Abstract
Study design
Prospective.
Objectives
To determine the optimum gonadotropin-releasing hormone (GnRH) dose to identify dysfunction of the hypothalamic–pituitary–gonadal axis in men with spinal cord injury (SCI).
Setting
Metropolitan Area Hospitals, New York and New Jersey, USA.
Methods
SCI men (16 hypogonadal (HG = serum testosterone <12.1 nmol/l) and 14 eugonadal (EG)) and able-bodied (AB) men (27 HG and 11 EG) were studied. GnRH (10, 50, and 100 μg) was randomly administered intravenously on three separate visits. Blood samples were collected post-GnRH for serum-luteinizing hormone (LH) and follicular-stimulating hormone (FSH).
Results
HG and EG men had a similar proportion of clinically acceptable gonadotropin responses to all three GnRH doses. The incremental gonadotropin responses to GnRH were not significantly different across the groups. However, in the SCI-HG group, GnRH of 100 μg resulted in the greatest integrated FSH response, and in the SCI-EG group, GnRH of 50 μg resulted in the greatest integrated LH response compared with the AB groups. A consistent, but not significant, absolute increase in gonadotropin release was observed in the SCI groups at all GnRH doses.
Conclusions
Lower doses of GnRH did not improve the ability to identify the clinical dysfunction of the hypothalamic–pituitary–gonadal axis. However, the absolutely higher SCI-HG FSH response to GnRH of 100 μg and a higher SCI-EG LH response to GnRH of 50 μg, along with a higher gonadotropin release at all GnRH doses, albeit not significant, suggests a hypothalamic–pituitary dysfunction in persons with SCI.
Similar content being viewed by others
Introduction
Paralysis and the associated physical inactivity in persons with spinal cord injury (SCI) result in muscle atrophy that will reduce resting and total daily energy expenditure. In the absence of sufficient restriction of caloric intake, adiposity and adverse metabolic consequences may result [1, 2].Compared with the general male population, men with SCI are observed to have an elevated prevalence of low-serum testosterone levels, and hypogonadism appears to increase with each advancing decade of life [3]. Loss of muscle mass and gain of adiposity would be anticipated to negatively impact general health due to adverse metabolic changes, impair physical function, reduce social integration, and decrease the quality of life [4–6]. In persons with SCI, dysfunction of the hypothalamic–pituitary–gonadal axis may result in depression of serum testosterone levels that would be anticipated to worsen the adverse body composition changes that occur as a consequence of paralysis and immobilization, as well as increase the likelihood of developing the adverse metabolic sequelae of SCI [7–11]. Testosterone deficiency is also associated with fatigue, depression, and other negative mood alterations [12–14]. In addition, one possible etiology for reduced semen quality is dysfunction of the hypothalamic–pituitary–testicular axis [15–17]. Thus, expanding our understanding of the occurrence of a dysfunctional hypothalamic–pituitary–gonadal axis may raise awareness and the ability to identify, diagnose, and treat this disorder.
The gonadotropin-releasing hormone (GnRH) stimulation test has been routinely used in clinical practice to determine the integrity of the hypothalamic–pituitary–gonadal axis. In the conventional approach, GnRH of 100 µg is administered intravenously and blood is collected for gonadotropin levels at 30 and/or 60 min after a provocative stimulus. The original work that determined the most appropriate dose of GnRH to administer for clinical purposes was performed about 40 years ago, and subsequently, there has been little interest to revisit the dose of GnRH in an attempt to further elucidate the function of the hypothalamic–pituitary–gonadal axis in various clinical conditions that may be associated with central dysregulation.
Our group reported that the hypothalamic–pituitary–gonadal axis is generally intact when evaluated by standard challenge testing in persons with spinal cord injury (SCI); albeit, the absolute gonadotropin response to GnRH of 100 µg was higher in persons with SCI who were classified as “responders” (i.e., adequate response by conventional clinical criteria) to provocative pituitary stimulation compared with healthy able-bodied controls who were classified as “responders” [18]. The testicular response to a conventional dose of human chorionic gonadotropin (hCG; 4000 IU) or with lower doses of hCG (400 and 1000) in those with SCI was generally appropriate, regardless of whether the participants had low or normal serum testosterone levels [18, 19]. Of note, whether an individual with SCI was hypogonadal or eugonadal was not predictive of whether the person would respond with an appropriate clinical response to the standard stimulation dose of hCG. The authors speculated that because peripheral stimulation to hCG was essentially normal in those with SCI, a more subtle central problem due to an insufficient hypothalamic drive to gonadotropin release should be considered.
The incidence of men with SCI who have low levels of testosterone (T) is reported to be between 40 and 60%, based on varying populations studied and different threshold values for T concentration to define hypogonadism [3, 8, 11, 20]. The etiology of hypogonadism is most likely multifactorial and includes general health [21], nutrition [22], medication usage (especially psychotropic agents and opioids) [23–26], alcohol consumption [27, 28], level, and completeness and duration of the neurological lesion, possibly directly related to the degree of adiposity [29]. Despite its etiology, T deficiency, as a relative or an absolute condition, may influence the tendency to lose a lean tissue and gain fat mass, predispose to adverse carbohydrate [30–33] and lipid metabolism [30, 31, 34, 35], and lower-energy expenditure [6, 36, 37].
Impotence and infertility are also common conditions among men with SCI [38–42]. Of the many possible explanations for poor semen quality [15], one possible etiology is the dysfunction of the hypothalamic–pituitary–testicular axis [16, 17, 43]. Early reports that employed provocative stimulation of the axis to assess testicular function have been inconclusive with regard to subsequent production of testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) [41, 44]. Huang et al. [45] found significantly elevated LH responses to GnRH in a subgroup of participants with SCI compared with controls; 53% (16 of 30) of participants with SCI had exaggerated LH responses and 20% (6 of 30) of participants had elevated FSH responses. The apparent discrepancies among the reports could, at least in part, be attributed to varying factors in subject selection, including health and nutrition parameters, medication effects, and level and duration of injury effects, or, simply to differences in methodology employed for provocative stimulation.
Provocative testing of the pituitary with GnRH is, by convention, performed at a standard dose. However, depending on the pathophysiology, it may be hypothesized that more subtle forms of hypothalamic–pituitary–gonadal axis dysfunction may be unmasked by the administration of GnRH doses that are lower than those conventionally employed and, thereby, permitting better differentiation between the hypogonadal and eugonadal status or, possibly, SCI and able-bodied individuals. As such, this study was designed to evaluate the integrity of the hypothalamic–pituitary–gonadal axis in hypogonadal and eugonadal men with SCI and able-bodied controls of a similar gonadal status by provocative stimulation of the pituitary with GnRH at three doses: the conventional dose level (100 μg) and two lower doses (10 and 50 μg).
Methods
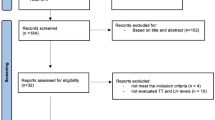
Study cohort
Participants were recruited from the James J. Peters VA Medical Center (JJPVAMC), Bronx, NY, and the Kessler Institute of Rehabilitation (KIR), West Orange, NJ. Otherwise, healthy men between the ages of 18 and 65 with chronic SCI (duration of injury > 1 year) who were assumed to have normal, sexual, and hypothalamic–pituitary–testicular function prior to injury or neurologically intact able-bodied men were considered for eligibility. The exclusion criteria included the following conditions: acute illness; active thyroid disease; medications for depression, mood changes, or any nervous condition; centrally acting high-blood-pressure medications (i.e., guanethidine, reserpine, methyldopa, β-adrenergic blockers, clonidine, etc.); medications for gastrointestinal disorders; medication for heart disease; medications for seizures (i.e., phenytoin or barbiturates); epilepsy; congestive heart failure; anticancer medications; antibiotics; pain medications; hormones (other than replacement doses); history of pituitary or testicular surgery; or less than 18 or older than 65 years of age. Abstinence from alcohol-containing beverages was required for 48 h before performing the study procedures.
Procedures
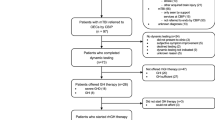
This was a prospective, open-label, randomized, and parallel group investigation to differentiate between normal and abnormal pituitary function in persons with SCI. Stimulation tests were performed to test the pituitary function with GnRH to assess the release of gonadotropins (LH, FSH). Three doses of GnRH (e.g., 10, 50, or 100 µg) were administered on separate days in a random order (Fig. 1). For each stimulation test, a dose-response curve was obtained from serial blood draws that were collected between 0800 and 0900 hours for the determination of plasma FSH and LH; serum concentrations of T were obtained for the determination of a hypogonadal or eugonadal status [46–48]. The GnRH stimulation test was performed on each subject in three visits on nonconsecutive days over several weeks. For the GnRH stimulation test, an intravenous line was placed in an antecubital vein for serial blood draws in heparinized tubes at time 0, and 15, 30, 60, 120, and 180 min following stimulation. Blood samples were centrifuged, plasma was separated from formed blood cell elements, and the plasma was frozen at −20 °C before hormone determination for serum T, plasma LH, and FSH concentrations.
Laboratory analysis
The serum T concentration was determined in duplicate by radioimmunoassay, in accordance with the manufacturer’s guidelines (ICN Biomedicals, Inc., Costa Mesa, CA). The sensitivity for T assay was 0.08 ng/ml; the intra-assay coefficient of variation (CV) were 9.6%, 8.1%, and 7.8% for T concentrations of 0.9, 7.0, and 20 ng/ml, respectively; the inter-assay CV were 8.6%, 9.1%, and 8.4% for T concentrations of 0.7, 6.0, and 16 ng/ml, respectively; and the two SD normal range for adult males is 2.8–8.8 ng/ml. Plasma FSH and LH levels were determined in duplicate by an immunoradiometric assay (Siemens Medical Solutions Diagnostics, Los Angeles, CA). The sensitivity for the FSH assay was 0.06 mIU/ml; the intra-assay CV were 3.8%, 2.4%, and 3.8% for FSH concentrations of 1.6, 10, and 73 mIU/ml, respectively; the inter-assay CV were 5.7%, 4.0%, and 5.0% for FSH concentrations of 4.6, 11, and 38 mIU/ml, respectively; and the 95% range for adult males is 1.1–13.5 mIU/ml. The sensitivity of the LH assay was 0.15 mIU/ml; the inter-assay CV were 1.6%, 1.2%, and 1.0% for LH concentrations of 9, 16, and 22 mIU/ml, respectively; the inter-assay CV were 7.1%, 2.6%, and 3.4% for LH concentrations of 2, 9, and 24 mIU/ml, respectively; and the 95% range for adult males is 0.4–5.7 mIU/ml.
Statistical analyses
To characterize subgroup responses, independent variables for neurological injury (SCI vs. AB) and gonadal status (hypogonadal (HG) vs. eugonadal (EG)) were concatenated to produce four categorical groups (Able-Bodied Eugonadal (AB-EG); Able-Bodied Hypogonadal (AB-HG); SCI-Eugonadal (SCI-EG); and SCI-Hypogonadal (SCI-HG)). Separate factorial analysis of variance (ANOVA) was performed to identify group differences for demographic (age, height, weight, BMI, and DOI) and baseline laboratory values at each study visit (T, LH, and FSH). Separate single-factor (GnRH dose) ANOVA was performed within each group (AB-EG, AB-HG, SCI-EG, and SCI-HG) to determine if baseline (Time 0) concentrations of FSH or LH were different. The values are expressed as group mean ± SD.
For each GnRH dose (10, 50, or 100 µg), a separate single factor (concatenated group: AB-EG; AB-HG; SCI-EG; and SCI-HG) mixed-model ANOVA with repeated measures on time (0, 15, 30, 60, 120, and 180 min) was performed to identify significant differences in the respective hormone concentrations. Significant time main effects were explored using pairwise comparisons within each model. To facilitate a more inclusive analysis of significant interaction effects within each GnRH dose, the area under the curve (AUC; integrated response) was calculated using GraphPad software (Prism 6.0, La Jolla, CA) for each group’s FSH and LH response. AUC was calculated as the sum of the rise above the baseline value for each time point and group. The effects of increasing the dose on the total stimulated responses were analyzed using a single-factor (concatenated group: AB-EG; AB-HG; SCI-EG; and SCI-HG) ANOVA with repeated measures on dose (10, 50, or 100 µg). Bonferroni’s post-hoc tests were performed to identify group differences to the respective doses.
To evaluate the efficacy of each stimulation dose to produce a standard gonadotropin response, the respective subject responses (e.g., time) to each stimulation dose for FSH and LH were characterized as a binary categorical variable (e.g., “responder” or “nonresponder”) based on whether a greater than two-fold increase in the plasma LH level and a greater than 50% increase in the plasma FSH level from the baseline concentration were achieved [49]. Chi-square analyses were performed to identify group differences for the percentage of responders at each time point and stimulation dose. Chi-square analyses were then performed to identify the percentage of participants who achieved a positive FSH and LH response to the respective doses at each time point (e.g., diagnostic agreement). With a consideration for the standard clinical blood collection times (e.g., 30 and 60 min post-stimulation injection) [49], chi-square analyses were performed to identify the percentage of responders at the 30- and 60-minute time points at the standard dose (100 µg) and middle dose (50 µg). An a priori level of significance was set at p ≤ 0.05. Statistical analyses were completed using IBM SPSS Statistics 21 (IBM, Armonk, NY, USA).
Statement of ethics
The research protocol was approved by the Institutional Review Boards of the James J. Peters Veterans Affairs Medical Center and the Kessler Foundation. Written informed consent was obtained from each subject before study participation. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Demographic information and baseline blood values
Demographic data for participants and baseline gonadotropin values in the AB-EG, AB-HG, SCI-EG, and SCI-HG groups are provided (Table 1). The groups were well matched for demographic characteristics and there were no differences in the distribution in the SCI subgroups for the proportion of individuals with paraplegia or tetraplegia. The statistical differences for baseline serum T values (p < 0.0001) for gonadal status (HG vs. EG) in the SCI and AB groups were provided by the study design. The mean plasma FSH and LH concentrations for the baseline visits are provided before the administration of GnRH. With the exception of the baseline visit for the plasma FSH concentrations before the administration of GnRH at 100 µg, the other FSH and LH values were not significantly different between the EG and HG groups. Within each group, the respective plasma FSH or LH concentrations for each study visit were not statistically different at the baseline blood collection. The mean plasma FSH (normal range: 0.9–15.0 mIU/ml) and LH (normal range: 1.3–13.0) concentrations for all groups were within the normal ranges for adult males.
GnRH provocative stimulation
Provocative testing with GnRH was performed at 3 concentrations (i.e., 10, 50, and 100 µg). Significant group main effects were not observed for plasma’s FSH or LH responses at any dose. However, significant time main effects were observed for plasma’s FSH or LH responses at each dose (Fig. 2), indicating that the respective stimulations produced a change in the corresponding hormone concentration. Post-hoc analyses revealed that FSH and LH concentrations at each time point after administration of the GnRH doses were significantly greater (p < 0.05) than their respective baseline concentration (Time 0). After administration of GnRH at 50 and 100 µg for FSH, the 30-, 60-, and 120-min postinjection time point concentrations were also significantly greater than the 15-min time point concentration (p < 0.01, Fig. 2). After the administration of GnRH at 50 and 100 µg, the 30-min post-GnRH time point for LH was the only one that was significantly greater than the 15-min time point (p < 0.01, Fig. 2). A significant group×time interaction effect was observed after the administration of GnRH at 50 µg for FSH and was observed after the administration of GnRH at 50 and 100 µg for LH.
Gonadotropin responses to GnRH stimulation at 3 doses by a group. The results from the omnibus-repeated measures analysis of variance for each GnRH dose and gonadotropin (e.g., FSH and LH) are provided as group, time, or interaction effects in the top-right portion of the corresponding plot. Time main effects were explored using Bonferroni’s post-hoc tests and significant increases from Time 0 or Time 15 to a later time point in all groups were also explored. FSH and LH concentrations at each time point after administration of the GnRH doses were significantly greater (p < 0.05) than their respective baseline concentration (Time 0). After the administration of GnRH at 50 and 100 µg for FSH, the 30-, 60-, and 120-minute postinjection time point concentrations were also significantly greater than the 15-minute time point concentration (p < 0.01, Fig. 2). After the administration of GnRH at 50 and 100 µg doses, the 30-minute post-GnRH time point for LH was the only one that was significantly greater than the 15-minute time point (p < 0.01, Fig. 2). NS: not significant; AB-EG: able-bodied eugonadal; AB-HG: able-bodied hypogonadal; SCI-EG: spinal cord injury eugonadal; and SCI-HG: spinal cord injury hypogonadal. Note that the response of the gonadotropins to stimulation was observably higher in the SCI groups compared with the AB groups, regardless of the dose of GnRH administered. Standard-deviation bars are redacted from the figure to enhance visualization, and are provided below: 
Analyses for the area under the curve responses to graded GnRH stimulation
Within each dose, the omnibus model to test for group differences was significant for FSH at the 10 and 50 µg (p < 0.05, respectively) and 100 µg (p < 0.001) doses (Fig. 3); post-hoc analyses failed to reveal the presence of any subgroup differences. However, at 100 µg, the integrated FSH response in the SCI-HG group was significantly greater than the response in the AB-HG group (*p < 0.01) and trending toward a significant difference compared with the AB-EG group († p = 0.07) (Fig. 3). Within each group, no statistical differences demonstrated an increasing dose effect on the FSH responses to stimulation. For LH, the within-dose group comparisons were not statistically significant after the administration of GnRH at 10 or 100 µg, but did achieve a significance after the administration of GnRH at 50 µg (p < 0.01); post-hoc analyses revealed that the integrated LH response in the SCI-EG group was significantly greater than the response in the AB-HG group (*p < 0.01) and trending toward a significant difference compared with the AB-EG group († p = 0.07) (Fig. 3). Within each group, a statistically significant dose effect on the integrated LH responses was observed for the AB-EG and SCI-EG (p < 0.05) groups, but not for the SCI-HG and AB-HG groups that approached a significance. The SCI-EG and AB-EG groups had significantly greater integrated LH responses after the administration of GnRH at 50 and 100 µg, respectively, compared with GnRH at 10 µg (‡ p < 0.05).
FSH and LH area under the curve responses by the dose of GnRH (e.g., 10 µg, 50 µg, and 100 µg). The results are provided from the omnibus model to determine the presence of significant group differences within each GnRH dose for FSH (top panel) and LH (bottom panel). The dose of GnRH administered is provided beneath each set of bars. Post-hoc tests that revealed the presence of significant group differences within each dose and hormone (e.g., FSH or LH) are provided with brackets and the corresponding level of significance is also provided (*p < 0.01, † p = 0.07). The results from the omnibus model to determine the presence of significant AUC responses to GnRH dose within the group are labeled beneath the FSH (top panel) and LH (bottom panel) graphical presentations. Post-hoc tests revealing the presence of significant increases in AUC responses for LH are provided on the corresponding bar, against which the change occurred compared with the 10 µg dose (‡ p < 0.05). NS not significant, AB-EG able-bodied eugonadal, AB-HG able-bodied hypogonadal, SCI-EG spinal cord injury eugonadal, and SCI-HG spinal cord injury hypogonadal
Clinically significant responses to GnRH dose stimulation
Within each GnRH dose (10, 50, and 100 µg) and time point (15, 30, 60, 120, and 180 min), chi-square analyses were performed to determine if the groups (e.g., AB-EG, AB-HG, SCI-EG, and SCI-HG) differed in the proportion of individuals who achieved a clinically acceptable FSH or LH response (Table 2). For all doses and time points, there were no significant differences in the proportion of responders among groups. When categorizing individuals by whether or not they achieved acceptable clinical responses for both FSH and LH at the respective time points within each dose, the groups did not differ on the proportion of a diagnostic agreement for gonadotropins. In comparing the effect of increasing GnRH dose at specific time points (e.g., 30 and 60 min) within each group, chi-square analyses revealed that a diagnostic agreement for an acceptable clinical response at the 30 or 60 min time points after the administration of GnRH at 50 vs. 100 µg were not significantly different for the proportion of clinically acceptable responses for both gonadotropins among the groups, except for the AB-HG group that had a greater diagnostic agreement after the administration of GnRH at 50 µg compared with GnRH at 100 µg. There did not appear to be any indication that age, body mass, level of injury, or duration of SCI contributed to these findings.
Discussion
The question could be raised as to whether individuals with SCI have a more subtle abnormality in central regulation that may be unmasked by a nuanced approach to provocative testing of the hypothalamic–pituitary axis with GnRH. Provocative stimulation of the hypothalamic–pituitary axis with conventional and lower doses of GnRH revealed novel and potentially clinically significant findings in persons with SCI. This work adds further evidence to support the concept that there is central dysfunction in the regulation of the hypothalamic–pituitary axis in persons with SCI because of the heightened pituitary sensitivity to GnRH, regardless of gonadal status. Compared with the AB controls, a greater integrated FSH response in the SCI-HG group after stimulation with GnRH at 100 µg and a greater integrated LH response in the SCI-EG group after stimulation with GnRH at 50 µg suggests that hypothalamic GnRH may be globally depressed in persons with SCI. The current study also revealed that a similar percentage of respondents achieved the clinically acceptable responses of circulating FSH or LH after GnRH stimulation at the standard postinjection collection time points (e.g., 30 and 60 min), regardless of gonadal status. Similarly, the agreement in identifying individuals with acceptable dual gonadotropin responses—that is, FSH or LH responses achieved to the same dose of GnRH that met the clinical criteria of “normal”—was inconsistent, and without regard to GnRH dose or time of blood collection; however, the highest agreement in obtaining an acceptable gonadotropin response to stimulation was observed after the administration of GnRH at 50 µg.
In a prior study, about 75% of the participants in the SCI group, and a similar percent in the AB group, had a clinically acceptable gonadotropin response to standard provocative GnRH pituitary stimulation (“responders”) [18]. Of note, the SCI responder group had a significantly increased FSH release at several time points compared with the AB responder group; the average and integrated LH release in the SCI responder group approached significance compared with that of the AB-responder group [18]. Because serum T responses to standard hCG stimulation testing were not significantly different for able-bodied or SCI men, regardless of gonadal status, it was suggested that the preponderance of hypogonadism identified in men with SCI is probably associated with hypothalamic–pituitary dysfunction, and not with end-organ failure [19].
While not significant, possibly in part due to the relatively small group sizes, the stimulated absolute mean FSH responses in those with SCI, regardless of gonadal status, were consistently higher than those of the AB groups (Fig. 2), especially after the administration of GnRH at 100 µg (Fig. 3, top). Although not as striking, the stimulated absolute mean LH responses in those with SCI, regardless of gonadal status, were consistently higher than those of the able-bodied groups (Fig. 1), especially after the administration of GnRH at 50 µg (Fig. 3, bottom). One must be cautious not to overstate the importance of this observation in the absence of a statistical difference, but it is tempting to recognize this finding because it was consistent throughout the entire range of GnRH doses administered and regardless of gonadal status in the SCI groups. If one were to speculate, this absolutely higher gonadotropin response to exogenous GnRH may suggest a central GnRH deficiency.
The possible etiologies for the observed dysfunction of hypothalamic–pituitary–gonadal axis may include, but are not limited to, the following considerations. The feedback loop between the periphery (e.g., testis) and central organs (e.g., hypothalamus and/or pituitary) may be disrupted due to the interruption of spinal circuits and/or altered hormonal feedback mechanisms, resulting in perturbed regulation of the axis. Inhibin B, a gonadal peptide, acts to suppress FSH release [50–52]. By severing the nervous innervation to the testes, it may be postulated that normal diurnal patterns for the release and circulation of testosterone and/or inhibin may be perturbed, resulting in altered gonadotropin release [53, 54]. Another possibility is that prescribed or illicit medications, such as psychotropic agents that elevate prolactin levels and/or opioids that suppress LH-releasing factor, may impair central function [23–26, 28, 55–57].
Schally et al. isolated a porcine pituitary peptide that, if injected into animals or humans, caused a rise in serum LH and FSH concentrations [58]. After this discovery, the majority of the studies that lead to the acceptance of the conventional dose of GnRH for the provocative stimulation of the hypothalamic–pituitary axis were carried out in the 1970s when GnRH (or, as then referred to, luteinizing hormone releasing hormone (LHRH)) initially became available to the investigators. The original work established the preferred route of delivery (intravenous vs. intramuscular vs. subcutaneous bolus administration) [59–61] and the dose of GnRH for the optimum response for routine clinical testing [62–65]. Wollesen et al. administered a wide dosage range of GnRH (0–3000 µg) to 16 healthy men to determine the pituitary gonadotropin release to dose and time after administration [62]; the smallest dose of GnRH that resulted in a significant response from normal saline administration was 1.58 µg for LH and 20 µg for FSH, with the maximum response determined to be greater than 3000 µg; the authors recommended a 100 µg dose of GnRH with sample collection at 30 and 45 min after administration, which would capture both the peak LH and FSH responses, and put forth 95% confidence intervals in normal men for the gonadotropin responses: 400–800% of the mean baseline value for serum LH and 100–200% for serum FSH. de Kretser and colleagues [63] compared the 25–100 µg dose of GnRH and recommended the 100 µg dose because the rise in FSH was minimal or absent at the lower doses. Testing a GnRH dose range of 1.56–450 μg, Newton et al. [64] observed that GnRH at a dose of 100 μg produced a maximal response in the majority of healthy individuals. These investigators also administered GnRH to 96 female patients with secondary amenorrhea, 5 patients with primary amenorrhea, and 8 patients with pituitary disorders and concluded that the magnitude and duration of the pituitary response was not of additional diagnostic value [64]. In an effort to identify the “appropriate dose” of GnRH, Schonau-Jorgensen et al. intramuscularly administered GnRH at 50, 100, and 200 µg and determined serum gonadotropin concentrations sequentially, and found that the 200 µg dose delivered intramuscularly was equivalent to the 100 µg dose delivered intravenously [65].
Patients in the general population with idiopathic oligozoospermia have been reported to have basal levels of LH that are within the normal range. Of note, in the work presented, the basal LH levels were in the normal range in participants with SCI. Thus, because it is well appreciated that a proportion of persons with SCI have been reported to have reduced sperm counts due to several possible etiologies [15, 43], a combined peripheral and central abnormality cannot be excluded at least in a subgroup of those with SCI.
The unique approach of our incremental GnRH stimulation protocol has provided provocative observations on the sensitivity of the pituitary and the time course of gonadotropin responses. The apparent heightened absolute release of FSH to standard GnRH stimulation in men with SCI who were HG, as well as the heightened release of LH in EG men with SCI, was also observed. These observations suggest the central dysregulation of the hypothalamic–pituitary axis in men with SCI, despite basal and conventionally stimulated plasma gonadotropin levels within the normal range, and regardless of serum testosterone levels [8, 16, 41].
Limitations
The major limitation of this work is the relatively small number of participants in each of the four sample groups. It is tempting to hypothesize that a study with more participants in each of our four subgroups may have yielded additional findings that would have reached significance. Our study group comprised of community-dwelling individuals who may have had chronic medical conditions requiring outpatient management. The nutritional status, alcohol consumption, and/or opioid usage were not specifically evaluated, although pain medications were an exclusion criterion for study participation. The likelihood for clinically significant malnutrition was low, but in subsets of our participants, excessive chronic alcohol consumption or opioid use may have contributed to the presence of the central dysregulation of the hypothalamic–pituitary function. However, every effort was made to exclude individuals with known medical conditions that could confound the results of this study.
Conclusion
Our findings demonstrate that graded stimulation of the hypothalamic–pituitary axis with three doses of GnRH (10, 50, and 100 µg) was shown to have a modest dose-response effect. Individuals with SCI who had HG and EG status had a similar percentage of clinically acceptable gonadotropin responses to the administration of GnRH at 50 and 100 µg. The standard dose of GnRH (100 μg) stimulated the greatest FSH response in the SCI-HG group, which may be an important clinical feature if the individual is being evaluated for infertility, while GnRH at 50 or 100 μg was equally potent to a stimulated LH release in the SCI-HG group. The higher integrated FSH response to GnRH at 100 μg in the SCI-HG group and the higher integrated LH response in the SCI-EG group to GnRH at 50 μg, in association with an increased gonadotropin release at all GnRH doses in SCI compared with AB groups, albeit this latter observation was not significant, is a further evidence to support the presence of a hypothalamic–pituitary dysfunction in persons with SCI. Even a subtle dysfunction of the hypothalamic–pituitary–gonadal axis may be associated with reduced circulating levels of testosterone and predisposition to adverse body composition and accompanying metabolic changes, as well as the potential undesirable effects on the psyche and deleterious effects on spermatogenesis. Thus, screening of the serum testosterone concentration should be performed on a regular and routine basis in persons with SCI with the consideration of initiating hormone replacement therapy in those with low values and no contraindications to this intervention.
Data archiving
All relevant data are within this manuscript and raw data are archived by the authors.
References
Sedlock DA, Laventure SJ. Body composition and resting energy expenditure in long term spinal cord injury. Paraplegia. 1990;28:448–54.
Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371–8.
Bauman WA, La Fountaine MF, Spungen AM. Age-related prevalence of low testosterone in men with spinal cord injury. J Spinal Cord Med. 2014;37:32–39.
Bauman WA, Spungen AM. Body composition in aging: adverse changes in able-bodied persons and in those with spinal cord injury. Top Spinal Cord Inj Rehabil. 2001;6:22–36.
Kocina P. Body composition of spinal cord injured adults. Sports Med. 1997;23:48–60.
Spungen AM, Bauman WA, Wang J, Pierson RN Jr. The relationship between total body potassium and resting energy expenditure in individuals with paraplegia. Arch Phys Med Rehabil. 1993;74:965–8.
Bauman WA, Spungen AM, Flanagan S, Zhong YG, Alexander LR, Tsitouras PD. Blunted growth hormone response to intravenous arginine in subjects with a spinal cord injury. Horm Metab Res. 1994;26:152–6.
Wang YH, Huang TS, Lien IN. Hormone changes in men with spinal cord injuries. Am J Phys Med Rehabil. 1992;71:328–32.
Bauman WA, Spungen AM. Metabolic changes in persons after spinal cord injury. Phys Med Rehabil Clin N Am. 2000;11:109–40.
Schopp LH, Clark M, Mazurek MO, Hagglund KJ, Acuff ME, Sherman AK, et al. Testosterone levels among men with spinal cord injury admitted to inpatient rehabilitation. Am J Phys Med Rehabil. 2006;85:678–84; quiz 685–677.
Clark MJ, Schopp LH, Mazurek MO, Zaniletti I, Lammy AB, Martin TA, et al. Testosterone levels among men with spinal cord injury: relationship between time since injury and laboratory values. Am J Phys Med Rehabil. 2008;87:758–67.
Burris AS, Banks SM, Carter CS, Davidson JM, Sherins RJ. A long-term, prospective study of the physiologic and behavioral effects of hormone replacement in untreated hypogonadal men. J Androl. 1992;13:297–304.
Corona G, Rastrelli G, Vignozzi L, Mannucci E, Maggi M. How to recognize late-onset hypogonadism in men with sexual dysfunction. Asian J Androl. 2012;14:251–9.
Khera M. Patients with testosterone deficit syndrome and depression. Arch Esp Urol. 2013;66:729–36.
Linsenmeyer TA, Perkash I. Infertility in men with spinal cord injury. Arch Phys Med Rehabil. 1991;72:747–54.
Kikuchi TA, Skowsky WR, El-Toraei I, Swerdloff R. The pituitary-gonadal axis in spinal cord injury. Fertil Steril. 1976;27:1142–5.
Cortes-Gallegos V, Castaneda G, Alonso R, Arellano H, Cervantes C, Parra A. Diurnal variations of pituitary and testicular hormones in paraplegic men. Arch Androl. 1982;8:221–6.
Bauman WA, La Fountaine MF, Cirnigliaro CM, Kirshblum SC, Spungen AM. Provocative stimulation of the hypothalamic-pituitary-testicular axis in men with spinal cord injury. Spinal Cord. 2016;54:961–6.
Bauman WA, La Fountaine MF, Cirnigliaro CM, Kirshblum SC, Spungen AM. Testicular responses to hCG stimulation at varying doses in men with spinal cord injury. Spinal Cord. 2017;55:659–63.
Durga A, Sepahpanah F, Regozzi M, Hastings J, Crane DA. Prevalence of testosterone deficiency after spinal cord injury. PMR. 2011;3:929–32.
Grossmann M, Matsumoto AM. A perspective on middle-aged and older men with functional hypogonadism: focus on holistic management. J Clin Endocrinol Metab. 2017;102:1067–75.
Bergendahl M, Veldhuis JD. Altered pulsatile gonadotropin signaling in nutritional deficiency in the male. Trends Endocrinol Metab. 1995;6:145–59.
Aloisi AM, Aurilio C, Bachiocco V, Biasi G, Fiorenzani P, Pace MC, et al. Endocrine consequences of opioid therapy. Psychoneuroendocrinology. 2009;34(Suppl 1):S162–S168.
Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002;3:377–84.
Pfeiffer A, Herz A. Endocrine actions of opioids. Horm Metab Res. 1984;16:386–97.
Raap DK, Van de Kar LD. Selective serotonin reuptake inhibitors and neuroendocrine function. Life Sci. 1999;65:1217–35.
Noth RH, Walter RM Jr. The effects of alcohol on the endocrine system. Med Clin N Am. 1984;68:133–46.
Bannister P, Losowsky MS. Ethanol and hypogonadism. Alcohol Alcohol. 1987;22:213–7.
Sullivan SD, Nash MS, Tefera E, Tinsley E, Blackman MR, Groah S. Prevalence and etiology of hypogonadism in young men with chronic spinal cord injury: a cross-sectional analysis from two University-Based rehabilitation centers. PMR. 2017;9:751–760.
Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:749–56.
Bauman WA, Adkins RH, Spungen AM, Kemp BJ, Waters RL. The effect of residual neurological deficit on serum lipoproteins in individuals with chronic spinal cord injury. Spinal Cord. 1998;36:13–17.
Stanworth RD, Jones TH. Testosterone in obesity, metabolic syndrome and type 2 diabetes. Front Horm Res. 2009;37:74–90.
Traish AM. Testosterone and weight loss: the evidence. Curr Opin Endocrinol Diabetes Obes. 2014;21:313–22.
Bauman WA, Spungen AM, Zhong YG, Rothstein JL, Petry C, Gordon SK. Depressed serum high density lipoprotein cholesterol levels in veterans with spinal cord injury. Paraplegia. 1992;30:697–703.
Monroe AK, Dobs AS. The effect of androgens on lipids. Curr Opin Endocrinol Diabetes Obes. 2013;20:132–9.
Bauman WA, Cirnigliaro CM, La Fountaine MF, Jensen AM, Wecht JM, Kirshblum SC, et al. A small-scale clinical trial to determine the safety and efficacy of testosterone replacement therapy in hypogonadal men with spinal cord injury. Horm Metab Res. 2011;43:574–9.
Wade GN. Sex steroids and energy balance: sites and mechanisms of action. Ann N Y Acad Sci. 1986;474:389–99.
Munro D, Horne HW Jr, Paull DP. The effect of injury to the spinal cord and cauda equina on the sexual potency of men. N Engl J Med. 1948;239:903–11.
Horne HW, Paull DP, Munro D. Fertility studies in the human male with traumatic injuries of the spinal cord and cauda equina. N Engl J Med. 1948;239:959–61.
Bors E, Engle ET, Rosenquist RC, Holliger VH. Fertility in paraplegic males; a preliminary report of endocrine studies. J Clin Endocrinol Metab. 1950;10:381–98.
Ver Voort SM. Infertility in spinal-cord injured male. Urology. 1987;29:157–65.
Beretta G, Chelo E, Zanollo A. Reproductive aspects in spinal cord injured males. Paraplegia. 1989;27:113–8.
Perkash I, Martin DE, Warner H, Blank MS, Collins DC. Reproductive biology of paraplegics: results of semen collection, testicular biopsy and serum hormone evaluation. J Urol. 1985;134:284–8.
Nance PW, Shears AH, Givner ML, Nance DM. Gonadal regulation in men with flaccid paraplegia. Arch Phys Med Rehabil. 1985;66:757–9.
Huang TS, Wang YH, Chiang HS, Lien YN. Pituitary-testicular and pituitary-thyroid axes in spinal cord-injured males. Metabolism. 1993;42:516–21.
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536–59.
Winters SJ. Diurnal rhythm of testosterone and luteinizing hormone in hypogonadal men. J Androl. 1991;12:185–90.
Gupta SK, Lindemulder EA, Sathyan G. Modeling of circadian testosterone in healthy men and hypogonadal men. J Clin Pharmacol. 2000;40:731–8.
Bhasin S, Jameson JL. Disorders of the testes and male reproductive system. In: Braunwald E, Fauci AS, Hauser SL, Kasper DL, Jameson JL, Longo DL (eds). Harrison’s Principles of Internal Medicine. New York: McGraw-Hill Education, 2005, pp. 2188.
Gregory SJ, Kaiser UB. Regulation of gonadotropins by inhibin and activin. Semin Reprod Med. 2004;22:253–67.
Bilezikjian LM, Blount AL, Donaldson CJ, Vale WW. Pituitary actions of ligands of the TGF-beta family: activins and inhibins. Reproduction. 2006;132:207–15.
Iliadou PK, Tsametis C, Kaprara A, Papadimas I, Goulis DG. The Sertoli cell: novel clinical potentiality. Hormones. 2015;14:504–14.
Tenover JS, Bremner WJ. Circadian rhythm of serum immunoreactive inhibin in young and elderly men. J Gerontol. 1991;46:M181–184.
Chong YH, Pankhurst MW, McLennan IS. The daily profiles of circulating AMH and INSL3 in men are distinct from the other testicular hormones, inhibin B and testosterone. PLoS ONE. 2015;10:e0133637.
Ajmal A, Joffe H, Nachtigall LB. Psychotropic-induced hyperprolactinemia: a clinical review. Psychosomatics. 2014;55:29–36.
Brennan MJ. The effect of opioid therapy on endocrine function. Am J Med. 2013;126(Suppl 1):S12–S18.
Schooling CM, Au Yeung SL, Freeman G, Cowling BJ. The effect of statins on testosterone in men and women, a systematic review and meta-analysis of randomized controlled trials. BMC Med. 2013;11:57.
Schally AV, Arimura A, Baba Y, Nair RM, Matsuo H, Redding TW, et al. Isolation and properties of the FSH and LH-releasing hormone. Biochem Biophys Res Commun. 1971;43:393–9.
Arimura A, Spies HG, Schally AV. Relative insensitivity of rhesus monkeys to the LH-releasing hormone (LH-RH). J Clin Endocrinol Metab. 1973;36:372–4.
Redding TW, Kastin AJ, Gonzales-Barcena D, Coy DH, Coy EJ, Schalch DS, et al. The half-life, metabolism and excretion of tritiated luteinizing hormone-releasing hormone (LH-RH) in man. J Clin Endocrinol Metab. 1973;37:626–31.
Mortimer CH, Besser GM, Goldie DJ, Hook J, McNeilly AS. The TSH, FSH and prolactin responses to continuous infusions of TRH and the effects of oestrogen administration in normal males. Clin Endocrinol. 1974;3:97–103.
Wollesen F, Swerdloff RS, Odell WD. LH and FSH responses to luteinizing releasing hormone in normal fertile women. Metabolism. 1976;25:1275–85.
de Kretser DM, Burger HG, Hudson BK. The pituitary-testicular response to luteinising hormone releasing hormone administration to normal men. Aust N Z J Med. 1975;5:227–30.
Newton JR, Kilpatrick MJ, Pike JM, Collins WP. An evaluation of the diagnostic value of synthetic luteinizing hormone releasing hormone. Acta Endocrinol. 1975;80:417–28.
Schonau-Jorgensen F, Kampmann JP, Micic S, Roos J, Johnsen SG. LH and FSH in serum after intramuscular administration of LH/FSH-releasing hormone in normal and hypogonadal men. Acta Endocrinol. 1975;78:1–10.
Acknowledgements
The research reported in this article was supported by the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research, and Development Service. This work was funded by the Veteran Affairs Rehabilitation Research & Development National Center of Excellence for the Medical Consequences of Spinal Cord Injury (B2648-C, B4162-C and B9212-C, and B2020-C). We wish to thank the James J Peters Veterans Affairs Medical Center, Bronx, NY, and the Kessler Institute for Rehabilitation, West Orange, NJ, for their support. Grant Sources: Veteran Affairs Rehabilitation Research and Development Service (#B2468-C, #B4162-C, #B9212-C, and #B2020-C) and the James J Peters VA Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bauman, W.A., La Fountaine, M.F., Cirnigliaro, C.M. et al. Administration of increasing doses of gonadotropin-releasing hormone in men with spinal cord injury to investigate dysfunction of the hypothalamic–pituitary–gonadal axis. Spinal Cord 56, 247–258 (2018). https://doi.org/10.1038/s41393-017-0002-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-017-0002-x
This article is cited by
-
Cannabis shenanigans: advocating for the restoration of an effective treatment of pain following spinal cord injury
Spinal Cord Series and Cases (2018)