Abstract
Background
Most of the epidemiological data on prostate cancer risk factors come from high-income countries (HIC). Reducing exposure to prostate cancer modifiable risk factors may significantly lower PCa morbidity and mortality in LIC and MIC. The objective of this study was to summarize the evidence on modifiable risk factors (RFs) for PCa in LIC and lower-middle-income countries (LMIC).
Methods
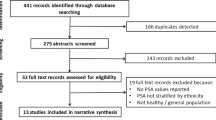
We conducted a systematic search on MEDLINE, EMBASE, and Global Health databases. We selected case-control and cohort studies from 2010 onwards that studied modifiable RFs for PCa in LIC and LMIC with a population of 30 million or more, as defined by the World Bank in January 2021. Risk of bias was assessed by the Ottawa-Newcastle tool. Individual study estimates were pooled when estimates were available for at least two studies.
Results
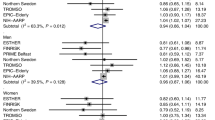
5740 studies were initially identified; 16 studies met inclusion criteria. All were case–control studies except one retrospective cohort study. Higher fat intake was associated with a higher risk of PCa incidence with an odds ratio (OR) of 3.13 (95% CI 1.33–7.33). Higher vegetable intake (OR 0.48, 95% CI 0.24–0.97) and tea consumption (OR 0.51, 95% CI 0.32–0.83) were associated with a lower risk for PCa. There was no association between fruits, fish, and chicken consumption and risk of PCa. Alcohol consumption, smoking, red meat intake, and a BMI ≥ 25–30 kg/m2 showed a trend towards an increased risk, although these were not statistically significant.
Conclusions
In LIC and LMIC, high fat intake was associated with higher risk of PCa while a diet rich in vegetables and tea intake was associated with a lower risk. Future prospective studies will be important to elucidate whether other modifiable risk factors for PCa specific to LIC and LMIC can be identified to inform impactful and cost-effective preventive strategies in these countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All the data used for this study are available online on journal sites where the included studies were retrieved from.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Hassanipour-Azgomi S, Mohammadian-Hafshejani A, Ghoncheh M, Towhidi F, Jamehshorani S, Salehiniya H. Incidence and mortality of prostate cancer and their relationship with the Human Development Index worldwide. Prostate Int. 2016;4:118–24.
Gann PH. Risk factors for prostate cancer. Rev Urol. 2002;4:S3–S10.
Prostate Cancer Risk Factors [Internet]. https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/risk-factors.html. Accessed 8 Nov 2021.
Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–90.
Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009;12:497–506.
Sathish T, Teo KK, Britz-McKibbin P, Gill B, Islam S, Paré G, et al. Variations in risks from smoking between high-income, middle-income, and low-income countries: an analysis of data from 179 000 participants from 63 countries. Lancet Glob Health. 2022;10:e216–26.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:71.
World Bank Country and Lending Groups—World Bank Data Help Desk [Internet]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 31 Oct 2021.
Ottawa Hospital Research Institute [Internet]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 31 Oct 2021.
Tyagi B, Manoharan N, Raina V. A case control study on prostate cancer in Delhi. Asian Pac J Cancer Prev. 2010;11:397–401.
Ganesh B, Saoba SL, Sarade MN, Pinjari SV. Risk factors for prostate cancer: an hospital-based case-control study from Mumbai, India. Indian J Urol 2011;27:345–50.
George GP, Ramesh V, Mittal RD. Impact of total and ionized serum calcium on prostate cancer risk in North Indian men. Asian Pac J Cancer Prev. 2011;12:1257–60.
Mahmood S, Qasmi G, Ahmed A, Kokab F, Zahid MF, Afridi MI, et al. Lifestyle factors associated with the risk of prostate cancer among Pakistani men. J Ayub Med Coll. 2012;24:111–5.
Bashir MN, Ahmad MR, Malik A. Risk factors of prostate cancer: a case-control study in Faisalabad, Pakistan. Asian Pac J Cancer Prev. 2014;15:10237–40.
Singh N, Hussain S, Kakkar N, Singh SK, Sobti RC, Bharadwaj M. Implication of high risk human papillomavirus HR-HPV infection in prostate cancer in Indian population—a pioneering case-control analysis. Sci Rep. 2015;5:7822.
Bashir MN, Malik MA. Case-control study of diet and prostate cancer in a rural population of Faisalabad, Pakistan. Asian Pac J Cancer Prev. 2015;16:2375–8.
Agalliu I, Adebiyi AO, Lounsbury DW, Popoola O, Jinadu K, Amodu O, et al. The feasibility of epidemiological research on prostate cancer in African men in Ibadan, Nigeria. BMC Public Health. 2015;15:425.
Lassed S, Deus CM, Lourenço N, Dahdouh A, Rizvanov AA, Oliveira PJ, et al. Diet, lifestyles, family history, and prostate cancer incidence in an East Algerian Patient Group. BioMed Res Int. 2016;2016:5730569.
Van Hoang D, Pham NM, Lee AH, Tran DN, Binns CW. Dietary carotenoid intakes and prostate cancer risk: a case-control study from Vietnam. Nutrients 2018;10:E70.
Malik SS, Batool R, Masood N, Yasmin A. Risk factors for prostate cancer: a multifactorial case-control study. Curr Probl Cancer. 2018;42:337–43.
Gunda D, Kido I, Kilonzo S, Nkandala I, Igenge J, Mpondo B. Prevalence and associated factors of incidentally diagnosed prostatic carcinoma among patients who had transurethral prostatectomy in Tanzania: a retrospective study. Ethiop J Health Sci. 2018;28:11–8.
Hoang DV, Shivappa N, Pham NM, Hebert JR, Binns CW, Lee AH. Dietary inflammatory index is associated with increased risk for prostate cancer among Vietnamese men. Nutr Burbank. 2019;62:140–5.
Adler C, Friesen MC, Yeboah ED, Tettey Y, Biritwum RB, Adjei AA, et al. Usual adult occupation and risk of prostate cancer in West African men: The Ghana Prostate Study. Occup Environ Med. 2019;76:71–7.
Hurwitz LM, Yeboah ED, Biritwum RB, Tettey Y, Adjei AA, Mensah JE, et al. Overall and abdominal obesity and prostate cancer risk in a West African population: an analysis of the Ghana Prostate Study. Int J Cancer. 2020;147:2669–76.
Saleh NE, Alhusseiny SM, El-Zayady WM, Aboelnaga EM, El-Beshbishi WN, Saleh YM, et al. Trichomonas vaginalis serostatus and prostate cancer risk in Egypt: a case-control study. Parasitol Res. 2021;120:1379–88.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276–82.
McPheeters ML, Kripalani S, Peterson NB, Idowu RT, Jerome RN, Potter SA, et al. Thresholds for Quality Assessment [Internet]. Closing the Quality Gap: Revisiting the State of the Science (Vol. 3: Quality Improvement Interventions To Address Health Disparities). Agency for Healthcare Research and Quality (US); 2012. https://www.ncbi.nlm.nih.gov/books/NBK107322/. Accessed 12 Oct 2021.
Xu C, Han FF, Zeng XT, Liu TZ, Li S, Gao ZY. Fat intake is not linked to prostate cancer: a systematic review and dose-response meta-analysis. PLoS ONE. 2015;10:e0131747.
Yan H, Cui X, Zhang P, Li R. Fruit and vegetable consumption and the risk of prostate cancer: a systematic review and meta-analysis. Nutr Cancer. 2021;21:1–8.
Liu B, Mao Q, Cao M, Xie L. Cruciferous vegetables intake and risk of prostate cancer: a meta-analysis. Int J Urol. 2012;19:134–41.
Etminan M, Takkouche B, Caamaño-Isorna F. The role of tomato products and lycopene in the prevention of prostate cancer: a meta-analysis of observational studies. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 2004;13:340–5.
Alexander DD, Mink PJ, Cushing CA, Sceurman B. A review and meta-analysis of prospective studies of red and processed meat intake and prostate cancer. Nutr J. 2010;9:50.
Bylsma LC, Alexander DD. A review and meta-analysis of prospective studies of red and processed meat, meat cooking methods, heme iron, heterocyclic amines and prostate cancer. Nutr J. 2015;14:125.
Discacciati A, Orsini N, Wolk A. Body mass index and incidence of localized and advanced prostate cancer—a dose–response meta-analysis of prospective studies. Ann Oncol. 2012;23:1665–71.
Harrison S, Tilling K, Turner EL, Martin RM, Lennon R, Lane JA, et al. Systematic review and meta-analysis of the associations between body mass index, prostate cancer, advanced prostate cancer, and prostate-specific antigen. Cancer Causes Control. 2020;31:431–49.
Perez‐Cornago A, Travis RC, Appleby PN, Tsilidis KK, Tjønneland A, Olsen A, et al. Fruit and vegetable intake and prostate cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Int J Cancer. 2017;141:287–97.
He Q, Wan Z-CE, Xu X-BING, Wu J, Xiong G-LIAN. Poultry consumption and prostate cancer risk: a meta-analysis. PeerJ 2016;4:e1646.
Szymanski KM, Wheeler DC, Mucci LA. Fish consumption and prostate cancer risk: a review and meta-analysis. Am J Clin Nutr. 2010;92:1223–33.
Lin Y-WEI, Hu Z-HUI, Wang X, Mao Q-QI, Qin J, Zheng X-YI, et al. Tea consumption and prostate cancer: an updated meta-analysis. World J Surg Oncol. 2014;12:38.
Sen A, Papadimitriou N, Lagiou P, Perez-Cornago A, Travis RC, Key TJ, et al. Coffee and tea consumption and risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2019;144:240–50.
Zheng J, Yang B, Huang T, Yu Y, Yang J, Li D. Green tea and black tea consumption and prostate cancer risk: an exploratory meta-analysis of observational studies. Nutr Cancer. 2011;63:663–72.
Guo Y, Zhi F, Chen P, Zhao K, Xiang H, Mao Q, et al. Green tea and the risk of prostate cancer: a systematic review and meta-analysis. Medicines. 2017;96:e6426.
Bettuzzi S, Brausi M, Rizzi F, Castagnetti G, Peracchia G, Corti A. Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer Res. 2006;66:1234–40.
Middleton Fillmore K, Chikritzhs T, Stockwell T, Bostrom A, Pascal R. Alcohol use and prostate cancer: a meta-analysis. Mol Nutr Food Res. 2009;53:240–55.
Hong S, Khil H, Lee DH, Keum N, Giovannucci EL. Alcohol consumption and the risk of prostate cancer: a dose-response meta-analysis. Nutrients 2020;12:2188.
Huncharek M, Haddock KS, Reid R, Kupelnick B. Smoking as a risk factor for prostate cancer: a meta-analysis of 24 prospective cohort studies. Am J Public Health. 2010;100:693–701.
Islami F, Moreira DM, Boffetta P, Freedland SJ. A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur Urol. 2014;66:1054–64.
Benke IN, Leitzmann MF, Behrens G, Schmid D. Physical activity in relation to risk of prostate cancer: a systematic review and meta-analysis. Ann Oncol Off J Eur Soc. Med Oncol. 2018;29:1154–79.
Berger FF, Leitzmann MF, Hillreiner A, Sedlmeier AM, Prokopidi-Danisch ME, Burger M, et al. Sedentary behavior and prostate cancer: a systematic review and meta-analysis of prospective cohort studies. Cancer Prev Res. 2019;12:675–88.
Maele-Fabry GV, Willems JL. Occupation related pesticide exposure and cancer of the prostate: a meta-analysis. Occup Environ Med. 2003;60:634–42.
Rao D, Yu H, Bai Y, Zheng X, Xie L. Does night-shift work increase the risk of prostate cancer? A systematic review and meta-analysis. OncoTargets Ther. 2015;8:2817–26.
Lewis-Mikhael AM, Bueno-Cavanillas A, Guiron TO, Olmedo-Requena R, Delgado-Rodríguez M, Jiménez-Moleón JJ. Occupational exposure to pesticides and prostate cancer: a systematic review and meta-analysis. Occup Environ Med. 2016;73:134–44.
Krstev S, Knutsson A. Occupational risk factors for prostate cancer: a meta-analysis. J Cancer Prev. 2019;24:91–111.
Bosland MC. The role of estrogens in prostate carcinogenesis: a rationale for chemoprevention. Rev Urol. 2005;7:S4–S10.
Ragin C, Davis-Reyes B, Tadesse H, Daniels D, Bunker CH, Jackson M, et al. Farming, reported pesticide use, and prostate cancer. Am J Mens Health. 2013;7:102–9.
Kaneko R, Zaitsu M, Sato Y, Kobayashi Y. Risk of cancer and longest-held occupations in Japanese workers: a multicenter hospital-based case-control study. Cancer Med. 2019;8:6139–50.
Mistry K, Cable G. Meta-analysis of prostate-specific antigen and digital rectal examination as screening tests for prostate carcinoma. J Am Board Fam Pract. 2003;16:95–101.
Lumen N, Fonteyne V, De Meerleert G, Ost P, Villeirs G, Mottrie A, et al. Population screening for prostate cancer: an overview of available studies and meta-analysis. Int J Urol. 2012;19:100–8.
Coughlin SS. A review of social determinants of prostate cancer risk, stage, and survival. Prostate Int. 2020;8:49–54.
Dennis LK, Dawson DV. Meta-analysis of measures of sexual activity and prostate cancer. Epidemiology 2002;13:72–9.
Taylor ML, Mainous AG, Wells BJ. Prostate cancer and sexually transmitted diseases: a meta-analysis. Fam Med. 2005;37:506–12.
Caini S, Gandini S, Dudas M, Bremer V, Severi E, Gherasim A. Sexually transmitted infections and prostate cancer risk: a systematic review and meta-analysis. Cancer Epidemiol. 2014;38:329–38.
Yin B, Liu W, Yu P, Liu C, Chen Y, Duan X, et al. Association between human papillomavirus and prostate cancer: a meta-analysis. Oncol Lett. 2017;14:1855–65.
Russo GI, Calogero AE, Condorelli RA, Scalia G, Morgia G, La, et al. Human papillomavirus and risk of prostate cancer: a systematic review and meta-analysis. Aging Male J Int Soc Study Aging Male. 2020;23:132–8.
Najafi A, Chaechi Nosrati MR, Ghasemi E, Navi Z, Yousefi A, Majidiani H, et al. Is there association between Trichomonas vaginalis infection and prostate cancer risk? A systematic review and meta-analysis. Micro Pathog. 2019;137:103752.
Schetter AJ, Heegaard NHH, Harris CC. Inflammation and cancer: interweaving microRNA, free radical, cytokine and p53 pathways. Carcinogenesis 2010;31:37–49.
Lonkar P, Dedon PC. Reactive species and DNA damage in chronic inflammation: reconciling chemical mechanisms and biological fates. Int J Cancer. 2011;128:1999–2009.
Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S. The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158:1–7. PURE Investigators-Writing Group Jul e1.
Author information
Authors and Affiliations
Contributions
FC helped design the search strategy, collected the data, performed the statistical analysis and contributed to the manuscript; CK collected the data and contributed to the manuscript; SZ collected the data and contributed to the manuscript; SDM helped design the search strategy and contributed to the manuscript; MD contributed to the manuscript; JP designed the search strategy; DPL helped design the search strategy, reviewed the statistical analysis and contributed to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cirne, F., Kappel, C., Zhou, S. et al. Modifiable risk factors for prostate cancer in low- and lower-middle-income countries: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis 25, 453–462 (2022). https://doi.org/10.1038/s41391-022-00570-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00570-1
This article is cited by
-
Transcending frontiers in prostate cancer: the role of oncometabolites on epigenetic regulation, CSCs, and tumor microenvironment to identify new therapeutic strategies
Cell Communication and Signaling (2024)
-
A healthy diet, a healthy prostate? A brief commentary on the latest research on diet and prostate cancer
Prostate Cancer and Prostatic Diseases (2023)
-
Relationship between cigarette use and prostate cancer risk: what do we know and what should we do?
Prostate Cancer and Prostatic Diseases (2023)
-
Bacterial Peptides and Bacteriocins as Novel Treatment for Prostate Cancer
International Journal of Peptide Research and Therapeutics (2023)