Abstract
Background
Shared decision-making (SDM) for metastatic prostate cancer (mPC) engages patients in the decision-making process and may be associated with better outcomes relative to physician- or patient-directed decision-making. We assessed the association between decision locus of control (DLOC) and patient-reported quality of life (QOL), functional outcomes, and decision satisfaction among mPC patients.
Methods
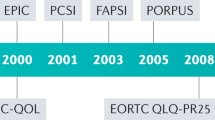
After a clinic visit in which a treatment decision was made (baseline), mPC patients completed DLOC and QOL surveys. QOL was re-assessed at 2- and 4-months post-baseline. Mean scores for each QOL dimension (physical, emotional, cognitive, social, and role functioning) were compared by DLOC group using mixed effects models. Patient preferences for DLOC and provider communication techniques were similarly collected via survey.
Results
Median age of participants (N = 101) was 69 years (range: 49-92); most were White (80%) and married (82%). 62% reported using SDM. At baseline, there were no differences in QOL dimensions between DLOC groups. At 4 months, patient-directed (p = 0.01) and SDM (p = 0.03) were associated with better physical functioning than physician-directed decision-making, and there was an indication of potentially greater decision satisfaction among patients who reported patient-directed (p = 0.06) or SDM (p = 0.10). SDM was the most reported preferred DLOC.
Conclusion
mPC patients reporting SDM had better physical functioning at 4 months than physician- or patient-directed decision-making, suggesting measurable benefit from patient involvement in decision-making. Future investigations of these associations in larger, more diverse populations can further clarify these previously unmeasured benefits of patient engagement in treatment decisions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
American Cancer Society. Cancer Facts & Figures 2022. Atlanta: American Cancer Society; 2022.
Oswald LB, Schumacher FA, Gonzalez BD, Moses KA, Penson DF, Morgans AK. What do men with metastatic prostate cancer consider when making treatment decisions? A mixed-methods study. Patient Prefer Adherence. 2020;14:1949–59.
Elkin EB, Kim SHM, Casper ES, Kissane DW, Schrag D. Desire for information and involvement in treatment decisions: elderly cancer patients’ preferences and their physicians’ perceptions. J Clin Oncol. 2007;25:5275–80.
Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45:941–50.
Keating NL, Guadagnoli E, Landrum MB, Borbas C, Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? J Clin Oncol. 2002;20:1473–1479.
Oswald LB, Kasimer R, Rappazzo K, Fought AJ, Penson DF, Morgans AK. Patient expectations of benefit from systemic treatments for metastatic prostate cancer. Cancer Med. 2020;9:980–7.
Schumacher FA, Helenowski IB, Oswald LB, Gonzalez BD, Benning JT, Morgans AK. Treatment decision-making in metastatic prostate cancer: perceptions of locus of control among patient, caregiver, and physician triads. Patient Prefer Adherence. 2022;16:235–44.
Hawley ST, Lantz PM, Janz NK, Salem B, Morrow M, Schwartz K, et al. Factors associated with patient involvement in surgical treatment decision making for breast cancer. Patient Educ Couns. 2007;65:387–95.
Kehl KL, Landrum MB, Arora NK, Ganz PA, van Ryn M, Mack JW, et al. Association of actual and preferred decision roles with patient-reported quality of care: shared decision making in cancer care. JAMA Oncol. 2015;1:50–58.
Degner LF, Kristjanson LJ, Bowman D, Sloan JA, Carriere KC, O’Neil J, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277:1485–1492.
Beaver K, Luker KA, Owens RG, Leinster SJ, Degner LF, Sloan JA. Treatment decision making in women newly diagnosed with breast cancer. Cancer Nurs. 1996;19:8–19.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76.
Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: the Satisfaction with Decision scale. Med Decis Mak. 1996;16:58–64.
Bilodeau BA, Degner LF. Information needs, sources of information, and decisional roles in women with breast cancer. Oncol Nurs Forum. 1996;23:691–6.
Kluetz PG, O’Connor DJ, Soltys K. Incorporating the patient experience into regulatory decision making in the USA, Europe, and Canada. Lancet Oncol. 2018;19:e267–e274.
Resnick MJ, Penson DF. Quality of life with advanced metastatic prostate cancer. Urol Clin North Am. 2012;39:505–15.
Clark JA, Wray N, Brody B, Ashton C, Giesler B, Watkins H. Dimensions of quality of life expressed by men treated for metastatic prostate cancer. Soc Sci Med. 1997;45:1299–1309.
Clark JA, Wray N, Ashton CM. Living with treatment decisions: regrets and quality of life among men treated for metastatic prostate cancer. J Clin Oncol. 2001;19:72–80.
Nicolai J, Buchholz A, Seefried N, Reuter K, Härter M, Eich W, et al. When do cancer patients regret their treatment decision? A path analysis of the influence of clinicians’ communication styles and the match of decision-making styles on decision regret. Patient Educ Couns. 2016;99:739–46.
Schneider A, Korner T, Mehring M, Wensing M, Elwyn G, Szecsenyi J. Impact of age, health locus of control and psychological co-morbidity on patients’ preferences for shared decision making in general practice. Patient Educ Couns. 2006;61:292–8.
Saha S, Beach MC. The impact of patient-centered communication on patients’ decision making and evaluations of physicians: a randomized study using video vignettes. Patient Educ Couns. 2011;84:386–92.
U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research, U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research & U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
Acknowledgements
This work was supported by the Department of Defense Physician Research Training Award PC150398.
Funding
Department of Defense Physician Research Training Award PC150398 (PI Morgans).
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: AM, data collection: FS, AM, KM, analysis and interpretation of results: FS, IH, ZS, AM, draft manuscript preparation: FS, JB, LO, BG, KM, AM. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
BDG reports personal fees from SureMed Compliance, KemPharm, and Elly Health, Inc. unrelated to this work. All other authors declare no competing interests.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schumacher, F.A., Helenowski, I.B., Sun, Z. et al. Treatment decision-making among patients with metastatic prostate cancer: Impact of decision locus of control on functional outcomes and decision satisfaction. Prostate Cancer Prostatic Dis 26, 201–206 (2023). https://doi.org/10.1038/s41391-023-00647-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-023-00647-5