Abstract
Background
Outcomes of radical prostatectomy (RP) in men with history of lower urinary tract symptoms related to benign prostatic enlargement (LUTS/BPE) surgery represents a controversial issue. We performed an updated systematic review and meta- analysis evaluating oncological and functional outcomes of RP in this subset of patients.
Methods
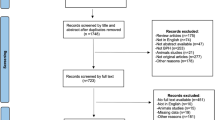
Eligible studies were identified from MEDLINE, Web of Science and the Scopus databases. The following outcomes were evaluated: incidence of positive surgical margins (PSM), incidence of biochemical recurrence (BCR), 3-mo and 1-year urinary continence (UC) rates, incidence of nerve-sparing (NS) procedures, 1-year erectile function (EF) recovery rates. We estimated pooled Odds ratios (OR) and 95% confidence intervals (CI) using random effects models. Sub-analyses were performed according to the type of RP and LUTS/BPE surgery.
Results
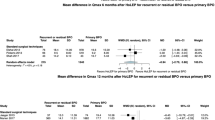
Twenty-five retrospective studies including 11,101 patients undergoing RP were included in the analysis (2113 with history of LUTS/BPE surgery, and 8898 controls). PSM rate was significantly higher in patients with history of LUTS/BPE surgery (OR 1.39, 95% CI 1.18–1.63, p < 0.001). No statistically significant difference in terms of BCR emerged between patients with or without history of LUTS/BPE surgery (OR 1.46, 95% CI 0.97–2.18, p = 0.066). Three-months and 1-year UC rates were significantly lower in patients with previous LUTS/BPE surgery (OR 0.48, 95% CI 0.34–0.68, p < 0.001 and OR 0.44, 95% CI 0.31–0.62, p < 0.001; respectively). Although not statistically significant differences between the two groups emerged in terms of adoption of NS procedures (OR 0.59, 95% CI 0.32–1.12, p = 0.107), 1-year EF recovery was significantly lower in patients with history of LUTS/BPE procedures (OR 0.60, 95% CI 0.40–0.89, p = 0.010).
Conclusions
In conclusions, RP in patients with history of previous LUTS/BPE surgery is associated with increased incidence of PSM, lower UC rates at both 3-months and 1-year follow-up as well as lower rates of EF recovery at 1-year follow-up.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

















Similar content being viewed by others
References
Verze P, Califano G, Sokolakis I, Russo GI, Hatzichristodoulou G, Musi G, et al. EAU-YAU Men’s health working party. The impact of surgery for lower urinary tract symptoms/benign prostatic enlargement on both erectile and ejaculatory function: A systematic review. Int J Impot Res. 2019;31:319–27.
Fusco F, Creta M, De Nunzio C, Gacci M, Li Marzi V, Finazzi Agrò E. Alpha-1 adrenergic antagonists, 5-alpha reductase inhibitors, phosphodiesterase type 5 inhibitors, and phytotherapic compounds in men with lower urinary tract symptoms suggestive of benign prostatic obstruction: A systematic review and meta-analysis of urodynamic studies. Neurourol Urodyn. 2018;37:1865–74.
Arcaniolo D, Manfredi C, Veccia A, Herrmann TRW, Lima E, Mirone V, et al. EAU Section of Uro-Technology (ESUT) Research Group. Bipolar endoscopic enucleation versus bipolar transurethral resection of the prostate: an ESUT systematic review and cumulative analysis. World J Urol. 2020;38:1177–86.
Fernández-Pascual E, Manfredi C, Martín C, Martínez-Ballesteros C, Balmori C, Lledó-García E, et al. mpMRI-US Fusion-guided targeted cryotherapy in patients with primary localized prostate cancer: A prospective analysis of oncological and functional outcomes. Cancers (Basel) 2022;14:2988.
Manfredi C, Arcaniolo D, Spatafora P, Crocerossa F, Fusco F, Verze P, et al. Emerging minimally invasive transurethral treatments for benign prostatic hyperplasia: A systematic review with meta-analysis of functional outcomes and description of complications. Minerva Urol Nephrol. 2022;74:389–99.
Manfredi C, García-Gómez B, Arcaniolo D, García-Rojo E, Crocerossa F, Autorino R, et al. Impact of surgery for benign prostatic hyperplasia on sexual function: A systematic review and meta-analysis of erectile function and ejaculatory function. Eur Urol Focus. 2022;8:1711–32.
Yang Y, Luo Y, Hou GL, Huang QX, Lu MH, Si-tu J, et al. Laparoscopic radical prostatectomy after previous transurethral resection of the prostate in clinical T1a and T1b prostate cancer: A matched-pair analysis. Urol J. 2015;12:2154–9.
Stanzione A, Ponsiglione A, Cuocolo R, Cocozza S, Picchi SG, Stilo S, et al. Abbreviated protocols versus Multiparametric MRI for assessment of extraprostatic extension in prostatic carcinoma: A multireader study. Anticancer Res. 2019;39:4449–54.
Capogrosso P, Capitanio U, Vertosick EA, Ventimiglia E, Chierigo F, Oreggia D, et al. Temporal trend in incidental prostate cancer detection at surgery for benign prostatic hyperplasia. Urology. 2018;122:152–7.
Liao H, Duan X, Du Y, Mou X, Hu T, Cai T, et al. Radical prostatectomy after previous transurethral resection of the prostate: Oncological, surgical and functional outcomes-a meta-analysis. World J Urol. 2020;38:1919–32.
Guo Z, He J, Huang L, Wang Z, Hu P, Wang S, et al. Prevalence and risk factors of incidental prostate cancer in certain surgeries for benign prostatic hyperplasia: A systematic review and meta-analysis. Int Braz J Urol. 2022;48:915–29.
Veccia A, Antonelli A, Francavilla S, Porpiglia F, Simeone C, Lima E, et al. Minimally Invasive Radical Prostatectomy after Previous Bladder Outlet Surgery: A Systematic Review and Pooled Analysis of Comparative Studies. J Urol. 2019;202:511–7.
Li H, Zhao C, Liu P, Hu J, Yi Z, Chen J, et al. Radical prostatectomy after previous transurethral resection of the prostate: A systematic review and meta-analysis. Transl Androl Urol. 2019;8:712–27.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34.
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inf Decis Mak. 2007;7:16.
Durieux N, Vandenput S, Pasleau F. Médecine factuelle: la hiérarchisation des preuves par le Centre for Evidence-Based Medicine d’oOford [OCEBM levels of evidence system]. Rev Med Liege. 2013;68:644–9.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa scale: Comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Su YK, Katz BF, Sehgal SS, Yu SJ, Su YC, Lightfoot A, et al. Does previous transurethral prostate surgery affect oncologic and continence outcomes after RARP? J Robot Surg. 2015;9:291–7.
Zugor V, Labanaris AP, Porres D, Witt JH. Surgical, oncologic, and short-term functional outcomes in patients undergoing robot-assisted prostatectomy after previous transurethral resection of the prostate. J Endourol. 2012;26:515–9.
Tugcu V, Atar A, Sahin S, Kargi T, Gokhan Seker K, IlkerComez Y, et al. Robot-assisted radical prostatectomy after previous prostate surgery. JSLS. 2015;19:e2015.00080.
Yazici S, Inci K, Yuksel S, Bilen CY, Ozen H. Radical prostatectomy after previous prostate surgery: Effects on surgical difficulty and pathologic outcomes. Urology. 2009;73:856–9.
Verze P, Greco F, Scuzzarella S, Bottone F, Palmieri A, Cucchiara V, et al. The impact of previous prostate surgery on the outcomes of laparoscopic radical prostatectomy. Minerva Urol Nefrol. 2017;69:76–84.
Teber D, Cresswell J, Ates M, Erdogru T, Hruza M, Gözen AS, et al. Laparoscopic radical prostatectomy in clinical T1a and T1b prostate cancer: oncologic and functional outcomes–a matched-pair analysis. Urology. 2009;73:577–81.
Pompe RS, Leyh-Bannurah SR, Preisser F, Salomon G, Graefen M, Huland H, et al. Radical prostatectomy after previous TUR-P: Oncological, surgical, and functional outcomes. Urol Oncol. 2018;36:527.e21–527.e28.
Pastore AL, Palleschi G, Silvestri L, Leto A, Al-Rawashdah SF, Petrozza V, et al. Laparoscopic radical prostatectomy after previous transurethral resection of prostate using a catheter balloon inflated in prostatic urethra: Oncological and functional outcomes from a matched pair analysis. Int J Urol. 2015;22:1037–42.
Palisaar JR, Wenske S, Sommerer F, Hinkel A, Noldus J. Open radical retropubic prostatectomy gives favourable surgical and functional outcomes after transurethral resection of the prostate. BJU Int. 2009;104:611–5.
Menard J, de la Taille A, Hoznek A, Allory Y, Vordos D, Yiou R, et al. Laparoscopic radical prostatectomy after transurethral resection of the prostate: surgical and functional outcomes. Urology 2008;72:593–7.
Kretschmer A, Mazzone E, Barletta F, Leni R, Heidegger I, Tsaur I. et al. EAU-YAU Prostate Cancer Working Party. Initial experience with radical prostatectomy following Holmium laser enucleation of the prostate. Eur Urol Focus. 2021;7:1247–53.
Jin K, Qiu S, Liao XY, Zheng XN, Tu X, Tang LS, et al. Transurethral resection of the prostate is an independent risk factor for biochemical recurrence after radical prostatectomy for prostate cancer. Asian J Androl. 2020;22:217–21.
Jaffe J, Stakhovsky O, Cathelineau X, Barret E, Vallancien G, Rozet F. Surgical outcomes for men undergoing laparoscopic radical prostatectomy after transurethral resection of the prostate. J Urol. 2007;178:483–7.
Hung CF, Yang CK, Ou YC. Robotic assisted laparoscopic radical prostatectomy following transurethral resection of the prostate: perioperative, oncologic and functional outcomes. Prostate Int. 2014;2:82–9.
Hampton L, Nelson RA, Satterthwaite R, Wilson T, Crocitto L. Patients with prior TURP undergoing robot-assisted laparoscopic radical prostatectomy have higher positive surgical margin rates. J Robot Surg. 2008;2:213–6.
Gupta NP, Singh P, Nayyar R. Outcomes of robot-assisted radical prostatectomy in men with previous transurethral resection of prostate. BJU Int. 2011;108:1501–5.
Gellhaus PT, Monn MF, Leese J, Flack CK, Lingeman JE, Koch MO, et al. Robot-Assisted Radical Prostatectomy in Patients with a History of Holmium Laser Enucleation of the Prostate: Feasibility and Evaluation of Initial Outcomes. J Endourol. 2015;29:764–9.
Garg H, Seth A, Kumar R. Impact of previous transurethral resection of prostate on robot-assisted radical prostatectomy: A matched cohort analysis. J Robot Surg. 2022; 3. https://doi.org/10.1007/s11701-021-01348-8.
Eden CG, Richards AJ, Ooi J, Moon DA, Laczko I. Previous bladder outlet surgery does not affect medium-term outcomes after laparoscopic radical prostatectomy. BJU Int. 2007;99:399–402.
Colombo R, Naspro R, Salonia A, Montorsi F, Raber M, Suardi N, et al. Radical prostatectomy after previous prostate surgery: Clinical and functional outcomes. J Urol. 2006;176:2459–63.
Chaloupka M, Figura F, Weinhold P, Jokisch F, Westhofen T, Pfitzinger P, et al. Impact of previous transurethral prostate surgery on health-related quality of life after radical prostatectomy: Does the interval between surgeries matter? World J Urol. 2021;39:1431–8.
Carbin DD, Tamhankar AS, Ahluwalia P, Gautam G. Does prior transurethral resection of prostate affect the functional and oncological outcomes of robot-assisted radical prostatectomy? A matched-pair analysis. J Robot Surg. 2021 Nov 28. https://doi.org/10.1007/s11701-021-01339-9.
Leyh-Bannurah SR, Liakos N, Oelke M, Wagner C, Schuette A, Fangmeyer B, et al. Perioperative and postoperative outcomes of robot-assisted radical prostatectomy in prostate cancer patients with prior transurethral subvesical deobstruction: Results of a high-volume center. J Urol. 2021;206:308–18.
Abedali ZA, Calaway AC, Large T, Koch MO, Lingeman JE, Boris RS. Robot-assisted radical prostatectomy in patients with a history of Holmium Laser Enucleation of the Prostate: The Indiana University Experience. J Endourol. 2020;34:163–8.
Magheli A, Gonzalgo ML, Su LM, Guzzo TJ, Netto G, Humphreys EB, et al. Impact of surgical technique (open vs laparoscopic vs robotic-assisted) on pathological and biochemical outcomes following radical prostatectomy: An analysis using propensity score matching. BJU Int. 2011;107:1956–62.
Kim M, Yoo D, Pyo J, Cho W. Clinicopathological Significances of Positive Surgical Resection Margin after Radical Prostatectomy for Prostatic Cancers: A Meta-Analysis. Med (Kaunas). 2022;58:1251.
Stanford JL, Feng Z, Hamilton AS, Gilliland FD, Stephenson RA, Eley JW, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA 2000;283:354–60.
Pavlovich CP, Rocco B, Druskin SC, Davis JW. Urinary continence recovery after radical prostatectomy - anatomical/reconstructive and nerve-sparing techniques to improve outcomes. BJU Int. 2017;120:185–96.
EAU Guidelines. Edn. presented at the EAU Annual Congress Amsterdam (2022). ISBN 978-94-92671-16-5.
Author information
Authors and Affiliations
Contributions
Conceptualization, investigation, and supervision: MC and FF; results interpretation and writing: CM, DA; results interpretation: CDN, LS, VM, CI; contribution to an oversight of the overall study: SAK, HHW, PG, TB; review and editing: NL, MDS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Creta, M., Manfredi, C., Arcaniolo, D. et al. Functional and oncological outcomes after radical prostatectomy in patients with history of surgery for lower urinary tract symptoms related to benign prostatic enlargement: A systematic review with meta-analysis. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00678-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00678-y
This article is cited by
-
Impact of peritoneal reconfiguration on lymphocele formation after robot-assisted radical prostatectomy with pelvic lymph node dissection: a systematic review and meta-analysis of randomized controlled trials
Prostate Cancer and Prostatic Diseases (2023)
-
New robotic platforms for prostate surgery: the future is now
Prostate Cancer and Prostatic Diseases (2023)
-
Prostate Cancer in Transgender Women: Epidemiology, Clinical Characteristics, and Management Challenges
Current Oncology Reports (2023)