13], who found that age significantly influenced function in both cervical and thoracic injuries, with function decreasing as age increased.
Novel analysis: does age moderate the relationship between lesion level and function?
At admission to rehabilitation, among motor complete cervical and thoracic injuries, the strength of the lesion-function relationship is not different based on age above or below 35 years (both age × lesion level β p ≥ 0.510, Table 4). This means the functional value of each cervical or thoracic segment is approximately the same for persons younger or older than 35.
However, when we code the sample as younger or older than 50, for cervical but not thoracic injuries, the relationship between lesion level and function is stronger for persons age 50 and older compared to persons under 50 (Table 4, age × lesion term). Using the regression coefficients, the estimated SCIMtot value of each cervical segment is 3.15 points for persons under age 50 and 4.15 points for persons age 50 and older.
For all age moderation analyses, the age coefficient was not statistically significant (Table 4, all age β p ≥ 0.11). This suggests that for each lesion level, there was no measureable difference in function between persons younger or older than the age cutoff (35 or 50). However, there may be a clinically relevant age effect. For each cervical segment rostral to T1, the estimated function for persons ≥50 is at least 2.68 points lower than persons ≤49 (Supplemental Fig. 2, gray shaded area = 2.68 points). This 2.68 is the 95% CI lower limit for the estimated SCIMtot value of a cervical segment.
Novel analysis: does sex moderate the relationship between lesion level and function?
Sex does not moderate the relationship between lesion level and functional outcome for cervical (sex × lesion level β = −1.27, p = 0.465) or thoracic injuries (sex × lesion level β = −0.116, p = 0.965). In addition, there was no statistically significant difference in function between men and women for cervical (β = 3.90, p = 0.71) or thoracic injuries (β = −0.258, p = 0.99).
Novel analysis: is the moderating effect of age further moderated by sex?
The moderating effect of age on the lesion level-function relationship is not further moderated by sex. This finding holds true for both age cut offs and both injury groups. For the 35 year cutoff, for cervical injuries, sex × age × lesion level resulted in β = 1.809 and p = 0.872, and for thoracic injuries, sex × age × lesion level resulted in β = 1.71 and p = 0.470. For the 50 year cutoff, for cervical injuries, sex × age × lesion level resulted in β = 0.292 and p = 0.763, and for thoracic injuries, sex × age × lesion level resulted in β = −0.188 and p = 0.445.
Discussion
Using our database, we found similar results as van Hedel and Curt’s [13] findings regarding the value of each cervical and thoracic segment and the association between ASIA motor level and SCIM function. Our finding of similar results in a very different cohort (19 days versus 6 months post injury) suggests these relationships and the value of each segment are robust and can reliably inform clinical trial design. Our higher correlation coefficients, higher R2, and smaller confidence intervals compared to van Hedel and Curt [13] suggest that the relationship between neurological impairment and function is stronger before rehabilitation and before compensation strategies are adopted.
Existing literature indicates that at matched levels of motor impairment/preservation, ‘function’ is lower in older individuals [19,20,21]. Van Hedel and Curt’s [13] results supports this proposition using a cohort that was six months’ post injury. We cannot confirm their results. Our ‘non-finding’ of a statistical age effect could be due to our cohort’s sub-acute, pre-rehabilitation state. However, the EM-SCI study group reported age negatively influenced function at one-month post injury, which we presume was pre-rehabilitation [21]. The EM-SCI analysis included motor incomplete injuries, which could explain the divergent results. We concur with their suggestion that the negative impact of age on function represents an inability of older individuals to develop compensation strategies [21].
To expand our understanding of age and sex effects, we assessed whether the value of each segment depended on a person’s age or sex. Restated, our question was, if subsets of both groups (age and sex) ‘recover’ the same number of neurological levels, can we expect these subsets to ‘recover’ the same amount of function? Our results suggest that for cervical and thoracic injuries, the functional value of each segment is similar for men and women and for persons above/below age 35. Each of these groups are estimated to have a similar degree of functional benefit from each segment recovered. However, for individuals with motor complete cervical injures, the estimated functional value of each segment is greater for people age 50 or older versus those under age 50. This suggests that “older” persons may be better able to translate neurological recovery into functional gains. This directly contrasts with multiple reports [21, 29] that older adults are less able to [30,31,32,33] translate neurological recovery to functional gains. This conflict may be due to underlying study sample differences. Although our analysis was based on motor complete injuries (AIS A and B), presence of a motor complete injury does not preclude a substantial zone of partial preservation [34] which could contribute to greater function or functional gains. Future work on the moderating effect of age on the lesion-function relationship in motor complete injuries should address the potential influence of the zone of partial preservation.
Last, but not least, our replication of van Hedel and Curt’s analysis of the potential impact of ‘center’ on neurological and functional outcomes produced mixed results. We confirmed their finding that center did not affect neurological outcome. However, we were unable to confirm that center did not affect functional outcome. Our results indicate that persons with thoracic injuries admitted to high accrual centers had greater function than those admitted to medium or low accrual centers. This could be due to many factors, such as SCIM administration differences, a practice effect of administering the SCIM more frequently, or that larger centers may receive a greater number of higher functioning individuals.
Clinical trial design age, sex, and center considerations
Half of all Phase II and III drug trials fail due to an inability to demonstrate efficacy [35]. Some efficacy threats can be mitigated with thoughtful trial design, but not all threats warrant equal consideration. We suggest that center and age effects may pose greater confounding threats than sex for efficacy trials among motor complete injuries. Sex has been inconsistently reported as having a negative impact on functional outcomes [22, 23]. On the other hand, there is robust evidence that older individuals have poorer functional outcomes than younger individuals [19,20,21]. Our results add to this evidence base by suggesting that the functional value of each segment is greater for persons over age 50. Collectively, these findings suggest that larger sample sizes may be needed to establish efficacy in persons aged 50 and older. Potential center effects have been minimally addressed by previous recommendations for SCI trials [36, 37]. Some center effects, such as those attributable to staff competency, may be mitigated by implementing stringent training procedures and frequently assessing tester reliability. Others, such as patient selection bias, may require thoughtful selection of participating sites to achieve the desired composition. Clinical trial designs could be improved if relevant effect sizes for potential confounders were established.
Limitations
Generalizability, interpretation, and application of our work must be balanced against its limitations. With regards to ‘center’ effects or non-effects, readers should be aware that both our and Van Hedel and Curt’s center ‘coding’ was arbitrary. However, inter-center variance represents real threats to establishing efficacy [38, 39]. Our dataset included traumatic and non-traumatic injuries. Although all had motor complete injuries, it is possible that the observed results could differ if the sub-groups were analyzed separately. However, given the parallels with van Hedel and Curt’s results, any effect is likely negligible. Our sample was also very early post-injury and it is probable that the relationships and outcomes will present differently in a more chronically injured cohort. Finally, when performing the replication analyses, we noted that some of the regression models poorly fit the data. Inspection of the residuals normal probability plots indicated non-normal distributions, which can result in unstable coefficient estimates. Van Hedel and Curt did not report model fit information, thus we cannot know if their regression models fit the data well.
Conclusions
This study provides greater understanding of the neurologic and functional value of each spinal segment and the influence of age and sex upon these values at the time of initial admission to inpatient rehabilitation in the United States. With respect to the scientific knowledge base, our results paired with van Hedel and Curt [13] suggest (a) the neurological and functional value of each segment is consistent across very different healthcare settings and two distinct time points post injury and (b) that these values are minimally impacted by age and sex. With respect to clinical trial design, our results suggest (a) differences between study centers could confound the ability to detect functional changes in thoracic injuries and (b) the effect of age on the functional value of each segment could confound the ability to detect functional changes in cervical injuries.
References
Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen® Study Group. The Sygen® multicenter acute spinal cord injury study. Spine. 2001;26:S87–98.
Fehlings MG, Theodore N, Harrop J, Maurais G, Kuntz C, Shaffrey CI, et al. A phase I/IIa trial of a recombinant rho protein antagonist in acute spinal cord injury. J Neurotrauma. 2011;28:787–96.
Lammertse DP, Jones LAT, Charlifue SB, Kirshblum SC, Apple DF, Ragnarsson KT, et al. Autologous incubated macrophage therapy in acute, complete spinal cord injury: results of the phase 2 randomized controlled multicenter trial. Spinal Cord. 2012;50:661–71.
Casha S, Zygun D, McGowan MD, Bains I, Yong VW, Hurlbert RJ. Results of a phase II placebo-controlled randomized trial of minocycline in acute spinal cord injury. Brain. 2012;135:1224–36.
Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS ONE. 2012;7:e32037 https://doi.org/10.1371/journal.pone.0032037
Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. 1997;35:226–74.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spin Cord Med. 2011;34:547–54.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM – spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K, et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2011;49:880–5.
Kramer JL, Lammertse DP, Schubert M, Curt A, Steeves JD. Relationship between motor recovery and independence after sensorimotor-complete cervical spinal cord injury. Neurorehabil Neural Repair. 2012;26:1064–71.
Van Hedel HJA, Curt A. Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotrauma. 2006;23:161–1631.
Steeves JD, Kramer JK, Fawcett JW, Cragg J, Lammertse DP, Blight AR, et al. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal Cord. 2011;49:257–65.
Ackerman P, Morrison SA, McDowell S, Vazquez L. Using the Spinal Cord Independence Measure III to measure functional recovery in a post-acute spinal cord injury program. Spinal Cord. 2010;48:380–7.
Krassioukov AV, Furlan JC, Fehlings MG. Medical co-morbidities, secondary complications, and mortality in elderly with acute spinal cord injury. J Neurotrauma. 2003;20:391–9.
Furlan JC, Kattail D, Fehlings MG. The impact of co-morbidities on age-related differences in mortality after acute traumatic spinal cord injury. J Neurotrauma. 2009;26:1361–7.
Gulati A, Yeo CJ, Cooney AD, McLean AN, Fraser MH, Allan DB. Functional outcome and discharge destination in elderly patients with spinal cord injuries. Spinal Cord. 2011;49:215–8.
McKinley W, Cifu D, Seel R, Huang M, Kreutzer J, Drake D, et al. Age-related outcomes in persons with spinal cord injury: a summary paper. NeuroRehabilitation. 2003;18:83–90.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M. Effects on age on spinal cord lesion patients’ rehabilitation. Spinal Cord. 2003;41:457–64.
Jakob W, Wirz M, van Hedel HJ, Dietz V, EM-SCI Study Group.. Difficulty of elderly SCI subjects to translate motor recovery--“body function”--into daily living activities. J Neurotrauma. 2009;26:2037–44.
Greenwald BD, Seel RT, Cifu DX, Shah AN. Gender-related differences in acute rehabilitation lengths of stay, charges, and functional outcomes for a matched sample with spinal cord injury: a multicenter investigation. Arch Phys Med Rehabil. 2001;82:1181–7.
Sipski ML, Jackson AB, Gomez-Marin O, Estores I, Stein A. Effects of gender on neurologic and functional recovery after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1826–36.
Aiken LS, West SG, (eds.). Multiple regression: testing and interpreting interactions. Thousand Oaks, CA: Sage Publications; 1991.
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016;54:270–6.
Chen Y, He Y, DeVivo MJ. Demographics and Injury Profile of New Traumatic Spinal Cord Injuries in the United States, 1972-2014. Arch Phys Med Rehabil. 2016;97:1610–9.
Toda M, Nakatani E, Omae K, Fukushima M, Chin T. Age-specific characterization of spinal cord injuries over a 19-year period at a Japanese rehabilitation center. PLoS ONE. 2018; https://doi.org/10.1371/journal.pone.0195120
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Wirz M, Dietz V, EM-SCI Network. Recovery of sensorimotor function and activities of daily living after cervical spinal cord injury: the influence of age. J Neurotrauma. 2015;32:194–9.
Wilson JR, Davis AM, Kulkarni AV, Kiss A, Frankowski RF, Grossman RG, et al. Defining age-related differences in outcome after traumatic spinal cord injury: Analysis of a combined, multi-center dataset. Spine J. 2014;14:1192–8.
Sparrey CJ, Choo AM, Liu J, Tetzlaff W, Oxland TR. The distribution of tissue damage in the spinal cord is influenced by the contusion velocity. Spine. 2008;33:E812–819.
Wang H, Xiang L, Liu J, Zhou Y, Ou L. Gender differences in the clinical characteristics of traumatic spinal fractures among the elderly. Arch Gerontol Geriatr. 2014;59:657–64.
Daneshvar P, Roffey DM, Brikeet YA, Tsai EC, Bailey CS, Wai EK. Spinal cord injuries related to cervical spine fractures in elderly patients: factors affecting mortality. Spine J. 2013;13:862–6.
Marino RJ, Burns S, Graves DE, Leiby BE, Kirshblum S, Lammertse DP. Upper- and lower-extremity motor recovery after traumatic cervical spinal cord injury: an update from the national spinal cord injury database. Arch Phys Med Rehabil. 2011;92:369–75.
Thomas DW, Burns J, Audette J, Carroll A, Dow-Hygelund C, Hay M. Clinical development success rates 2006-2015. Biotechnology Innovation Organization (BIO) Industry Analysis. 2016. pp. 1–28.
Lammertse DL, Tuszynski MH, Steeves JD, Curt A, Fawcett JW, Rask C, et al. Guidelines for the conduct of clinical trials for spinal cor injury as developed by the ICCP panel: clinical trial design. Spinal Cord. 2007;45:232–42.
Fehlings MG, Kim KD, Aarabi B, Rizzo M, Bond LM, McKerracher L, et al. Rho inhibitor VX-210 in acute traumatic subaxial cervical spinal cord injury: design of the SPinal cord injury Rho INhibition investiGation (SPRING) clinical trial. J Neurotrauma. 2018;35:1049–56.
Localio AR, Berlin JA, Ten Have TR. Confounding due to cluster in multicenter studies–causes and cures. Health Serv Outcomes Res Methodol. 2002;3:195–210.
Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Int Med. 2001;135:112–23.
Acknowledgements
We acknowledge Carla Strohhofer’s substantial effort on cleaning and error checking the database and financial support from The Miami Project to Cure Paralysis and The Craig H. Neilsen Foundation (83492).
Funding
The Miami Project to Cure Paralysis and The Craig H. Neilsen Foundation (83492).
Authors’ contributions
REC conceptualized the manuscript; contributed to the selection of aims, selected and executed all statistical analyses, developed the tables and figures, and contributed to multiple drafts of the manuscript. KDA designed and executed the original study that resulted in the database; contributed to the selection of aims, and contributed to multiple drafts of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Cowan, R.E., Anderson, K.D. Replication and novel analysis of age and sex effects on the neurologic and functional value of each spinal segment in the US healthcare setting. Spinal Cord 57, 156–164 (2019). https://doi.org/10.1038/s41393-018-0206-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0206-8
This article is cited by
-
Functional independence in the Finnish spinal cord injury population
Spinal Cord (2022)