Abstract
Background
To explore the role of preoperative MRI prostate shape in urinary incontinence after robot-assisted radical prostatectomy (RARP).
Methods
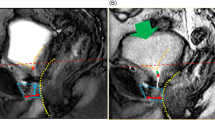
Patients were stratified into four groups based on the mpMRI prostatic apex shape: Group A (prostatic apex overlapping the membranous urethra anteriorly and posteriorly), Group B and C (overlap of the prostatic apex of the anterior or posterior membranous urethra, respectively) and Group D (no overlap). Preoperative variables and intraoperative data were compared. Continence recovery was defined as no pad/day or 1 safety pad/day by an outpatient evaluation performed at 1, 3, 6, and 12 months after RARP.
Results
One hundred patients underwent RARP were classified as belonging to Group A (n = 30), Group B (n = 16), Group C (n = 14), and Group D (n = 40). Group D showed a significantly more favorable urinary continence recovery after RARP respect to all the other shapes presenting any forms of overlapping (HR = 1.9, 95% CI 1.2–3.1, p = 0.007). The estimated HR remained substantially unchanged after adjusting by age, body mass index, CCI, prostate volume, and bladder neck sparing (HR = 1.9, 95% CI 1.1–3.2, p = 0.016). The continence recovery median time was 9 months for Group A + B + C (95% CI 5–11) and 4 months for Group D (95% CI 2–6) (p = 0.023).
Conclusion
Shape D showed a better continence recovery when compared to other shapes presenting any kind of overlapping of the prostatic apex over the membranous urethra.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mottet N, Cornford P, van den Bergh RCN, Briers E, De Santis M, Gillessen S, et al. EAU–EANM–ESTRO–ESUR–ISUP–SIOG, guidelines on prostate cancer. Eur Assoc Urol. 2021. https://uroweb.org/guideline/prostate-cancer/.
Averbeck MA, Woodhouse C, Comiter C, Bruschini H, Hanus T, Herschorn S, et al. Surgical treatment of post-prostatectomy stress urinary incontinence in adult men: report from the 6th International Consultation on Incontinence. Neurourol Urodyn. 2019;38:398–406.
Heesakkers J, Farag F, Bauer RM, Sandhu J, De Ridder D, Stenzl A. Pathophysiology and contributing factors in postprostatectomy incontinence: a review. Eur Urol. 2017;71:936–44.
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012;62:405–17.
Theissen L, Preisser F, Wenzel M, Humke C, Roos FC, Kluth LA, et al. Very early continence after radical prostatectomy and its influencing factors. Front Surg. 2019;6:60.
von Bodman C, Matsushita K, Savage C, Matikainen MP, Eastham JA, Scardino PT, et al. Recovery of urinary function after radical prostatectomy: predictors of urinary function on preoperative prostate magnetic resonance imaging. J Urol. 2012;187:945–50.
Averbeck MA, Marcelissen T, Anding R, Rahnama’i MS, Sahai A, Tubaro A. How can we prevent postprostatectomy urinary incontinence by patient selection, and by preoperative, peroperative, and postoperative measures? International Consultation on Incontinence-Research Society 2018. Neurourol Urodyn. 2019;38 Suppl 5:S119–26.
Lee H, Kim K, Hwang SI, Lee HJ, Byun SS, Lee SE, et al. Impact of prostatic apical shape and protrusion on early recovery of continence after robot-assisted radical prostatectomy. Urology. 2014;84:844–9.
Wenzel M, Preisser F, Mueller M, Theissen LH, Welte MN, Hoeh B, et al. Effect of prostatic apex shape (Lee types) and urethral sphincter length in preoperative MRI on very early continence rates after radical prostatectomy. Int Urol Nephrol. 2021;53:1297–303.
Burkhard FC, Bosch JLHR, Cruz F, Lemack GE, Nambiar AK, Thiruchelvam N, et al. EAU Guidelines on Urinary Incontinence. Eur Assoc Urol. 2020. https://uroweb.org/guideline/urinary-incontinence/.
Ditzhaus M, Dobler D, Pauly M. Inferring median survival differences in general factorial designs via permutation tests. Stat Methods Med Res. 2021;30:875–91.
Chiam K, Carle C, Hughes S, Kench JG, Woo HH, Lord S, et al. Use of multiparametric magnetic resonance imaging (mpMRI) in active surveillance for low-risk prostate cancer: a scoping review on the benefits and harm of mpMRI in different biopsy scenarios. Prostate Cancer Prostatic Dis. 2021;24:662–73.
Baack Kukreja J, Bathala TK, Reichard CA, Troncoso P, Delacroix S, Davies B, et al. Impact of preoperative prostate magnetic resonance imaging on the surgical management of high-risk prostate cancer. Prostate Cancer Prostatic Dis. 2020;23:172–8.
Sherrer RL, Glaser ZA, Gordetsky JB, Nix JW, Porter KK, Rais-Bahrami S. Comparison of biparametric MRI to full multiparametric MRI for detection of clinically significant prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:331–6.
Sievert KD, Amend B, Toomey PA, Robinson D, Milsom I, Koelbl H, et al. Can we prevent incontinence? ICI-RS 2011. Neurourol Urodyn. 2012;31:390–9.
Abrams, P, Cardozo, L, Wagg, A, Wein, A. Incontinence 6th ed. ICI-ICS. Pathophysiology of incontinence in men. International Continence Society. Bristol UK: ISBN: 978-0956960733; 2017. pp.431–433.
Wallner C, Dabhoiwala NF, DeRuiter MC, Lamers WH. The anatomical components of urinary continence. Eur Urol. 2009;55:932–43.
Mungovan SF, Sandhu JS, Akin O, Smart NA, Graham PL, Patel MI. Preoperative membranous urethral length measurement and continence recovery following radical prostatectomy: a systematic review and meta-analysis. Eur Urol. 2017;71:368–78.
Qiu X, Li Y, Chen M, Xu L, Guo S, Marra G, et al. Retzius-sparing robot-assisted radical prostatectomy improves early recovery of urinary continence: a randomized, controlled, single-blind trial with a 1-year follow-up. BJU Int. 2020;126:633–40.
Dalela D, Jeong W, Prasad MA, Sood A, Abdollah F, Diaz M, et al. A pragmatic randomized controlled trial examining the impact of the retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2017;72:677–85.
Barakat B, Othman H, Gauger U, Wolff I, Hadaschik B, Rehme C. Retzius sparing radical prostatectomy versus robot-assisted radical prostatectomy: which technique is more beneficial for prostate cancer patients (MASTER Study)? A systematic review and meta-analysis. Eur Urol Focus. 2021;S2405-4569:00218–2.
Rosenberg JE, Jung JH, Edgerton Z, Lee H, Lee S, Bakker CJ, et al. Retzius-sparing versus standard robotic-assisted laparoscopic prostatectomy for the treatment of clinically localized prostate cancer. Cochrane Database Syst Rev. 2020;8:CD013641.
Author information
Authors and Affiliations
Contributions
Protocol/project development: VI, MC, EFA, PB. Data collection or management: MC, VF, CC, MV, RB, FP, FM, MS, MA, AUC, MS. Data analysis: MS. Paper writing/editing: VI, MC, MS, CC, RB, EFA, PB.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iacovelli, V., Carilli, M., Sandri, M. et al. The role of preoperative prostatic shape in the recovery of urinary continence after robotic radical prostatectomy: a single cohort analysis. Prostate Cancer Prostatic Dis 26, 374–378 (2023). https://doi.org/10.1038/s41391-022-00563-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00563-0
This article is cited by
-
Comparison of senhance and da vinci robotic radical prostatectomy: short-term outcomes, learning curve, and cost analysis
Prostate Cancer and Prostatic Diseases (2024)
-
Membranous urethral length measurement on preoperative MRI to predict incontinence after radical prostatectomy: a literature review towards a proposal for measurement standardization
European Radiology (2023)