Abstract
Study design
Prospective cohort study.
Objectives
This prospective cohort study aims to evaluate the recovery of penetration/aspiration and functional feeding outcome in patients with acute TCSCI.
Setting
Tampere University Hospital, Tampere, Finland
Methods
Forty-six patients with TCSCI were enrolled. All the patients received speech therapeutic interventions based on their clinical needs and were examined with a videofluoroscopic swallowing study (VFSS) at enrollment. The incidence of VFSS-verified laryngeal penetration/aspiration according to Rosenbek’s Penetration-Aspiration Scale (PAS) served as the primary outcome. The secondary outcome was the level of functional oral intake (as per the Functional Oral Intake Scale; FOIS). Based on the PAS results, the patients were divided into two groups: (i) penetrator/aspirators (PAS score ≥3) and (ii) non-penetrator/aspirators (PAS score ≤2). Follow-up VFS studies were primarily conducted on the patients with penetration/aspiration in prior VFS studies. The follow-up VFS studies were scheduled on the basis of clinical demand.
Results
Of the 46 patients, 48% had penetration/aspiration in the first VFSS. The second VFSS was conducted on 20 patients, of whom 6 patients (30%) had penetration/aspiration. The third VFSS was conducted on 9 patients. Of these, only two (22%) patients were still penetrator/aspirators. The majority (n = 37, 88%) of the patients presented a total oral intake without restrictions at the time of the final follow-up. Only one patient (2%) was still tube-dependent with consistent oral intake.
Conclusion
Swallowing physiology in patients with TCSCI improved during the first months after injury, and the number of penetrator/aspirators decreased progressively.
Similar content being viewed by others
Introduction
Dysphagia is a relatively common secondary complication in patients with a cervical spinal cord injury (CSCI). In previous studies, the incidence of dysphagia in CSCI has varied from 16 to 80% [1,2,3,4,5,6,7,8,9,10,11], and the incidence of aspiration verified by VFSS or fiberoptic endoscopic evaluation of swallowing (FEES) varied between 6 and 41% [2,3,4, 6,7,8,9,10,11]. Studies focusing on CSCI have presented some risk factors for dysphagia, e.g., age [1, 7,8,9, 11], tracheostomy [1, 3,4,5,6,7,8,9,10,11], mechanical ventilation [1, 5, 9,10,11], the completeness of the spinal cord injury (SCI)[1, 4], the level of injury [1, 2, 4,5,6], and cervical surgery [1, 3]. By contrast, some studies found no association between dysphagia and age [2,3,4, 6], dysphagia and mechanical ventilation [8], dysphagia and the level or completeness of the injury [7, 8, 10], and dysphagia and cervical surgery [4,5,6,7,8, 11]. Longitudinal reports on the rate and extent of recovery from swallowing dysfunction in patients with TCSCI are limited [2,3,4, 6].
In this prospective study we aim to examine the temporal recovery of penetration/aspiration and functional feeding outcome in cohort of 46 patients with TCSCI. In addition, we report the summary of speech therapy interventions for the patients during the follow-up. Data for this study were collected as a part of routine multidisciplinary care at a university hospital that is focused on treating traumatic SCI patients. This current study is the third part of our research project that aims to improve knowledge on the incidence, risk factors, and recovery trajectory of laryngeal penetration/aspiration of with patients with TCSCI in Finland. In our first study with the same cohort of patients as used in this current study, we reported the incidence of aspiration with PAS scores 7–8 to be 33 % and the incidence of penetration with PAS scores 2–5 to be 41% [12]. In our second study we reported the following risk factors for predicting penetration-aspiration in patients with TCSCI: (i) necessity of bronchoscopies; (ii) a lower level of anterior cervical operation; (iii) coughing, throat clearing, and choking related to swallowing; and (iv) changes in voice quality related to swallowing [13]. For the purposes of the second study, the patient cohort comprised of 37 out of 46 patients with VFSS conducted in 28 days post-injury.
Methods
This study was performed with the approval of the Ethics Committee of Pirkanmaa Hospital District, Tampere, Finland. All patients provided written informed consent according to the Declaration of Helsinki. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Patients and demographic data
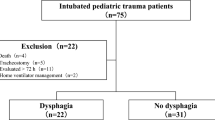
The study population consists of a prospective cohort of applicable patients with acute TCSCI admitted to the Tampere University Hospital from February 2013 to April 2015. In total, 94 consecutive patients were screened, and 46 (48.9%) patients were included in this study. The primary exclusion criteria included: (1) age <18 years; (2) respiratory arrest; (3) severe brain injury; (4) a prior medical condition causing dysphagia; (5) pregnancy; and (6) refusal to participate. Secondary reasons for exclusion were: (1) a low level of consciousness at enrollment; (2) discharge before recruitment; (3) a delay of 3 months or more between the injury and admission to the study hospital; and (4) a videofluoroscopic swallowing study (VFSS) not being performed. The study process is described in detail in our previous publication [12].
The following variables were recorded for all patients: gender; age at the time of injury; injury mechanism (as per the International Spinal Cord Injury Core Data Set [14]); length of stay (LOS) on the rehabilitation ward, a total number of speech therapy interventions during acute care and rehabilitation and time frames between the injury and swallowing evaluations. The International Standards for Neurological Classification of Spinal Cord Injury was used to evaluate and classify the neurological consequences of the spinal cord injury [15, 16]. The completeness of the injury was defined according to the American Spinal Injury Association Impairment Scale (AIS): AIS A = motor-sensory complete, AIS B = motor complete-sensory incomplete, or AIS C–D = motor-sensory incomplete.
VFSS
The first VFSS (Siemens Axiom Luminos DRF, Erlangen, Germany) was conducted on all 46 patients as soon as practically possible post-injury. Based on the Rosenbek’s Penetration-Aspiration Scale (PAS) results, the patients were divided into two groups: (i) penetrator/aspirators (PAS score ≥ 3) and (ii) non-penetrator/aspirators (PAS score ≤ 2). Scores of 1 and 2 are considered functionally normal [17,18,19]. The follow-up VFS studies were primarily conducted on patients with penetration/aspiration (PAS score ≥3) evident in the prior VFSS. Additionally, a follow-up VFSS was conducted on seven non-penetrator/aspirators (PAS score ≤2) based on clinical needs. The second, third, and fourth VFS studies were scheduled based on clinical needs. The VFSS protocol included 5 ml, 10 ml, and 20 ml boluses of a thin, water-soluble contrast agent (Omnipaque 350 mgI/ml, GE Healthcare, Oslo, Norway). If severe aspiration occurred during the VFSS protocol with thin liquids, the research protocol was discontinued. For the patients who penetrated/aspirated, the VFSS was continued with thick liquid and puree to elaborate a dysphagia management plan. The VFSS protocol is described in our previous publication [12].
PAS
The primary outcome variable was the incidence of laryngeal penetration/aspiration on the VFSS as graded by the PAS [20]. The PAS is a validated 8-point scale that captures the depth of airway invasion and the patient’s response to swallowing ( ± ejection of penetrated/aspirated material). The scale ranges from “no material entering the airway” (PAS = 1) to “material entering the airway without a cough response” (PAS = 8). The PAS scoring was conducted jointly by a speech therapist (TI) and a radiologist (IR-K).
FOIS
The secondary outcome variable was the level of functional oral intake as per the Functional Oral Intake Scale (FOIS) [21]. The FOIS is a validated 7-point tool for estimating and documenting change in functional eating abilities over time. The scale ranges from nothing by mouth (level 1) to total oral intake without restrictions (level 7). The FOIS was initially designed for stroke patients, but it has also been widely used with other patient populations, e.g., traumatic brain injury, and head and neck cancer [22, 23]. The FOIS was assessed by the first author based on medical records, a clinical evaluation, and the VFS studies.
Statistical analysis
The Statistical Package for Social Sciences software program (IBM SPSS Statistics for Windows, Version 24.0, Armonk, NY, USA) was used to perform all the statistical analyses. Descriptive statistics [frequency (n), percentage, mean, standard deviation (SD), median, min/max] were used to calculate variable and subgroup characteristics. The normality of the variable distributions was tested using the Shapiro–Wilk test. Group comparisons were tested with the Fisher’s exact test and Mann–Whitney U-test. Differences in the FOIS levels for the whole study sample were tested with the Wilcoxon Signed Rank Test. The statistical significance level was set at 5%. All statistical analyses were performed with the guidance of a statistician.
Results
The patients
In total, 46 out of 94 patients with TCSCI were included in this prospective study. Of the 46 patients, 85% were male. The mean age at the time of the injury was 62.1 years (median 64.0, min–max. 25.7–91.6). Most patient had incomplete injury (78%). Details of the patients’ demographic and injury characteristics are published in our previous study [12]. There were no statistically significant differences between the non-penetrator/aspirators and penetrator/aspirators in age (p = 0.891, Mann–Whitney U-test), gender (p = 0.418, Fisher’s Exact Test), type of injury (complete vs. incomplete, p = 1.000, Fisher’s Exact Test), and time between injury and the first VFSS study (p = 0.691, Mann–Whitney U-test).
The incidence of penetration/aspiration
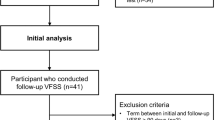
Of the 46 patients, 22 (48%) had penetration/aspiration (PAS score ≥ 3) in the first VFSS. The second VFSS was conducted on 20 patients, of whom 6 patients (30%) had penetration/aspiration. The third VFSS was conducted on 9 patients. Of these, only two (22%) patients were still penetrator/aspirators. One of them showed consistent penetration/aspiration in the fourth and fifth follow-up VFSS at 159 and 273 days post-injury. Based on a telephone interview, the other patient with prolonged aspiration/penetration returned to total oral intake without restrictions and the percutaneous endoscopic gastrostomy (PEG) tube was removed 264 days post-injury without a follow-up VFSS. The flowchart of the VFSS follow-ups and penetration/aspiration results are presented in Fig. 1.
The FOIS outcomes
Forty-two (91%) of the 46 patients were treated at the Tampere University Hospital’s rehabilitation ward after the acute treatment. The mean duration of the first rehabilitation was 51.9 days (SD = 33.3, median = 45.0, min = 7, max = 123). The FOIS levels of these 42 patients after the first clinical evaluation and VFSS and at the time of the final follow-up are presented in Table 1. Differences in initial FOIS scores between the penetrator/aspirators and non-penetrator/aspirators were statistically significant (p = 0.000, Mann–Whitney U-test). In addition, differences between the FOIS scores in the first clinical evaluation and the final follow-up were statistically significant for the whole sample (p = 0.000, Wilcoxon Signed Ranks Test) and between subgroups (penetrator/aspirators vs. non-penetrator/aspirators) (p = 0.000, Mann–Whitney U-test). The majority (n = 37, 88%) of the patients had total oral intake without restrictions at the time of the final follow-up. Only one patient (2%) was still tube-dependent with consistent oral intake.
Of the 46 patients, four (9%) were not treated at Tampere University Hospital’s rehabilitation ward after the acute treatment. One patient (2%) with a FOIS score of 1 died during the acute treatment and three patients (7%) with FOIS scores of 5, 2, and 1 were transferred to another hospital.
Detailed FOIS results in relation to aspiration/penetration status
In total, 19 (86%) patients with penetration/aspiration in the first VFSS were treated at the rehabilitation ward and their detailed FOIS outcomes are presented in Table 2. After 63 days post-injury, half of the patients achieved a FOIS score of 7 indicating the return to an unrestricted diet.
Respectively, 23 (96%) non-penetrator/aspirators were treated at the rehabilitation ward. Twelve of them (52%) were able to start total oral intake without restrictions based on the first VFSS. However, two of them required follow-up VFS studies. One of them had laryngeal regurgitation and the other a right-sided recurrent laryngeal nerve paralysis and laryngeal retention. Despite these problems, both were able to return to total oral intake without restrictions.
Eleven (48%) of the non-penetrator/aspirators required some diet modification for a short period of time. The detailed FOIS outcomes for these 11 patients are presented in Table 3. As seen in Table 3, two patients (Cases 2 and 4) had a prolonged need for tube feeding and a modified diet. Both were able to start oral intake with a modified diet after the first VFSS and the nasogastric tubes were removed. Case 2 had anterior cervical surgery 72 days post-injury and was diagnosed with pneumonia 2 days post-surgery. Because of the pneumonia, Case 2 required intensive care and the nasogastric tube had to be replaced. Case 4 had anterior surgery 30 days post-injury, and a VFSS conducted 2 days post-surgery revealed aspiration. Case 4 eventually required a PEG.
Speech therapy interventions
All patients received speech therapeutic interventions based on their clinical needs. A post hoc analysis revealed that the difference in the number of speech therapy sessions between the penetrator/aspirators and non-penetrator/aspirators was statistically significant (p = 0.000, Mann–Whitney U-test). The penetrator/aspirators (n = 19) received on average 23 speech therapy sessions (SD = 24, median = 14, min = 3, max = 97). Each speech therapy session included one or more different interventions including (total number of interventions): (i) clinical evaluation (57 evaluations), (ii) VFSS (44 studies), (iii) FEES (27 evaluations), (iv) supervising the mealtime (37 sessions), (v) swallowing exercises without food (214 sessions), (vi) swallowing exercises with food (241 sessions), (vii) counseling (9 sessions), and (viii) VitalStim®Therapy -trial (4 sessions).
Respectively, the non-penetrator/aspirators (n = 23) received on average 5 speech therapy sessions (SD = 6, median = 3, min = 2, max = 31). Speech therapy interventions included (total number of interventions): (i) clinical evaluation (36 evaluations), (ii) VFSS (27 studies), (iii) FEES (3 evaluations), (iv) supervising the mealtime (20 sessions), (v) swallowing exercises with food (13 sessions), (vi) counseling (5 sessions), and (vii) voice therapy counseling (4 sessions).
Discussion
The purpose of the current study was to evaluate the recovery of penetration/aspiration and functional feeding outcome in patients with acute TCSCI. The findings of this study suggest that the prognosis to recovery from a propensity for penetrating/aspirating is good in this cohort of patients with TCSCI as the majority of them achieved safe oral nutrition within the first few months post-injury. The generalizability of these results is, naturally, subject to certain limitations. Thus, similar results may not be gained in other clinical contexts. However, our study sample and results are considered to be representative of Finnish patients with acute TCSCI, as they are based on a consecutive series of admitted patients with acute TCSCI.
In the existing literature, only a few studies have evaluated recovery from dysphagia after CSCI [2,3,4, 6]. The methodological heterogeneity, however, makes it difficult to compare our results to prior findings. Our study sample consists of a consecutive series of adult patients with TCSCI recruited with rigorous exclusion criteria. Additionally, the mean age of the patients (62.1 years) in our study sample is higher than in former studies. For example, Wolf and Meiners [2] carried out a study of 51 patients (mean age 43.4 years) with heterogeneous CSCI etiologies. They reported that eight (16%) patients had a PEG tube at the end of the treatment, but only one of them was fully tube-dependent. In the course of their study, 27 out of 51 patients (53%) were followed by repeated FEES. They reported that only three (6%) patients showed consistent severe dysphagia with danger of substantial aspiration based on FEES. Respectively, Abel and colleagues [4] reported that six (8%) patients of their study population of 73 patients (children and adults, mean age 42.9 years) with heterogeneous CSCI etiologies had persistent dysphagia and were discharged with PEG tubes. A retrospective study by Seidl and colleagues [6] reported that ten (6%) of their study population (n = 175, mean age 43.5 years) of patients with heterogeneous CSCI etiologies were discharged with PEG tubes. They followed up 17 patients with repeated FEES. The third FEES revealed that eight of them showed consistent aspiration. Another retrospective study by Brady and colleagues [3] with 72 patients (mean age 55.5 years) reported that the mean level for ASHA NOMS (American Speech-Language-Hearing Association National Outcomes Measurement System, levels 1–7) at admission was 2.7 and at discharge 5.3. The level 5 indicates that all nutrition and hydration needs are met by mouth with minimal diet restrictions.
Our findings highlight that the majority (88%) of our study patients had total oral intake without restrictions at the time of the final follow-up. The differences between the FOIS scores in the first clinical evaluation and the final follow-up were statistically significant for the whole study sample and between the subgroups (aspirators/penetrator vs. non- aspirators/penetrator). Only one patient (2%) showed consistent severe aspiration and was still tube-dependent with a consistent oral intake. Despite the methodological heterogeneity, our findings seem to be in line with previous research. Nevertheless, it is important to note that there are marked differences in patient selection and follow-up time points between these studies. Wolf and Meiners [2], and Seidl and colleagues [6] did not report the length of stay in hospital or any time frames for the follow-ups. Abel and colleagues [4] reported that their patients spent a median of 200 days in a facility following the initial care. For our study patients, the mean duration of the first rehabilitation period was 51.9 days.
A post hoc analysis revealed that the difference in the number of speech therapy sessions between the penetrator/aspirators and non-penetrator/aspirators was statistically significant. It is reasonable to hypothesize that patients with penetration/aspiration require more speech therapeutic interventions than patients without penetration/aspiration. However, it is important to bear in mind that dysphagia is a broader phenomenon. In our study sample, nearly half (48%) of the non-penetrator/aspirators required some diet modification at the beginning of oral intake. Two of them had a special need for speech therapeutic follow-ups. Based on these findings, we consider it important to continue speech therapeutic monitoring of this patient group at a low threshold during the acute phase and rehabilitation, even if the first VFSS does not indicate any penetration/aspiration.
Future research should concentrate on the investigation of the numerous factors that can influence the recovery of penetration/aspiration and functional oral intake outcome in this patient group. Additionally, further studies regarding the role of penetration/aspiration in the incidence of pneumonia in the acute and post-acute settings would be worthwhile. Further, a future study investigating dysphagia in patients with non-traumatic CSCI would be highly worthwhile.
Limitations of the study
The limitations of this study are the small sample size and the fact that the VFSS research protocol included only measured boluses (5 ml, 10 ml, and 20 ml) of a thin, liquid consistency. The small sample size restricts the statistical analyses and further limits the generalizability of the results. Secondly, we decided to focus on only VFSS findings of penetration/aspiration, although dysphagia is a much broader phenomenon. Finally, we were unable to implement VFSS monitoring in accordance with a predetermined schedule for patients participating in the study. Data for this study were collected prospectively during acute hospital care and rehabilitation.
Conclusions
This study suggests that the prognosis to recovery from a propensity for penetrating/aspirating is good in this cohort of patients with TCSCI, and majority of them achieved safe oral nutrition within the first few months post-injury.
References
Kirshblum S, Johnston MV, Brown J, O’Connor KC, Jarosz P. Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil. 1999;80:1101–5.
Wolf C, Meiners TH. Dysphagia in patients with acute cervical spinal cord injury. Spinal Cord. 2003;41:347–53.
Brady S, Miserendino R, Statkus R, Springer T, Hakel M, Stambolis V. Predictors to dysphagia and recovery after cervical spinal cord injury during acute rehabilitation. J Appl Res 2004;4:1–11.
Abel R, Ruf S, Spahn B. Cervical spinal cord injury and deglutition disorders. Dysphagia . 2004;19:87–94.
Shem K, Castillo K, Naran B. Factors associated with dysphagia in individuals with high tetraplegia. Top Spinal Cord Inj Rehabil. 2005;10:8–18.
Seidl RO, Nusser-Muller-Busch R, Kurzweil M, Niedeggen A. Dysphagia in acute tetraplegics: a retrospective study. Spinal Cord. 2010;48:197–201.
Shin JC, Yoo JH, Lee YS, Goo HR, Kim DH. Dysphagia in cervical spinal cord injury. Spinal Cord. 2011;49:1008–13.
Shem K, Castillo K, Wong S, Chang J. Dysphagia in individuals with tetraplegia: incidence and risk factors. J Spinal Cord Med. 2011;34:85–92.
Shem K, Castillo K, Wong SL, Chang J, Kolakowsky-Hayner S. Dysphagia and respiratory care in individuals with tetraplegia: incidence, associated factors, and preventable complications. Top Spinal Cord Inj Rehabil. 2012;18:15–22.
Chaw E, Shem K, Castillo K, Wong SL, Chang J. Dysphagia and associated respiratory considerations in cervical spinal cord injury. Top Spinal Cord Inj Rehabil. 2012;18:291–9.
Shem KL, Castillo K, Wong SL, Chang J, Kao MC, Kolakowsky-Hayner SA. Diagnostic accuracy of bedside swallow evaluation versus videofluoroscopy to assess dysphagia in individuals with tetraplegia. Pm R. 2012 ;4:283–9.
Ihalainen T, Rinta-Kiikka I, Luoto TM, Koskinen EA, Korpijaakko-Huuhka A, Ronkainen A. Traumatic cervical spinal cord injury: a prospective clinical study of laryngeal penetration and aspiration. Spinal Cord. 2017;55:979–84.
Ihalainen T, Rinta-Kiikka I, Luoto TM, Thesleff T, Helminen M, Korpijaakko-Huuhka A, et al. Risk factors for laryngeal penetration-aspiration in patients with acute traumatic cervical spinal cord injury. Spine J. 2018;18:81–87.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T. et al. International spinal cord injury core data set. Spinal Cord. 2006;44:535–40.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards For Neurological Classification Of Spinal Cord Injury. J Spinal Cord Med. 2011;34:547–54.
Robbins J, Coyle J, Rosenbek J, Roecker E, Wood J. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999;14:228–32.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;21:270–4.
Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol-Head & Neck Surg. 2010;142:208–13.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia . 1996;11:93–98.
Crary MA, Mann GDC, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Hansen TS, Engberg AW, Larsen K. Functional oral intake and time to reach unrestricted dieting for patients with traumatic brain injury. Arch Phys Med Rehabil. 2008;89:1556–62.
Molen Lvd, Rossum MAv, Burkhead LM, Smeele LE Rasch CRN, Hilgers FJM. A randomized preventive rehabilitation trial in advanced head and neck cancer patients treated with chemoradiotherapy: feasibility, compliance, and short-term effects. Dysphagia. 2011;26:155–70.
Acknowledgements
The authors thank the patients, biostatistician Mika Helminen, and research assistant Anne Simi for their assistance.
Funding
This study was funded by Maire Taponen säätiö, The Finnish Dysphagia Rehabilitation Association, and Finnish Association of Speech Therapists.
Author contributions
TI contributed to the study design, data collection, data analysis, data interpretation, and article preparation. TML contributed to the data interpretation and article preparation. IR-K contributed to the data collection and article preparation. A-MK-H contributed to the article preparation. AR contributed to the study design and article preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TI has received research grants from Maire Taponen säätiö, The Finnish Dysphagia Rehabilitation Association, and Finnish Association of Speech Therapists. TML declares that he has no conflict of interest. IR-K declares that she has no conflict of interest. AR declares that he has no conflict of interest. A-MK-H declares that she has no conflict of interest.
Rights and permissions
About this article
Cite this article
Ihalainen, T., Luoto, T.M., Rinta-Kiikka, I. et al. Traumatic cervical spinal cord injury: recovery of penetration/aspiration and functional feeding outcome. Spinal Cord 56, 1000–1007 (2018). https://doi.org/10.1038/s41393-018-0091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0091-1