Abstract
Background
Benign prostatic hyperplasia, lower urinary tract symptoms, and prostate cancer often co-occur. Their effect on urinary function is an important consideration regarding prostate cancer treatment choices. While prostate volume (PV) and urinary symptoms are commonly used in treatment choice decision making, their association with post-treatment urinary function is unknown. We evaluated the associations between PV and baseline urinary function with treatment choice and post-treatment urinary function among men with localized prostate cancer.
Methods
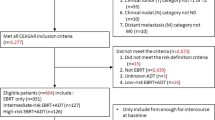
We identified 1647 patients from CEASAR, a multicenter population-based, prospective cohort study of men with localized prostate cancer, for analysis. Primary outcomes were treatment choice and health-related quality of life (HRQOL) assessed by the 26-item Expanded Prostate Index Composite (EPIC-26) at pre-specified intervals up to 5 years. Multivariable analysis was performed, controlling for demographic and clinicopathologic features.
Results
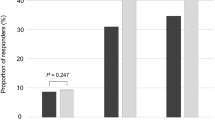
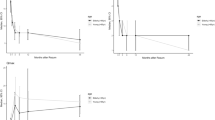
Median baseline PV was 36 mL (IQR 27–48), and baseline urinary irritative/obstructive domain score was 87 (IQR 75–100). There was no observed clinically meaningful association between PV and treatment choice or post-treatment urinary function. Among patients with poor baseline urinary function, treatment with radiation or surgery was associated with statistically and clinically significant improvement in urinary function at 6 months which was durable through 5 years (improvement from baseline at 5 years: radiation 20.4 points, surgery 24.5 points).
Conclusions
PV was not found to be associated with treatment modality or post-treatment urinary irritative/obstructive function among men treated for localized prostate cancer. Men with poor baseline urinary irritative/obstructive function improve after treatment with surgery or radiation therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
08 March 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41391-023-00658-2
References
Bostwick DG, Cooner WH, Denis L, Jones GW, Scardino PT, Murphy GP. The association of benign prostatic hyperplasia and cancer of the prostate. Cancer. 1992;70:291–301.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part II: recommended approaches and details of specific care options. J Urol. 2018;199:990–7.
Eastham JA, Auffenberg GB, Barocas DA, Chou R, Crispino T, Davis JW, et al. Clinically localized prostate cancer: AUA/ASTRO guideline, Part I: Introduction, Risk Assessment, Staging and Risk-Based Management. J Urol. 2022. https://doi.org/10.1097/JU.0000000000002757.
Barocas DA, Penson DF. Functional recovery following primary treatment for prostate cancer: update from the CEASAR study. Eur Urol Focus. 2020;6:205–7.
Mendenhall NP, Rausch Osian SM, Bryant CM, Hoppe BS, Morris CG. What men want: results from a national survey on decision making for prostate cancer treatment and research participation. Clin Transl Sci. 2021; cts.13090.
Barocas DA, Chen V, Cooperberg M, Goodman M, Graff JJ, Greenfield S, et al. Using a population-based observational cohort study to address difficult comparative effectiveness research questions: The CEASAR study. J Comp Eff Res. 2013;2:445–60.
Mandel P, Weinhold P, Michl U, Huland H, Graefen M, Tilki D. Impact of prostate volume on oncologic, perioperative, and functional outcomes after radical prostatectomy. Prostate. 2015;75:1436–46.
Ward NT, Parsons JK, Levinson AW, Bagga HS, Mettee LZ, Su L-M, et al. Prostate size is not associated with recovery of sexual function after minimally invasive radical prostatectomy. Urology. 2011;77:952–6.
Levinson AW, Bagga HS, Pavlovich CP, Mettee LZ, Ward NT, Link RE, et al. The impact of prostate size on urinary quality of life indexes following laparoscopic radical prostatectomy. J Urol. 2008;179:1818–22.
Szymanski KM, Wei JT, Dunn RL, Sanda MG. Development and validation of an abbreviated version of the expanded prostate cancer index composite instrument for measuring health-related quality of life among prostate cancer survivors. Urology. 2010;76:1245–50.
Skolarus TA, Dunn RL, Sanda MG, Chang P, Greenfield TK, Litwin MS, et al. Minimally important difference for the expanded prostate cancer index composite short form. Urology. 2015;85:101–6.
Litwin MS, Greenfield S, Elkin EP, Lubeck DP, Broering JM, Kaplan SH. Assessment of prognosis with the total illness burden index for prostate cancer. Cancer. 2007;109:1777–83.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Radloff LS. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401.
Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians participatory decision-making style. Med Care. 1995;33:1176–87.
White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817.
Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. In: Lecam L, Neyman J (eds). Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. University of California Press, 1966, pp 221–34.
White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30:377–99.
Schafer JL. Analysis of Incomplete Multivariable Data. 1st ed. Chapman and Hall CRC Press: London, UK, 1997.
Simon RM, Howard LE, Moreira DM, Roehrborn C, Vidal AC, Castro-Santamaria R, et al. Does prostate size predict the development of incident lower urinary tract symptoms in men with mild to no current symptoms? Results from the REDUCE Trial. Eur Urol. 2016;69:885–91.
Crawford ED, Wilson SS, McConnell JD, Slawin KM, Lieber MC, Smith JA, et al. Baseline factors as predictors of clinical progression of benign prostatic hyperplasia in men treated with placebo. J Urol. 2006;175:1422–7.
Vesely S, Knutson T, Damber J-E, Dicuio M, Dahlstrand C. Relationship between age, prostate volume, prostate-specific antigen, symptom score and uroflowmetry in men with lower urinary tract symptoms. Scand J Urol Nephrol. 2003;37:322–8.
Uberoi P, Smith CA, Lucioni A. Management of lower urinary tract symptoms after prostate radiation. Curr Urol Rep. 2021;22:37.
Masters JG, Rice ML. Improvement in urinary symptoms after radical prostatectomy: a prospective evaluation of flow rates and symptom scores. BJU Int. 2003;91:795–7.
Schwartz EJ, Lepor H. Radical retropubic prostatectomy reduces symptom scores and improves quality of life in men with moderate and severe lower urinary tract symptoms. J Urol. 1999;161:1185–8.
Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N. Engl J Med. 2008;358:1250–61.
Teunissen FR, Willigenburg T, Meijer RP, van Melick HHE, Verkooijen HM, van der Voort van Zyp JRN. The first patient-reported outcomes from the Utrecht Prostate Cohort (UPC): the first platform facilitating ‘trials within cohorts’ (TwiCs) for the evaluation of interventions for prostate cancer. World J Urol. 2022;40:2205–12.
Pepin A, Pernia M, Danner MT, Ayoob M, Yung TM, Lei S, et al. Impact of age on patient-reported outcomes following stereotactic body radiation therapy for prostate cancer. Cureus. 2021. https://doi.org/10.7759/cureus.13780.
Wang F, Luan Y, Fan Y, Huang T, Zhu L, Lu S, et al. Comparison of the oncological and functional outcomes of brachytherapy and radical prostatectomy for localized prostate cancer. Med (B Aires). 2022;58:1387.
Funding
AHRQ: 1R01HS019356, 1R01HS022640. PCORI: CE-12-11-4667. NIH/NCI: R01CA230352. NCATS/NIH: UL1TR000011.
Author information
Authors and Affiliations
Contributions
JET, MD: 1,3,4,5,6. CJDW, MD, PhD, FRCSC: 1,3,4,5,6. ZZ, MS: 1,3,5,6. L-CH, PhD: 1,3,5,6. DFP, MD, MPH: 1,2,5,6. TK, PhD: 1,3,5,6. MG, MD, MPH: 1,2,5,6. ASH, PhD, MA: 1,2,5,6. X-CW, MD, MPH: 1,2,5,6. LEP, PhD, MPH: 1,2,5,6. AS, PhD: 1,2,5,6. MRC, MD, MPH: 1,2,5,6. MH, PhD:1,2,5,6. BBO’N, MD: 1,2,5,6. SHK, PhD, MS, MPH: 1,2,5,6. SG, MD: 1,2,5,6. KEH, MD, MHSc, MPH: 1,2,5,6. DAB, MD, MPH: 1,2,3,4,5,6. (1) Conception or design of the work. (2) Data collection. (3) Data analysis and interpretation. (4) Drafting the article. (5) Critical revision of the article. (6) Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In this article the statement in the Funding information section was incorrectly given as '5T32CA106183' and has been deleted. The original article has been corrected.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tallman, J.E., Wallis, C.J.D., Zhao, Z. et al. Prostate volume, baseline urinary function, and their association with treatment choice and post-treatment urinary function in men treated for localized prostate cancer. Prostate Cancer Prostatic Dis 26, 787–794 (2023). https://doi.org/10.1038/s41391-022-00627-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00627-1
This article is cited by
-
Prevalence of lower urinary tract symptoms in taxi drivers: a cross-sectional web-based survey
Prostate Cancer and Prostatic Diseases (2023)