Abstract
Background
While prostate multiparametric-magnetic resonance imaging (MP-MRI) has improved the diagnosis of clinically significant prostate cancer (CSPC), the complementary use of prostate-specific antigen (PSA) levels to risk-stratify for CSPC requires further study. The objective of this project was to determine if prostate MP-MRI and PSA can provide complementary insights into CSPC risk stratification.
Methods
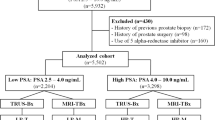
In an IRB-approved study, pathologic outcomes from patients who underwent MR/US fusion-targeted prostate biopsy were stratified by various parameters including PSA, PSA density (PSAD), age, race, and PI-RADS v2 score. CSPC was defined as a Gleason score ≥7. Logistic regression was used to determine odds ratios (OR) with 95% confidence intervals (CI). P values were reported as two-sided with p < 0.05 considered statistically significant. ROC curves were generated for assessing the predictive value of tests and sensitivity + specificity optimization was performed to determine optimal testing cutoffs.
Results
A total of 327 patients with 709 lesions total were analyzed. PSAD and PI-RADS scores provided complementary predictive value for diagnosis of CSPC (AUC PSAD: 0.67, PI-RADS: 0.72, combined: 0.78, p < 0.001). When controlling for PI-RADS score, age, and race, multivariate analysis showed that PSAD was independently associated with CSPC (OR 1.03 per 0.01 PSAD increase, 95% CI 1.02–105, p < 0.001). The optimal cutoff of PSAD ≥ 0.1 ng/ml/cc shows that a high versus low PSAD was roughly equivalent to an increase in 1 in PI-RADS score for the presence of CSPC (4% of PI-RADS ≤3 PSAD low, 6% of PI-RADS 3 PSAD high vs. 5% of PI-RADS 4 PSAD low, 22% of PI-RADS 4 PSAD high vs. 29% of PI-RADS 5 PSAD low, 46% of PI-RADS 5 PSAD high were found to have CSPC).
Conclusions
PSAD with a cutoff of 0.1 ng/ml/cc appears to be a useful marker that can stratify the risk of CSPC in a complementary manner to prostate MP-MRI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Kasel-Seibert M, Lehmann T, Aschenbach R, Guettler FV, Abubrig M, Grimm M-O, et al. Assessment of PI-RADS v2 for the detection of prostate cancer. Eur J Radio. 2016;85:726–31.
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876–92.
Minhaj Siddiqui M, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion–guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–7.
Baco E, Rud E, Eri LM, Moen G, Vlatkovic L, Svindland A, et al. A randomized controlled trial to assess and compare the outcomes of two-core prostate biopsy guided by fused magnetic resonance and transrectal ultrasound images and traditional 12-core systematic biopsy. Eur Urol. 2016;69:149–56.
Panebianco V, Barchetti F, Sciarra A, Ciardi A, Indino EL, Papalia R, et al. Multiparametric magnetic resonance imaging vs. standard care in men being evaluated for prostate cancer: a randomized study. Urol Oncol. 2015;33:17.e1–17.e7.
Kim YJ, Huh JS, Park KK. Effectiveness of bi-parametric MR/US fusion biopsy for detecting clinically significant prostate cancer in prostate biopsy naïve men. Yonsei Med J. 2019;60:346–51.
Eldred-Evans D, Burak P, Connor MJ, Day E, Evans M, Fiorentino F, et al. Population-based prostate cancer screening with magnetic resonance imaging or ultrasonography: the IP1-PROSTAGRAM study. JAMA Oncol. 2021;7:395–402. https://doi.org/10.1001/jamaoncol.2020.7456.
Eldred-Evans D, Tam H, Sokhi H, Padhani AR, Winkler M, Ahmed HU. Rethinking prostate cancer screening: could MRI be an alternative screening test? Nat Rev Urol. 2020;17:526–39.
Baruah SK, Das N, Baruah SJ, Rajeev TP, Bagchi PK, Sharma D, et al. Combining prostate-specific antigen parameters with Prostate Imaging Reporting and Data System score version 2.0 to improve its diagnostic accuracy. World J Oncol. 2019;10:218–25.
Bosch JLHR, Bohnen AM, Groeneveld FPMJ. Validity of digital rectal examination and serum prostate specific antigen in the estimation of prostate volume in community-based men aged 50 to 78 years: the Krimpen Study. Eur Urol. 2004;46:753–9.
Van Kuiken M, Blackwell RH, Bisanz B, Yacoub J, Goldberg A, Shea S, et al. PD55-09 role of MPMRI PSA density and PIRADS score in predicting upstaging in men on active surveillance. J Urol. 2017;197:e1054. https://doi.org/10.1016/j.juro.2017.02.2432.
Nordström T, Akre O, Aly M, Grönberg H, Eklund M. Prostate-specific antigen (PSA) density in the diagnostic algorithm of prostate cancer. Prostate Cancer Prostatic Dis. 2018;21:57–63.
Qi Y, Zhang S, Wei J, Zhang G, Lei J, Yan W, et al. Multiparametric MRI-based radiomics for prostate cancer screening with PSA in 4-10 ng/mL to reduce unnecessary biopsies: radiomics for prostate cancer screening. J Magn Reson Imaging. 2020;51:1890–9.
Callender T, Emberton M, Morris S, Pharoah PDP, Pashayan N. Benefit, harm, and cost-effectiveness associated with magnetic resonance imaging before biopsy in age-based and risk-stratified screening for prostate cancer. JAMA Netw Open. 2021;4:e2037657.
Stevens E, Truong M, Bullen JA, Ward RD, Purysko AS, Klein EA. Clinical utility of PSAD combined with PI-RADS category for the detection of clinically significant prostate cancer. Urol Oncol. 2020;38:846.e9–846.e16.
Park H, Kim JY, Lee BM, Chang SK, Ko SY, Kim SJ, et al. A comparison of preplan MRI and preplan CT-based prostate volume with intraoperative ultrasound-based prostate volume in real-time permanent brachytherapy. Radiat Oncol J. 2011;29:199–205.
Jeong CW, Park HK, Hong SK, Byun S-S, Lee HJ, Lee SE. Comparison of prostate volume measured by transrectal ultrasonography and MRI with the actual prostate volume measured after radical prostatectomy. Urol Int. 2008;81:179–85.
Frye TP, Pinto PA, George AK. Optimizing patient population for MP-MRI and fusion biopsy for prostate cancer detection. Curr Urol Rep. 2015;16:50.
Shakir NA, George AK, Siddiqui MM, Rothwax JT, Rais-Bahrami S, Stamatakis L, et al. Identification of threshold prostate specific antigen levels to optimize the detection of clinically significant prostate cancer by magnetic resonance imaging/ultrasound fusion guided biopsy. J Urol. 2014;192:1642–8.
Author information
Authors and Affiliations
Contributions
AJVB, AL, LX, SW, and JWF were responsible for adding and maintaining the list of patient parameters in the system database. AW was responsible for the review of PI-RADS lesions. MJN and MMS were responsible for conducting biopsies. JW was responsible for manuscript creation. JWF, AC, and SW were responsible for data analysis. All authors were involved in the revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Frisbie, J.W., Van Besien, A.J., Lee, A. et al. PSA density is complementary to prostate MP-MRI PI-RADS scoring system for risk stratification of clinically significant prostate cancer. Prostate Cancer Prostatic Dis 26, 347–352 (2023). https://doi.org/10.1038/s41391-022-00549-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00549-y
This article is cited by
-
Best of 2022 in prostate cancer and prostatic diseases
Prostate Cancer and Prostatic Diseases (2023)
-
The role of PSA density in the MRI pathway for prostate cancer diagnostics
Prostate Cancer and Prostatic Diseases (2023)
-
Enhanced PSA Density Prediction Accuracy When Based on Machine Learning
Journal of Medical and Biological Engineering (2023)