Abstract
Study design
Repeated measures design.
Objectives
To determine the reproducibility of total-body and regional-body composition assessments from a total-body scan using dual-energy x-ray absorptiometry (DXA) in persons with spinal cord injury (SCI).
Methods
Twenty-four individuals with SCI completed within-day short-term precision testing by repositioning study participants between scans. An additional and separate cohort of 22 individuals with SCI were scanned twice on a GE-Lunar DXA scanner separated by a 4-week interval to assess the long-term precision assessment. The root mean square coefficient of variation percent (RMS-CV%) values for the regional and total body composition was calculated.
Results
For the same day, short-term precision assessment, the RMS-CV% for each region did not exceed 5.6, 2.7, 3.8, 6.5, 5.8, and 2.3% for arms, legs, trunk, android and gynoid regions, and total body mass, respectively. In the long-term precision assessment, the RMS-CV% for each region did not exceed 6.0, 3.0, 4.4, 8.2, 3.4, and 2.0% for arms, legs, trunk, android, gynoid, and total body mass. Moreover, the interclass-correlation coefficient in the long-term precision group demonstrated excellent linear agreement between repeat scans for all regions (r > 0.97).
Conclusions
The precision error of the total body composition variables in our SCI cohort was similar to those reported in the literature for nondisabled individuals, and the precision errors of the regional body composition compartments were notably higher, but similar to the regional precision errors reported in the general population.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) results in extreme physical inactivity with a decrease in skeletal muscle mass, primarily below the level of lesion, that results in a decreased resting energy expenditure and increased total body and visceral adiposity [1,2,3,4,5,6,7]. In a monozygotic twin study, individuals with SCI have lower lean mass (LM) compared to their non-SCI cotwin. The authors concluded that on average adults with SCI may lose up to 4 kg of LM for every decade after injury and accompanying immobilization [7]. As a result of these adverse body composition changes, persons with chronic SCI may be at greater risk for obesity, abnormal carbohydrate metabolism, and cardiovascular disease [2,3,4,5]. Assessment of body composition has gained considerable attention because of its relationship to dietary habits, exercise interventions, and metabolic profiles [3,4,5]. Dual-energy X-ray absorptiometry (DXA) has been used in both clinical and research settings for more than three decades to evaluate different body composition compartments. Briefly, DXA utilizes an X-ray source to emit two distinct photoelectric peaks to obtain the attenuation coefficient of fat mass (FM), LM, and bone mineral content (BMC).
In exercise intervention trials following 12 weeks of electrically-evoked resistance training, persons with SCI gained between 0.8−1.6 kg of LM by DXA measurement [5, 8]. The increase in LM is vital to cardio-metabolic health after SCI [3, 5] and, therefore, providing a tool with sufficiently high precision of measurement for soft tissue body composition is essential. In a study of 17 persons with chronic SCI, Astorino et al. [9] used total body DXA to measure changes in FM, fat free mass (FFM), and body weight immediately before and after 6 months of high volume (>6 h per week) activity based therapy consisting of dynamic resistance training, functional electrical stimulation (FES), body weight supported treadmill training, combined with load bearing training. The authors found large variability in individual changes with some participants showing increase, maintenance, or decrease in FFM, with the total group showing a significant increase in total body FFM and nonsignificant changes in all other variables [9]. In another study by Bakkum et al. [10], a multicenter randomized controlled trial was performed that compared 16-weeks of twice a week hand cycling to the equivalent quantity of hybrid cycling (lower body FES and upper body cycling) on visceral adiposity in persons with chronic SCI. The authors found a 3.6% and 4.7% reduction in trunk and android fat, respectively. While it is appreciated that the authors in the former study performed an inter-day precision assessment to obtain the coefficient of variation, knowledge of both the short and long-term precision error would have allowed investigators to optimally power the study based on the approximate effect size for different body composition variables and the precision error of the total body and regional areas. Despite the commonly reported precision error by DXA manufacturers, individual technologists who acquire DXA measurements have observed variable precision assessments dependent upon the population. For example, in a multicenter trial, the data from one of the seven study sites were removed because the precision error of the site was significantly greater than the other six study sites [11]. If the precision error of a densitometer measurement is not sufficiently small, then detection of soft tissue body composition changes, such as those after rehabilitation interventions in longitudinal clinical trials, may not be reliably determined. Several recent reports have identified the precision error of total body and regional body composition parameters from a total body DXA scan in the able-bodied population [12, 13]. In a study by Lohman et al. [14], the authors documented the “on and off” the table reproducibility of total body DXA in measuring LM, FM, BMC. Utilizing Pearson correlation coefficients to quantify reliability, the authors found excellent correlations between repeat scans for total body BMC (r = 0.99), LM (r = 0.99), and FM (r = 1.00), and bone mineral density (BMD) (r = 0.98), with regional reliability measurements that were considerably less precise than the total body measurements. Many short-term precision studies have utilized simple “repositioning” of the total body, torso, legs, and arms as a surrogate for an altered position from remounting the table. However, the majority of precision studies have utilized an “on and off” the table approach, a method by which the SCI participant dismounts the table between scans that more accurately captures the variability inherent performing repeat scans in practice. In the first treatment-control testosterone replacement pilot study in persons with SCI, Bauman et al. [15] reported precision errors of 1.2% for LM and 2.2% for FM in 30 SCI participants using the “on-and-off the table” method, as recommended by the International Society for Clinical Densitometry.
The purpose of the current study was to evaluate the reproducibility of total and regional DXA-derived body composition values to obtain the precision error of two total body DXA scans performed on the same day using the “on-and-off” table method (short-term precision) and of two total body DXA scans performed on separate days within a 4-week period (long-term precision). The primary hypothesis was that the CV of regional and total body composition measurement variables will be comparable to what has been previously reported in the literature for able-bodied individuals.
Methods
Study participants
Short-term precision assessment
Twenty-four men were recruited from the James J. Peters VA Medical Center (JJPVAMC), Bronx, NY (n = 18, clinicaltrials.gov NCT00886145) and the Richmond VA Medical Center (RVAMC), Richmond, VA (n = 6, clinicaltrials.gov NCT01652040) to participate in the short-term precision study. The complete demographic characteristics for the group with short-term precision have been provided (Table 1). Because persons with SCI are extremely difficult to remove from and place back on the scanning table, two investigators who were blinded to the study’s intent positioned the participants before each scan was acquired. After the participant was correctly positioned the scan was repeated.
Long-term precision
A separate group of twenty-two men (ages 18−50 years) were recruited from the RVAMC for participation in this study as part of enrollment in an ongoing clinical trial [clinicaltrials.gov NCT01652040] [16]. All had motor-complete SCI with levels of injury from cervical level-5 to lumbar level-2 and were classified as A or B by the ISNCSCI; the complete demographic characteristics for the group with long-term precision have been provided (Table 1). Participants were recruited by word of mouth and posted flyers or from the associated SCI clinics at the participating institution. All aspects related to the study design and methodology were reviewed and approved by the institutional review boards at the participating sites. The study was approved by the local ethics committee board and conducted according to the Declaration of Helsinki and after meeting inclusion criteria, participants were provided verbal and written consent. Persons were excluded with the following medical comorbidities: cardiovascular disease, uncontrolled type II diabetes and those on insulin, decubitus pressure sores (stage 2 or greater) and current urinary tract infections or symptoms.
Dual energy x-ray absorptiometry (DXA)
The total body and regional composition for FFM, FM, %FM, LM, and BMC body composition compartments for the total body, trunk, legs, arms, android, and gynoid regions were measured by DXA [2, 4, 6,7,8, 14]. Body composition was measured by whole body scans using a GE Lunar Prodigy Advance scanner (GE Lunar Inc., Madison, WI, USA). Transfer to the DXA scanner was performed using either a ceiling lift or self-transfer with or without sliding boards. Participants were asked to take off any metal, void their bladder, and dress in light clothes prior to transfer to the DXA table. Using the NHANES scanning method [12], both knees were strapped together using a large velcro strap above the knee joints and every effort was made to ensure that each leg is placed in neutral position with the big toe facing upward toward the celling. A lead research investigator checked that the whole-body posture was aligned straight with no rotation in the pelvis or shifting of the trunk to one side. Because of the difficulty in keeping the arms close to the body in large individuals or in cervical SCI, arms were strapped close to the body in mid-prone position to ensure the total body was within the scanning field to ensure consistency among all the participants. The standard mode scan was used with a radiation dose of 0.4 µGy in all but two participants who had body weights greater than 100 kg that required a higher radiation dose (0.8 µGy) to acquire the image. All scans were performed and analyzed by a trained DXA operator using Lunar software version 10.5. The total body cuts were placed by the computer auto analysis program delineating anatomical regions of interest with final adjustments made manually by the technician to ensure optimum inter-participant reproducibility. As part of daily quality assurance program, the DXA scanner was calibrated using the quality control phantom (L: 197.7, W: 60.1) according to the manufacturer guidelines for both short-term and long-term precision studies (S1).
After transferring to the DXA table, the wheelchair was weighed without the participant. The weight of the wheelchair was then subtracted from the weight of the wheelchair and the participant to measure their absolute total body weight. Height was measured in a supine lying position on the left side of the body and every effort was considered to place the knee joint into full extension and the foot into a neutral position by using a sliding board to maintain an upright position of the foot. The BMI was calculated as the body mass/height2 (kg/m2).
Statistical analysis
For estimation of the short term (n = 24) and long term (n = 22) precision error, the RMS-SD and the root mean square coefficient of variation percent (RMS-CV%) statistics were used according to the ISCD guidelines using the following calculations. For both precision error assessments, the root mean square (RMS) average of each participant’s variance (i.e., standard deviation squared [SD2]) was obtained from the repeated measures. Therefore, the first step in calculating the short-term precision is to calculate the variance for each participant given by the following equation [17, 18]:
where \(n_j\) is the number of measurements performed on one subject (note that nj should be the same for all subjects). \(x_{ij}\) is the ith result from the specific site obtained from the machine for subject j. \(\bar x_j\) is the average of the repeated measures for subject j. This can be expressed as a coefficient of variation (CV) of repeated measures which is given as a percent:
These short-term precision values are then used to find the short-term precision for the device using the following equation:
fwhere mj are the number of subjects used in the precision assessment and \({\mathrm SD}_j^2\) is the variance obtained from Eq. 1. When expressed as a percentage, the following equation will be used:
For long-term precision study, interclass-correlation coefficient (ICC) analyses were also performed to identify associations of the regional and total body compositions between scan 1 and scan 2 in the long-term precision group. Statistical significance was accepted at P < 0.05. All values are presented as the mean ± standard deviation. Statistical analyses were performed using SPSS, version 23.
Results
The physical and SCI characteristic of both studies are presented (Table 1). In the reproducibility trial over 4-week period, height, weight, and BMI were not significantly different between the first and second scans.
Phantom quality assurance block
The quality control assurance of the phantom box that was scanned 22 times (44 times in total for scans 1 and 2). The RMS-CV% of the %FM, BMD, BMC, and area were 0.026%, 0.04%, 0,024%, 0.065%, respectively, between the first and second scans (S1).
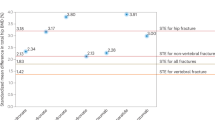
Short-term precision [2 repeat total body scans on the same day]
The short-term precision mean values for the same day (“on-off table”) assessment for regional and total body %FM, FM, LM, and BMC are presented (Table 2). The paired analysis indicated there were no statistical differences between scan 1 and scan 2. The RMS-CV% for each region did not exceed 5.6, 2.7, 3.8, 6.5, 5.8, and 2.3% for arms, legs, trunk, android, gynoid, and total body between repeated scans (Table 3).
Long-term precision [2 repeat total body scans 4 weeks apart]
The long-term precision mean values of scan 1 and scan 2 for regional and total body %FM, FM, LM, and BMC, are presented (Table 4) with the paired analysis demonstrating that there were no statistical differences between the scans with the exception of that for the android region %FM (P = 0.02). The RMS-SD and RMS-CV% for the regional and total body %FM, FM, LM, and BMC for the long-term precision data are also presented (Table 3). The RMS-CV% for each region did not exceed 6.0, 3.0, 4.4, 8.2, 3.4, and 2.0% for arms, legs, trunk, android, gynoid, and total body between repeated scans. Height was not significantly different (P = 0.6) between scan 1 (178.9 ± 5.8 cm) and scan 2 (179.1 ± 6.1 cm). For scan 1, weight measured by weighing scale was not significantly different from total body weight measured by DXA (79.4 ± 12.4 vs. 79.4 ± 12.2, P = 0.9, Table 3).
Long-term precision group and ICC
For arms, ICC for %FM (r = 0.99; 95%CI: 0.98−0.997, P < 0.0001), FM (r = 0.97; 95%CI: 0.94−0.99, P < 0.0001), LM (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) and BMC (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) showed a high level of agreement between scan 1 and scan 2. For legs, ICC for %FM (r = 0.99; 95%CI: 0.98−0.997, P < 0.0001), FM (r = 0.97; 95%CI: 0.94–0.99, P < 0.0001), LM (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) and BMC (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) showed a high level of agreement between scan 1 and scan 2. For trunk, ICC for %FM (r = 0.99; 95%CI: 0.98−0.997, P < 0.0001), FM (r = 0.97; 95%CI: 0.94−0.99, P < 0.0001), LM (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) and BMC (r = 0.98; 95%CI: 0.97−0.99, P < 0.0001) showed a high level of agreement between scan 1 and scan 2. For total body, ICC for %FM (r = 0.99; 95%CI: 0.98−0.997, P < 0.0001), FM (r = 0.97; 95%CI: 0.94–0.99, P < 0.0001), LM (r = 0.98; 95%CI: 0.97–0.99, P < 0.0001) and BMC (r = 0.98; 95%CI: 0.97–0.99, P < 0.0001) showed a high level of agreement between scan 1 and scan 2.
Discussion
The current study determined the short-term and long-term precision of total and regional soft tissue body composition in men with SCI. For the same-day short-term and long-term precision assessments (e.g., RMS-CV%) for each region of interest were quite similar. Moreover, the ICC in the long-term precision group demonstrated excellent linear agreement between repeat scans for all regions (r > 0.97).
A quantifiable precision error is inherent to densitometry measurement, and it represents the non-biological changes that can be attributed to random error; such error must be sufficiently minor to be able to detect the effect from an intervention with confidence [19]. Technologists who acquire DXA measurements on different patient populations observe variable precision assessments with the appreciated potential to confound interpretations of the findings. The ISCD has developed an official position regarding the use of DXA for body composition assessment and limited its applications to specific medical conditions including patients with HIV, obese individuals undergoing weigh loss programs, candidates for bariatric surgery, and persons with sarcopenia [20]. The ISCD recommends the minimum acceptable precision error should not exceed 3, 2, and 2% for total FM, total LM, and percent FM, respectively; the precision measurement should be performed in the population of interest [21]. This general guideline does not specifically address the regional areas because acceptable reliability studies on the arms, legs, and trunk have not been performed to date. There is an obvious need to determine the magnitude of error in regional and total body composition when conducting longitudinal trials after SCI [3, 8, 15, 22], and a paucity of work has been reported in persons with SCI that addresses the FM, LM, and BMC precision error that is derived from a total body DXA scan.
Longitudinal randomized clinical trials are essential to determine what rehabilitation interventions prove to be efficacious in reversing or preventing the adverse body composition changes observed in the chronic SCI population [15, 22]. Clinical trials that address rehabilitation interventions in persons with SCI require significant resources and often poise daunting challenges to recruit sample sizes that are adequate to address the questions being considered; therefore, accurately determining the precision error is essential to quantify the variability of DXA and to ensure valid outcomes [22]. Obstacles to successful DXA scanning in persons with SCI can be attributed to difficulty in positioning due to increased spasticity, tone, and contractures, as well as the logistical obstacle of transferring participants to a DXA table top height that is comfortable and safe [23]. As a result of these obstacles, the majority of DXA reliability studies have utilized a same-day “on-and-off” the table methodology where by participants are repositioned between DXA scans as the most feasible option to obtain the precision error [8, 24, 25]. In a reliability study by Kiebzak et al. [26], the authors performed total body DXA precision assessments on healthy male and female subjects. The total body BMD and BMC precision error was found to be 0.62% and 1.09%, respectively; while soft tissue precision error for fat tissue mass) and lean tissue mass was found to be 2.0% and 1.11%, respectively. In another study by Ley et al. [27], the authors established precision estimates for postmenopausal women with a precision error for total LM of 1.8% and total FM of 2.9%, with regional measurements showing more variability, but all were less than 5%. The short-term precision error findings presented herein are in agreement with these previous studies, and within the range reported in the general population.
Assessments of the long-term precision have utilized the ISCD guideline to calculate the precision error but performed the repeat scans on separate days, a study design that more accurately reflects the true change from repeated measurements and is the preferred study design for reliability studies. A between day (long -term) study design can capture the effect of confounding variables such as variability in participant hydration status, repositioning errors, and calibration stability that can lead to significantly larger precision error estimates [28]. In contrast, the within day (short-term) study design is a more practical surrogate method to measure the precision error from repeat scans and is the most common methodology used in the clinical or research settings. As a result, in the current study it was necessary to stratify the dataset into participants who completed repeat scans within the same day and those who completed repeat scans on different days. In a study by Powers et al. [29], the authors determined the long-term precision of regional and total soft tissue body composition in 609 participants who were recruited as a part of the National Health and Nutrition Examination Survey (NHANES) 2000–2002. Their findings indicated that the RMS-CV% ranged from 1.47–4.27, 1.41–2.28, 1.41–2.75 and 1.1–1.97 for arms, legs, trunk and total body, respectively. In the current long-term precision study, the RMS-CV% ranged from 2.7–4.4%, 1.27–3%, 2.0–4.4% and 1.4–1.96% for arms, legs, trunk and total body, respectively. The range of RMS-CV% for arms, legs, and total body is similar to what has been reported in the NHANES datasets, with the exception of the RMS-CV% for the trunk soft tissue variables that were notably higher in the current study. Several factors may have played a role in the observed discrepancy in the findings between these two studies. DXA machines by different manufacturers are appreciated to have different FM and LM values, and they also have different estimates of precision error [30]. The current study utilized a GE Lunar Prodigy densitometer, while the study by Powers et al. [29] utilized a Hologic densitometer to assess the precision error of soft tissue mass. Furthermore, the time period between repeat scans was 8 days in the NHANES study compared to 4 weeks in the current study, the maximum period deemed acceptable by the ISCD to determine the reproducibility of repeated scans [12, 20, 21]. We have previously shown that the caloric intake and macronutrients were stable across 4-week period in persons with motor-complete SCI [4], which provides support that change in soft tissue body composition without an intervention in persons with SCI is unlikely during this time frame.
An additional factor that may increase the precision error from a total body DXA scan include the failure to accurately reposition participant’s limbs between scans. The day to day precision is likely to be impacted by progressing skeletal muscle atrophy and with accompanying increases in intramuscular fat [3, 5], this may contribute to an increased precision error during longitudinal studies. Because of abnormal anatomical considerations which include joint contractures, leg-pelvic discrepancy, trunk scoliosis, and kyphosis, it may be difficult to position participants with SCI according to the recommended ISCD guidelines. However, our estimates of short-term precision errors were similar to those for long-term precision. Surprisingly, the range of the RMS-CV% was even higher in the arms in the short-term compared to long-term precision. Our findings of increased variability in the short-term precision cohort may have been because 67% of the participants had tetraplegia compared to 41% of the participants in the long-term precision study, a difference in group composition which was likely to relatively inflate the precision error in the short-term cohort.
Limitations
The primary limitation of this study was the relatively small sample size and the lack of statistical power to calculate the least significant change (LSC) of the total body composition variables. To report the LSC with a 95% confidence interval, one of three precision assessment methodologies must be adopted: two repeat scans on 30 participants, three repeat scans on 15 participants, or four repeat scans on ten participants. In the current study, vertebral hardware fusion was not accounted; however, this is likely to have trivial effects on our findings because a within-subject design was primarily employed. Only men with SCI were included since the original parent clinical trial was conducted to investigate the effect of resistance training and testosterone replacement therapy on men with SCI. Therefore, the generalizability of the results should be considered with caution and future studies need to include women with SCI. We have also tested the precision in a supine position utilizing the NHANES hands prone total body scanning methodology [31]. A recent report demonstrated a lower precision error utilizing the mid-prone hand position [25], a finding that may help improve precision error in the SCI population given the excessive abdominal adiposity in many individuals that can interfere with proper positioning to allow for uniform demarcation of regions of interest. This mid-prone position was standardized as the Nana protocol [32], and in a recent report the precision error was superior to that obtained in the NHANES protocol when utilizing foam positioning aids to standardize intra-participant distance between the legs and the distance separating the arm from the trunk.
Conclusion
The use of DXA in persons with SCI is safe, readily available, and relatively easy to perform, but there is little information that has been reported to date on the reliability of soft tissue body composition measurements that are derived from the total body scan. Our estimate of short-term and long-term precision errors for these measurements is likely to be higher than able-bodied control participants, but the error is such that longitudinal changes in tissue compartment measurements over extended periods of time would likely be reliable, and thus feasible to perform. The precision error of total body composition variables was equivalent to that of previous reports in the nondisabled; values in our SCI cohort were notably higher in regional body composition compartments, which is also similar to those reported in prior studies in the general population. Our study adds to the body of evidence that total and regional body composition assessment by DXA is highly reproducible among persons with SCI. The findings presented herein can be used for interpretation of those that have been generated in prior longitudinal findings, as well as for use in power calculations when determining minimum sample size in future clinical trials in which tissue compartment measurement by total body DXA is the the primary outcome variable.
References
Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371–8.
Gorgey AS, Gater DR. Regional and relative adiposity patterns in relation to carbohydrate and lipid metabolism in men with spinal cord injury. Appl Physiol Nutr Metab. 2011;36:107–14.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR. Effects of spinal cord injury on body composition and metabolic profile - part I. J Spinal Cord Med. 2014;37:693–702.
Gorgey AS, Caudill C, Sistrun S, Khalil RE, Gill R, Castillo T, et al. Frequency of dietary recalls, nutritional assessment, and body composition assessment in men with chronic spinal cord injury. Arch Phys Med Rehabil. 2015;96:1646–53.
Gorgey AS, Mather KJ, Cupp HR, Gater DR. Effects of resistance training on adiposity and metabolism after spinal cord injury. Med Sci Sports Exerc. 2012;44:165–74.
Paulson TA, Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr, et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95:2398–407.
Spungen AM, Wang J, Pierson RN, Bauman WA. Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol. 2000;88:1310–5.
Gorgey AS, Caudill C, Khalil RE. Effects of once weekly NMES training on knee extensors fatigue and body composition in a person with spinal cord injury. J Spinal Cord Med. 2016;39:99–102.
Astorino TA, Harness ET, Witzke KA. Chronic activity-based therapy does not improve body composition, insulin-like growth factor-I, adiponectin, or myostatin in persons with spinal cord injury. J Spinal Cord Med. 2015;38:615–25.
Bakkum AJ, Bishop NC, Goosey-Tolfrey VL, Stolwijk-Swüste JM, van Kuppevelt DJ, de Groot S, et al. Effects of hybrid cycle and handcycle exercise on cardiovascular disease risk factors in people with spinal cord injury: a randomized controlled trial. J Rehabil Med. 2015;47:523–30.
Morgan SL, Abercrombie W, Lee JY. Need for precision studies at individual institutions and assessment of size of regions of interest on serial DXA scans. J Clin Densitom. 2003;6:97–101.
Kerr A, Slater GJ, Byrne N, Nana A. Reliability of 2 different positioning protocols for dual-energy X-ray absorptiometry measurement of body composition in healthy adults. J Clin Densitom. 2016;19:282–9.
Saarelainen J, Hakulinen M, Rikkonen T, Kröger H, Koivumaa-Honkanen H, Honkanen R, et al. Inclusion of regional body composition parameters improves bone mineral density cross-calibration between GE lunar prodigy and iDXA densitometers. J Clin Densitom. 2017;20:97–105.
Lohman M, Tallroth K, Kettunen JA, Marttinen MT. Reproducibility of dual-energy x-ray absorptiometry total and regional body composition measurements using different scanning positions and definitions of regions. Metabolism. 2009;58:1663–8.
Bauman WA, Cirnigliaro CM, La Fountaine MF, Jensen AM, Wecht JM, Kirshblum SC, et al. A small-scale clinical trial to determine the safety and efficacy of testosterone replacement therapy in hypogonadal men with spinal cord injury. Horm Metab Res. 2011;43:574–9.
Gorgey AS, Khalil RE, Gill R, O’Brien LC, Lavis T, Castillo T, et al. Effects of testosterone and evoked resistance exercise after spinal cord injury (TEREX-SCI): study protocol for a randomised controlled trial. BMJ Open. 2017;7:e014125.
Glüer CC, Blake G, Lu Y, Blunt BA, Jergas M, Genant HK. Accurate assessment of precision errors: how to measure the reproducibility of bone densitometry techniques. Osteoporos Int. 1995;5:262–70.
Baim S, Wilson CR, Lewiecki EM, Luckey MM, Downs RW, Lentle BC. Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom. 2005;8:371–8.
Cirnigliaro CM, Myslinski MJ, La Fountaine MF, Kirshblum SC, Forrest GF, Bauman WA. Bone loss at the distal femur and proximal tibia in persons with spinal cord injury: imaging approaches, risk of fracture, and potential treatment options. Osteoporos Int. 2017;28:747–65.
Shepherd JA, Baim S, Bilezikian JP, Schousboe JT. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on Body Composition. J Clin Densitom. 2013;16:489–95.
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitom. 2013;16:455–66.
Gorgey AS, Martin H, Metz A, Khalil RE, Dolbow DR, Gater DR. Longitudinal changes in body composition and metabolic profile between exercise clinical trials in men with chronic spinal cord injury. J Spinal Cord Med. 2016;39:699–712.
Morse LR, Geller A, Battaglino RA, Stolzmann KL, Matthess K, Lazzari AA, et al. Barriers to providing dual energy x-ray absorptiometry services to individuals with spinal cord injury. Am J Phys Med Rehabil. 2009;88:57–60.
Watson LPE, Venables MC, Murgatroyd PR. An investigation into the differences in bone density and body composition measurements between 2 GE lunar densitometers and their comparison to a 4-component model. J Clin Densitom. 2017;20:498–506.
Thurlow S, Oldroyd B, Hind K. Effect of hand positioning on DXA total and regional bone and body composition parameters, precision error, and least significant change. J Clin Densitom. In Press 2018.
Kiebzak GM, Leamy LJ, Pierson LM, Nord RH, Zhang ZY. Measurement precision of body composition variables using the lunar DPX-L densitometer. J Clin Densitom. 2000;3:35–41.
Ley CJ, Lees B, Stevenson JC. Sex- and menopause-associated changes in body-fat distribution. Am J Clin Nutr. 1992;55:950–4.
Engelke K, Glüer CC, Genant HK. Factors influencing short-term precision of dual X-ray bone absorptiometry (DXA) of spine and femur. Calcif Tissue Int. 1995;56:19–25.
Powers C, Fan B, Borrud LG, Looker AC, Shepherd JA. Long-term precision of dual-energy X-ray absorptiometry body composition measurements and association with their covariates. J Clin Densitom. 2015;18:76–85.
Malouf J, DiGregorio S, Del Rio L, Torres F, Marin AM, Farrerons J, et al. Fat tissue measurements by dual-energy x-ray absorptiometry: cross-calibration of 3 different fan-beam instruments. J Clin Densitom. 2013;16:212–22.
Hangartner TN, Warner S, Braillon P, Jankowski L, Shepherd J. The official positions of the international society for clinical densitometry: acquisition of dual-energy X-ray absorptiometry body composition and considerations regarding analysis and repeatability of measures. J Clin Densitom. 2013;16:520–36.
Nana A, Slater GJ, Hopkins WG, Burke LM. Effects of daily activities on dual-energy X-ray absorptiometry measurements of body composition in active people. Med Sci Sports Exerc. 2012;44:180–9.
Acknowledgements
This work was supported by the Office of Research and Development, Medical Research Service, Department of Veterans Affairs (# B7867-W and #B2020-C).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Gorgey, A.S., Cirnigliaro, C.M., Bauman, W.A. et al. Estimates of the precision of regional and whole body composition by dual-energy x-ray absorptiometry in persons with chronic spinal cord injury. Spinal Cord 56, 987–995 (2018). https://doi.org/10.1038/s41393-018-0079-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-018-0079-x
This article is cited by
-
Denervation impacts muscle quality and knee bone mineral density after spinal cord injury
Spinal Cord (2023)
-
Predictors of muscle hypertrophy responsiveness to electrically evoked resistance training after spinal cord injury
European Journal of Applied Physiology (2022)
-
Serum testosterone levels may influence body composition and cardiometabolic health in men with spinal cord injury
Spinal Cord (2019)
-
Plasma adiponectin levels are correlated with body composition, metabolic profiles, and mitochondrial markers in individuals with chronic spinal cord injury
Spinal Cord (2018)