Abstract
Background
High-risk prostate cancer includes heterogenous populations with variable outcomes. This study aimed to compare the prognostic ability of individual high-risk factors, as defined by National Comprehensive Cancer Network (NCCN) risk stratification, in prostate cancer patients undergoing radical prostatectomy.
Methods
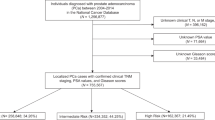
We queried the National Cancer Database from 2004 to 2018 for patients with non-metastatic high-risk prostate cancer who underwent radical prostatectomy and stratified them as Group H1: Prostate specific antigen (PSA) > 20 ng/ml alone, Group H2: cT3a stage alone and Group H3: Gleason Grade (GG) group 4/5 as per NCCN guidelines. The histopathological characteristics and rate of adjuvant therapy were compared between different groups. Inverse probability weighting (IPW)-adjusted Kaplan–Meier curves were utilized to compare overall survival (OS) in group H1 and H2 with H3.
Results
Overall, 61,491 high-risk prostate cancer patients were identified, and they were classified into Group H1 (n = 14,139), Group H2 (n = 2855) and Group H3 (n = 44,497). Compared to group H1 or H2, pathological GG group > 3 (p < 0.001), pathological stage pT3b or higher (p < 0.001), lymph nodal positive disease (pN1) (p < 0.001) and rate of adjuvant therapy (p < 0.001) were significantly in Group H3. IPW-adjusted Kaplan–Meier curves showed significantly better 5-year OS in group H1 compared to group H3 [95.1% vs 93.3%, p < 0.001] and group H2 compared to group H3 [94.4% vs 92.9%, p < 0.001].
Conclusion
PSA > 20 ng/ml or cT3a stage in isolation have better oncologic and survival outcomes compared to GG > 3 disease and sub-stratification of ‘High-risk’ category might lead to better patient prognostication.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data is available from the corresponding author on request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Rodrigues G, Warde P, Pickles T, Crook J, Brundage M, Souhami L, et al. Pre-treatment risk stratification of prostate cancer patients: A critical review. Can Urol Assoc J. 2012;6:121–7.
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. Jama. 1998;280:969–74.
Sundi D, Wang VM, Pierorazio PM, Han M, Bivalacqua TJ, Ball MW, et al. Very-high-risk localized prostate cancer: definition and outcomes. Prostate Cancer Prostatic Dis. 2014;17:57–63.
Tom MC, Reddy CA, Smile TD, Zhang RX, Ciezki JP, Stephans KL, et al. Validation of the NCCN prostate cancer favorable- and unfavorable-intermediate risk groups among men treated with I-125 low dose rate brachytherapy monotherapy. Brachytherapy. 2020;19:43–50.
Joniau S, Briganti A, Gontero P, Gandaglia G, Tosco L, Fieuws S, et al. Stratification of high-risk prostate cancer into prognostic categories: a European multi-institutional study. Eur Urol. 2015;67:157–64.
Walz J, Joniau S, Chun FK, Isbarn H, Jeldres C, Yossepowitch O, et al. Pathological results and rates of treatment failure in high-risk prostate cancer patients after radical prostatectomy. BJU Int. 2011;107:765–70.
Zumsteg ZS, Chen Z, Howard LE, Amling CL, Aronson WJ, Cooperberg MR, et al. Modified risk stratification grouping using standard clinical and biopsy information for patients undergoing radical prostatectomy: Results from SEARCH. Prostate. 2017;77:1592–600.
Muralidhar V, Chen MH, Reznor G, Moran BJ, Braccioforte MH, Beard CJ, et al. Definition and validation of “favorable high-risk prostate cancer”: implications for personalizing treatment of radiation-managed patients. Int J Radiat Oncol Biol Phys. 2015;93:828–35.
Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D’Amico AV, et al. Prostate cancer, version 2.2014. J Natl Compr Canc Netw. 2014;12:686–718.
Sundi D, Tosoian JJ, Nyame YA, Alam R, Achim M, Reichard CA, et al. Outcomes of very high-risk prostate cancer after radical prostatectomy: Validation study from 3 centers. Cancer. 2019;125:391–7.
Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Bekelman JE, Cheng H, et al. NCCN guidelines insights: prostate cancer, version 1.2021. J Natl Compr Canc Netw. 2021;19:134–43.
Spahn M, Joniau S, Gontero P, Fieuws S, Marchioro G, Tombal B, et al. Outcome predictors of radical prostatectomy in patients with prostate-specific antigen greater than 20 ng/ml: a European multi-institutional study of 712 patients. Eur Urol. 2010;58:1–7.
Chys B, Devos G, Everaerts W, Albersen M, Moris L, Claessens F, et al. Preoperative risk-stratification of high-risk prostate cancer: a multicenter analysis. Front Oncol. 2020;10:246.
Butler SS, Dee EC, Lamba N, Sha ST, Mahal BA, Whitbeck A, et al. Validation of a subclassification for high-risk prostate cancer in a prospective cohort. Cancer. 2020;126:2132–8.
American College of Surgeons -About the National Cancer Database. https://www.facs.org/quality-programs/cancer/ncdb/about. Accessed October, 2021.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33:1242–58.
Chierigo F, Wenzel M, Würnschimmel C, Flammia RS, Horlemann B, Tian Z, et al. Survival after radical prostatectomy versus radiation therapy in high-risk and very high-risk prostate cancer. J Urol. 2022;207:375–84.
Stephenson AJ, Kattan MW, Eastham JA, Bianco FJ Jr., Yossepowitch O, Vickers AJ, et al. Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol: Off J Am Soc Clin Oncol 2009;27:4300–5.
Kobayashi T, Kimura T, Lee C, Inoue T, Terada N, Kono Y, et al. Subclassification of high-risk clinically organ-confined prostate cancer for early cancer-specific mortality after radical prostatectomy. Jpn J Clin Oncol. 2016;46:762–7.
Muralidhar V, Zhang J, Wang Q, Mahal BA, Butler SS, Spratt DE, et al. Genomic validation of 3-tiered clinical subclassification of high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2019;105:621–7.
Fontenot PA, Mansour AM. Reporting positive surgical margins after radical prostatectomy: time for standardization. BJU Int. 2013;111:E290–9.
Author information
Authors and Affiliations
Contributions
HG- Investigation, visualization, Data curation, Data analysis, writing – original draft. FD- Investigation, visualization, Writing - Review & Editing. FA- Investigation, visualization, Writing - Review & Editing. HW- Data analysis, visualization, Writing - Review & Editing. SW- Data analysis, Visualization, ML- Investigation, visualization, Writing - Review & Editing. DK- Investigation, visualization, Writing - Review & Editing. RSS- Investigation, Writing - Review & Editing. AMM- Conceptualization, Methodology, Writing – review and editing, Supervision, Project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was done in accordance with the Declaration of Helsinki. It is a retrospective analysis of National Cancer Database and the need for informed consent was waived in view of anonymity of the data. The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garg, H., Dursun, F., Alsayegh, F. et al. Revisiting current National Comprehensive Cancer Network (NCCN) high-risk prostate cancer stratification: a National Cancer Database analysis. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-022-00621-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-022-00621-7
This article is cited by
-
Prognostic factors among patients with pathological Grade Group 5 prostate cancer based on robot-associated radical prostatectomy specimens from a large Japanese cohort (MSUG94)
World Journal of Urology (2024)
-
Therapeutic, diagnostic and prognostic values of TRIM proteins in prostate cancer
Pharmacological Reports (2023)