Abstract
Background
Men with progressive neuroendocrine or aggressive-variant metastatic prostate cancer (NEPC/AVPC) have a poor prognosis and limited treatment options, and immunotherapy has not been tested in such patients.
Methods
We conducted an open label single center phase 2 trial (NCT03179410) of men with progressive NEPC/AVPC either defined by histology or AVPC criteria. Avelumab (10 mg/kg every 2 weeks) was administered until progression or unacceptable toxicity. The primary endpoint was overall response rate (ORR). Secondary endpoints included ORR, radiographic progression-free survival (rPFS), overall survival, and safety. Correlative studies included longitudinal peripheral blood immune phenotyping. The study was limited by the small number of patients enrolled and by the early termination due to COVID-19.
Results
A total of 15 men with AVPC/NEPC were enrolled. The median age was 71 (range 51–85 years), and men had received a median of two prior therapies (range 1–3). Median PSA was 54 ng/dl (range 0–393), and 73% of men had liver metastasis. The ORR with avelumab in this setting by iRECIST or RECIST 1.1 was 6.7%, including one patient (6.7%) with a complete remission (CR), 20% with stable disease, and 67% with progressive disease. The patient with the CR had an MSH2 somatic mutation and MSI-high NEPC with central nervous system metastases, and his CR remains durable off all therapy for 2 years. The median rPFS was 1.8 months (95% CI 1.6–3.6 months), and median overall survival was 7.4 months (85% CI 2.8–12.6 months). Safety was consistent with the known profile of avelumab. Phenotyping of peripheral immune subsets suggest enhanced CXCR2-dependent myeloid and T-cell responses in this extraordinary responder.
Conclusions
While the study was terminated early due to slow enrollment at the onset of the COVID-19 pandemic and lower than anticipated objective response rate, PD-L1 inhibition with avelumab monotherapy showed poor efficacy in patients with microsatellite stable NEPC/AVPC. Immune profiling revealed enhanced CXCR2 positive immune cell activation in the one extraordinary responder, suggesting potential mechanisms for further immunotherapy development in this population.
Similar content being viewed by others
Introduction
Aggressive-variant prostate cancer (AVPC), also termed neuroendocrine prostate cancer (NEPC), androgen receptor (AR)-independent prostate cancer, or anaplastic prostate cancer, is an emerging and important condition that may arise de novo or upon transformation during hormonal therapies for men with metastatic prostate cancer. Approximately 20% of men with lethal, metastatic castration-resistant prostate cancer (mCRPC) harbor NEPC histologic findings, and many more have AVPC that is either neuroendocrine or AR negative/neuroendocrine negative or AR-independent disease, estimated to comprise at least one third of men who develop lethal disease [1,2,3]. Men with AVPC or NEPC have a much worse prognosis, with median overall survival of 7 months compared with years in men with adenocarcinoma [4]. No phase 3 studies have shown an overall survival benefit in men with AVPC or NEPC, and all approved therapies for mCRPC are only proven in patients with adenocarcinoma, highlighting the need for more effective therapies in these men with NEPC/AVPC.
The current standard-of-care for treating NEPC or AVPC and its spectrum of diseases is to start with hormonal therapies, as most NEPCs are mixed with adenocarcinoma. Once the cancer has become mCRPC or if the histology at diagnosis was small cell prostate cancer (SCPC), therapy focuses on platinum-based combination therapy. Although there are no phase 3 trials to evaluate these therapies, many patients have been treated with cisplatin and etoposide, [5,6,7] and a systematic review with a pooled analysis using all available published material on NEPC patients found that chemotherapy had a statistically significant survival benefit [4]. Consistent with this, a recent phase 1/2 clinical trial randomized patients with mCRPC to either cabazitaxel + carboplatin versus cabazitaxel alone [8]. Cabazitaxel + carboplatin led to an improvement in PFS over cabazitaxel alone. Additionally, a cohort of patients defined as having a molecular signature of AVPC was associated with an improvement in PFS and OS with the addition of carboplatin.
In addition to chemotherapy there is rationale for testing programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) inhibition in the context of NEPC. For example, in small cell lung cancer (SCLC) atezolizumab or durvalumab (PD-L1 inhibitors) in combination with a platinum agent and etoposide are the new standard-of-care for first-line treatment of SCLC in combination with up-front chemotherapy [9, 10]. Additionally, pembrolizumab [11] monotherapy and nivolumab ± ipilimumab [12] have shown efficacy in the relapsed setting; however, subsequent negative confirmatory phase III trials led to accelerated FDA approval withdrawal of both pembrolizumab and nivolumab in SCLC. In addition, NEPC tumors have a higher tumor mutational burden than typical adenocarcinoma [13] suggesting an opportunity for immunotherapy in this disease. Based on these observations we conducted the PICK-NEPC trial, a single-arm phase 2 clinical trial of single agent avelumab in NEPC/AVPC.
Methods
Study design and patients
PICK-NEPC was a single-center, prospective, single-arm phase II clinical trial conducted at Duke Cancer Institute (NCT03179410) to assess the utility of single-agent avelumab among men with NEPC/AVPC. The full protocol, including inclusion and exclusion criteria can be found in the Supplementary Methods and Supplementary Fig. 1. Eligible men were diagnosed with neuroendocrine or neuroendocrine-like prostate cancer based on histology criteria or clinical presentation criteria of AVPC. To meet histologic criteria patients needed to harbor either primary small cell carcinoma of the prostate, intermediate atypical carcinoma of the prostate, or mixed histology containing both adenocarcinoma and neuroendocrine or small cell components. To meet clinical presentation inclusion criteria of AVPC with adenocarcinoma of the prostate, but without any sign of neuroendocrine or small cell histology, patients had to be radiographically progressing despite castrate levels of testosterone (< 50 ng/ml) and have the following poor risk features:
-
(1)
Prior progression despite therapy with either abiraterone acetate and/or enzalutamide.
-
(2)
At least one of the following: (1) liver metastases; (2) bulky radiographic progression (> 2 cm short axis lymph nodes or > 1 cm long axis visceral metastases) combined with low serum PSA (<10 ng/ml); (3) high serum LDH (>1X upper limit of normal (ULN)). Patients were required to have received one line of approved chemotherapy and/or hormonal therapy and could have received up to three prior chemotherapy regimens.
Patients who previously received anti-PD(L)1 or anti-CTLA4 agents were excluded. Additional key exclusion criteria include active ongoing immunologic or autoimmune disease, immunosuppressant medication, prior organ or allogeneic stem-cell transplantation or active HIV, hepatitis B, or hepatitis C infection, active cardiovascular disease, persistent toxicity (>Grade 1) related to prior therapy, or other severe acute or chronic medical conditions such as colitis, inflammatory bowel disease, pneumonitis, or pulmonary fibrosis. All men provided informed consent under a Duke University institutional review board-approved protocol.
Study treatment
Enrolled men received avelumab (10 mg/kg by IV every 2 weeks) until progression or intolerable side effects for up to 3 years. Men were premedicated with an antihistamine and with paracetamol (acetaminophen) 30–60 min prior to each dose of avelumab. Men were continued on their ADT used at study entry per investigator with subsequent changes made per investigator. Men not on ADT at time of entry due to being purely SCPC could remain off ADT. Men with SCPC on ADT at study entry remained on ADT per investigator while all men with mixed histologies remained on active ADT during trial participation. Men on enzalutamide prior to enrollment were allowed to remain on enzalutamide during trial participation. Men were allowed to receive palliative radiation to any disease site indicated by the treating physician at any time during the study, provided that another untreated site of measurable disease was present at baseline.
Assessments
Bone scan and either CT or MRI scans of the chest, abdomen, and pelvis were performed to assess disease status at baseline as well as every eight weeks or at treatment discontinuation. Blood based biomarkers (carcinoembryonic antigen (CEA), chromogranin A, lactate dehydrogenase (LDH)) were monitored throughout the study if abnormal at baseline. Adverse events and toxicity were monitored throughout the study and for 30 days after treatment discontinuation (90 days for serious adverse events) and assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.03.
Study objectives
The primary objective of this study was to assess the efficacy of PD-L1 inhibition with avelumab as measured by a modified PCWG3 criteria, [14] where RECIST 1.1 [15] is replaced with iRECIST 1.1, a modified RECIST 1.1 for immune-based therapeutics [16], on radiographic response rate in men with metastatic neuroendocrine-like prostate cancer. Secondary endpoints included PCWG3 radiographic response rate using RECIST 1.1, rPFS using both RECIST 1.1 and iRECIST 1.1, overall survival, and the toxicities and safety of avelumab.
Analysis of clinical outcomes
This study used the optimal two-stage Simon design to test the hypothesis about modified PCWG3 using iRECIST radiologic response rate in subjects with NEPC treated with avelumab. Response was defined as a complete (CR) or partial response using iRECIST 1.1 criteria. Assuming that the response rate among subjects treated would be 5%, the trial was designed to have 88% power with a one-sided type I error rate = 5% to reject the null hypothesis of response rate of 5% when the true response rate would be 20%. The study planned a first stage in which 18 subjects would be enrolled and if one or fewer responses were observed the trial would be terminated. However, if two or more responses were observed, an additional 26 subjects would be enrolled at the second stage for a total of 44 subjects. If five or more subjects respond, this new agent would be declared to have promising activity. The probability of early termination under the null hypothesis was 0.77. These operating characteristics were selected to represent a reasonable compromise between high power, low false positive rates, and desire for small sample sizes, especially in the first stage. Allowing for 10% unevaluable rate, the target sample size was 49 subjects.
The Kaplan–Meier method was used to estimate rPFS and overall survival distributions. Summary statistics were computed for the duration of time on treatment distribution. The correlative science analyses were considered exploratory and interpreted as such.
Immune profiling
Peripheral blood immune phenotyping was performed at baseline and over time as described in the Supplementary Methods.
Results
Patient characteristics
From 12/21/2017 to 10/31/2019, 19 patients were consented and ultimately 15 patients were enrolled due to four patients screen failing as a result of not meeting all eligibility criteria (Supplementary Fig. 1B). As of 12/17/2020, date cutoff, the median follow-up time was 26 months (range 22–30). A total of 14/15 patients discontinued avelumab, most commonly due to disease progression. Baseline characteristics are shown in Table 1. The median age was 71 years (range, 51–85) with a median KPS score of 90 (range 80–100). Median PSA at baseline was 53.6 ng/ml (range, 0.0–393.0) and median LDH was 202 U/l (range, 81–330). At baseline, chromogranin A was elevated in 8/15 men (defined as >93 ng/ml, 53%), CEA was elevated in 5/15 men (defined as >2.5 ng/ml, 33%), and LDH was elevated in 8/15 men (defined as >200 U/l, 53%). Histologic diagnosis on central pathology review was adenocarcinoma for 10 patients (67%) and NEPC/small cell for 5 patients (33%). Four of the five patients classified as NEPC by pathology received prior carboplatin.
Anti-tumor activity
The median number of avelumab doses was 4 (range 2–20), and median follow-up was 26 months (range 22–30). Radiographic response is shown in Table 2. Of the 15 enrolled patients, 14 were evaluable by RECIST 1.1 and iRECIST 1.1 criteria. One patient (6.7%) showed a CR by both criteria and was found to be microsatellite instability-high by a commercial, tissue-based, next-generation sequencing panel. By iRECIST 1.1 criteria, three patients experienced stable disease, nine experienced unconfirmed progressive disease, and one experienced confirmed progression. Liver (n = 11), bone (n = 10), and lymph nodes (n = 9) were the most common sites of progression-related treatment discontinuation. One patient had treatment discontinued as a result of an adverse event, but the adverse event was unrelated to the study. The ORR for the entire study was 6.7% (95% CI 17–32%) by either criteria. Best percentage change from baseline target lesion size for 14 eligible patients is shown in Fig. 1A, and best confirmed PSA decline is shown in Fig. 1B. Two patients experienced a confirmed PSA decline from baseline. One experienced a confirmed decline of ≥30% and another by ≥90% (the same patient who achieved a CR). The study was stopped early after 15 patients were enrolled due to slow enrollment at the onset of the COVID-19 pandemic and lower than anticipated objective response rate.
Survival and progression-free survival outcomes
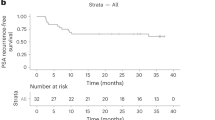
At the time of data cutoff, 13/15 (86.7%) of patients had died. Kaplan–Meier curves for overall survival and rPFS are shown in Fig. 2A, B. Median overall survival was 7.4 months (95% CI 2.8–12.6 months) and median rPFS was 1.8 months (95% CI 1.6–3.6 months).
A Kaplan–Meier estimates of overall survival during treatment with avelumab. B Kaplan–Meier estimates of radiographic progression-free survival (rPFS) using both RECIST 1.1 and iRECIST 1.1 during avelumab therapy. C Case description of exceptional responder to avelumab in a patient with MSI-H mCRPC.
Extraordinary responders
One patient experienced a CR on avelumab. His PSA trend and clinical events are shown in Fig. 2C. This man was diagnosed with prostate cancer metastatic to pelvic lymph nodes on which pathology showed 20% small cell carcinoma. Treatment with androgen deprivation therapy (ADT) and abiraterone acetate led to a decline in PSA from 34 to 1.7 ng/ml after 2 months of therapy, followed by a subsequent PSA increase to 6 ng/ml after 6 months total on ADT and abiraterone. He then presented with altered mental status and lower extremity weakness, and a brain MRI revealed a single 32 mm right frontal lobe brain mass consistent with metastasis. He underwent resection of the mass, which was consistent with prostate carcinoma. FoundationOne sequencing of this metastasis revealed microsatellite instability-high status, and a tumor mutational burden of 73 mut/Mb as well as a MSH2 splice site deletion (2451_2458 + 6del14). After completion of stereotactic body radiation therapy, he was enrolled on this study of single agent avelumab and continued on ADT. He had multiple pathologically enlarged retroperitoneal lymph nodes up to 2.6 cm and a PSA of 6 ng/ml at the start of treatment. After 2 months on ADT and avelumab his PSA declined to <0.01 ng/ml, and imaging showed CR in retroperitoneal lymph nodes after 6 months on therapy. Avelumab was discontinued 12 months after enrollment, and ADT was discontinued 18 months after enrollment based on patient preference given his CR. His PSA remains undetectable, and imaging shows no evidence of disease after testosterone recovery through October 2021, off all therapy for over 1.5 years. He did experience an episode of grade 3 pericarditis, thought to be immune related shortly after discontinuing avelumab, which resolved with prednisone.
A second patient experienced prolonged stable disease on avelumab for 9 months. The patient was diagnosed with localized prostate adenocarcinoma 17 years prior to enrollment with lung metastasis noted 9 years prior to enrollment. He was previously treated with local radiotherapy followed by ADT, sipuleucel-T, and enzalutamide for mCRPC. He had no neuroendocrine or small cell features on histology and no elevations in neuroendocrine serum biomarkers. At the time of enrollment he had PSA progression and bulky radiographic progression in lymph nodes and pulmonary nodules while on ADT and enzalutamide. He remained on enzalutamide/ADT through avelumab treatment. Imaging and PSA levels remained stable for 9 months on avelumab followed by PSA and radiographic progression in lymph nodes, after which he was treated with standard-of-care docetaxel followed by cabazitaxel.
Safety
Adverse events are reported in Table 3. Throughout the trial, all patients experienced at least one grade 1 adverse event. Three serious adverse events were attributed to avelumab, one episode of grade 3 autoimmune hepatitis, one episode of grade 4 autoimmune hepatitis, and one episode of grade 3 pericarditis. Two deaths occurred while on study, one attributed to progressive cancer and another due to thromboembolic event, neither attributed to avelumab. The safety profile was consistent with what has been previously described for avelumab.
Immune biomarkers
To characterize differences in peripheral immune subtypes in these patients over time, we used a 14-channel customized flow cytometry panel. This panel enabled the quantification of multiple immune subsets, including helper (CD3+CD4+) and cytotoxic (CD3+CD8+) T-cells, Natural Killer cells (CD3−CD16+CD56+), Natural Killer T (NKT) cells (CD3+CD56+CD16+), B cells (CD3−CD19+), monocyte lineages, including M1 (CD14+CD16−), M2 (CD14−CD16+), intermediate/transitional (CD14+CD16+), and myeloid-derived suppressor cell subsets (Lin-/HLA-DRlow/CD14+, MDSC4 (HLA-DRlow/CD14+), MDSC5 (CD15+/CD14−/CD11b+), MDSC10 (Lin−/CD14−/CD16+HLA-DR−/CD11b+) [17, 18], granulocytic (g)MDSC (CD11b+/HLA-DR−/CD14−/CD15+), and monocytic (m)MDSC (CD11b+/HLA-DR−/CD14+/CD15− [19, 20]); (Supplementary Fig. 2). CD182 (CXCR2) expression was measured on all lymphoid and myeloid populations; activation markers HLA-DR and CD279 (PD-1) were measured on all lymphocytes. Peripheral immune subsets in the patient with a CR showed no qualitative differences in the percentages of total lymphocytes, T-cells, or Helper T-cells at baseline or over time (Fig. 3A and Supplementary Fig. 3); however, this patient showed qualitatively higher levels of NKT cells (Fig. 3B) at all time points, PD-1-expressing helper T-cells (Fig. 3C) at all time points, increased levels of CXCR2+ cytotoxic T-cells that emerged over time during response (Fig. 3D) and initially low levels of CXCR2 positive monocytes, which substantially increased over time during response (Fig. 3E).
A Percentage of lymphocytes, CD3+ T-cells, and CD4+ helper T-cells. B Percentage of NK T-cells. C PD-L1+ (CD279) helper T-cells. D CXCR2+ (CD182) cytotoxic T-cells, and E CXCR2+ M1 monocytes. Line graphs show median values in solid lines while dotted lines indicate immune subsets in individual patient over time. CR complete response, PD progressive disease, SD stable disease. Beeswarm plots show all patients at each time point, with the patient exhibiting a complete response indicated in orange.
Discussion
In this phase 2 clinical trial, avelumab showed limited activity in men with metastatic NEPC/AVPC. Our objective response rate of 6.7% was similar to prior data with single agent PD-1/PD-L1 immunotherapy in men with mCRPC, and the single patient with a CR had MSH2-mutated, MSI-High NEPC. Although the number of NEPC patients is too small (n = 5) to draw a definitive conclusion on the efficacy of avelumab in this patient group, these results suggest that single agent PD-L1 checkpoint inhibition with ongoing ADT is not sufficiently active in NEPC/AVPC and is not a viable relapsed treatment option, aside from individuals with microsatellite instability.
These findings are generally consistent with prior findings for PD-(L)1 inhibition in unselected mCRPC, including the phase II KEYNOTE-199 trial [21], the IMbassador250 trial of the addition of atezolizumab to enzalutamide in mCRPC showing no benefit [22], and failure of ipilimumab to improve overall survival in a phase 3 clinical trial in mCRPC [23]. However, evidence exists that a favorable response to ipilimumab is associated with high intratumoral CD8 density, high INF-gamma response gene signature, and antigen-specific T-cell responses [24]. These insights may be similarly applicable to NEPC tumors to identify which small group of patients may respond to single agent checkpoint inhibition and further investigation into peripheral blood and tissue-based immunophenotyping to understand the underlying immune dysregulation that may underpin NEPC and mCRPC.
The chemokine receptor, CXCR2, the receptor for interleukin-8, is critical to promoting myeloid-derived suppressor cell function and resistance to immune checkpoint blockade in prostate cancer preclinical models [25,26,27]. Targeting CXCR2 is presently being tested in clinical trials of men with mCRPC and other solid tumors in combination with checkpoint blockade (NCT03473925). Interestingly, profiling of peripheral immune subsets in the present trial revealed high levels of CXCR2 (CD182) expression on cytotoxic T-cells in the one patient with a CR (Fig. 3). Consistent with this, transduction of CXCR2 increases migration of cytotoxic T-cells to tumors and enhances tumor regression in preclinical models of melanoma [28]. Conversely, baseline monocyte CXCR2 expression was lower for the patient who exhibited a CR than in other patients, but increased dramatically over time during response. This is also consistent with studies suggesting that CXCR2 knockout monocytes infused into mice with prostate cancer led to improved tumor regression and survival [29]. However, NEPC is also associated with tumor cell autonomous expression of CXCR2, which can promote lineage plasticity and AR therapy resistance [30], suggesting a complex interplay of tumor and host signaling using the same chemokine signaling axis.
This study has several limitations, including the lack of a randomized control arm, small sample size, mixture of tumor histologies included in the study, and lack of genomic profiling for all patients. However, the lack of responsiveness in all patients except the patient with microsatellite instability suggests that common genetic alterations in NEPC/AVPC, such as losses of TP53, RB1, or PTEN, may not enrich for single-agent immune checkpoint responsiveness.
In conclusion, avelumab monotherapy showed minimal efficacy in patients with relapsed NEPC/AVPC. The only objective response was in a patient with microsatellite instability-high disease. Genomic evaluation of microsatellite instability status is currently recommended in the National Comprehensive Cancer Network guidelines (v2022) as a biomarker to select patients who would benefit from immune checkpoint inhibition. The safety profile was consistent with prior investigations of avelumab without any new safety signals. Despite the lack of response as monotherapy, we believe it is reasonable to continue to pursue combination trials in men with NEPC/AVPC, and such trials are ongoing and important to the field, such as the CHAMP trial of cabazitaxel, carboplatin, nivolumab and ipilimumab (www.clinicaltrials.gov: NCT04709276). Further investigation is needed in this area to optimally select patients with prostate cancer for checkpoint inhibition as well as novel therapy combinations to improve outcomes in this aggressive disease.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary Materials.
References
Aggarwal R, Huang J, Alumkal JJ, Zhang L, Feng FY, Thomas GV, et al. Clinical and genomic characterization of treatment-emergent small-cell neuroendocrine prostate cancer: a multi-institutional prospective study. J Clin Oncol. 2018;36:2492–503.
Beltran H, Hruszkewycz A, Scher HI, Hildesheim J, Isaacs J, Yu EY, et al. The role of lineage plasticity in prostate cancer therapy resistance. Clin Cancer Res. 2019;25:6916–24.
Berchuck JE, Viscuse PV, Beltran H, Aparicio A. Clinical considerations for the management of androgen indifferent prostate cancer. Prostate Cancer Prostatic Dis. 2021;24:623–37.
Wang HT, Yao YH, Li BG, Tang Y, Chang JW, Zhang J. Neuroendocrine prostate cancer (NEPC) progressing from conventional prostatic adenocarcinoma: factors associated with time to development of NEPC and survival from NEPC diagnosis-a systematic review and pooled analysis. J Clin Oncol. 2014;32:3383–90.
Spiess PE, Pettaway CA, Vakar-Lopez F, Kassouf W, Wang X, Busby JE, et al. Treatment outcomes of small cell carcinoma of the prostate: a single-center study. Cancer. 2007;110:1729–37.
Steineck G, Reuter V, Kelly WK, Frank R, Schwartz L, Scher HI. Cytotoxic treatment of aggressive prostate tumors with or without neuroendocrine elements. Acta Oncol. 2002;41:668–74.
Nadal R, Schweizer M, Kryvenko ON, Epstein JI, Eisenberger MA. Small cell carcinoma of the prostate. Nat Rev Urol. 2014;11:213–9.
Corn PG, Heath EI, Zurita A, Ramesh N, Xiao L, Sei E, et al. Cabazitaxel plus carboplatin for the treatment of men with metastatic castration-resistant prostate cancers: a randomised, open-label, phase 1-2 trial. Lancet Oncol. 2019;20:1432–43.
Horn L, Mansfield AS, Szczesna A, Havel L, Krzakowski M, Hochmair MJ, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379:2220–9.
Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–39.
Chung HC, Piha-Paul SA, Lopez-Martin J, Schellens JHM, Kao S, Miller WH Jr., et al. Pembrolizumab after two or more lines of previous therapy in patients with recurrent or metastatic SCLC: results from the KEYNOTE-028 and KEYNOTE-158 studies. J Thorac Oncol. https://doi.org/10.1016/j.jtho.2019.12.109 (2019).
Antonia SJ, Lopez-Martin JA, Bendell J, Ott PA, Taylor M, Eder JP, et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): a multicentre, open-label, phase 1/2 trial. Lancet Oncol. 2016;17:883–95.
Beltran H, Prandi D, Mosquera JM, Benelli M, Puca L, Cyrta J, et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. Nat Med. 2016;22:298–305.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol. 2016;34:1402–18.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Seymour L, Bogaerts J, Perrone A, Ford R, Schwartz LH, Mandrekar S, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18:e143–52.
Mandruzzato S, Brandau S, Britten CM, Bronte V, Damuzzo V, Gouttefangeas C, et al. Toward harmonized phenotyping of human myeloid-derived suppressor cells by flow cytometry: results from an interim study. Cancer Immunol Immunother. 2016;65:161–9.
Zhang T, Harrison MR, O’Donnell PH, Alva AS, Hahn NM, Appleman LJ, et al. A randomized phase 2 trial of pembrolizumab versus pembrolizumab and acalabrutinib in patients with platinum-resistant metastatic urothelial. Cancer Cancer. 2020;126:4485–97.
Gabrilovich DI. Myeloid-derived suppressor cells. Cancer Immunol Res. 2017;5:3–8.
Yamauchi Y, Safi S, Blattner C, Rathinasamy A, Umansky L, Juenger S, et al. Circulating and tumor myeloid-derived suppressor cells in resectable non-small cell lung cancer. Am J Respir Crit Care Med. 2018;198:777–87.
Antonarakis ES, Piulats JM, Gross-Goupil M, Goh J, Ojamaa K, Hoimes CJ, et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: multicohort, open-label phase II KEYNOTE-199 study. J Clin Oncol. 2020;38:395–405.
Sweeney CJ, Gillessen S, Rathkopf D, Matsubara N, Drake C, Fizazi K, et al. Abstract CT014: IMbassador250: a phase III trial comparing atezolizumab with enzalutamide vs enzalutamide alone in patients with metastatic castration-resistant prostate cancer (mCRPC). Cancer Res. 2020;80:CT014.
Beer TM, Kwon ED, Drake CG, Fizazi K, Logothetis C, Gravis G, et al. Randomized, double-blind, phase III trial of ipilimumab versus placebo in asymptomatic or minimally symptomatic patients with metastatic chemotherapy-naive castration-resistant prostate cancer. J Clin Oncol. 2017;35:40–7.
Subudhi SK, Vence L, Zhao H, Blando J, Yadav SS, Xiong Q, et al. Neoantigen responses, immune correlates, and favorable outcomes after ipilimumab treatment of patients with prostate cancer. Sci Transl Med. 2020;12. https://doi.org/10.1126/scitranslmed.aaz3577.
Lopez-Bujanda ZA, Haffner MC, Chaimowitz MG, Chowdhury N, Venturini NJ, Patel RA, et al. Castration-mediated IL-8 promotes myeloid infiltration and prostate cancer progression. Nat Cancer. 2021;2:803–18.
Calcinotto A, Spataro C, Zagato E, Di Mitri D, Gil V, Crespo M, et al. IL-23 secreted by myeloid cells drives castration-resistant prostate cancer. Nature. 2018;559:363–9.
Lu X, Horner JW, Paul E, Shang X, Troncoso P, Deng P, et al. Effective combinatorial immunotherapy for castration-resistant prostate cancer. Nature. 2017;543:728–32.
Peng W, Ye Y, Rabinovich BA, Liu C, Lou Y, Zhang M, et al. Transduction of tumor-specific T cells with CXCR2 chemokine receptor improves migration to tumor and antitumor immune responses. Clin Cancer Res. 2010;16:5458–68.
Di Mitri D, Mirenda M, Vasilevska J, Calcinotto A, Delaleu N, Revandkar A, et al. Re-education of tumor-associated macrophages by CXCR2 blockade drives senescence and tumor inhibition in advanced prostate cancer. Cell Rep. 2019;28:2156–e2155.
Li Y, He Y, Butler W, Xu L, Chang Y, Lei K, et al. Targeting cellular heterogeneity with CXCR2 blockade for the treatment of therapy-resistant prostate cancer. Sci Transl Med. 2019;11. https://doi.org/10.1126/scitranslmed.aax0428.
Acknowledgements
AJA and JAS acknowledge funding support from NCI 1R01CA233585-03. The authors thank the patients and their families as well as the dedicated clinical and research staff at the Duke Cancer Institute. The authors acknowledge the efforts of Jennifer Enzor, Twan Weaver and the Duke Immune Profiling Core shared resource, and the Duke Cancer Institute biostatistics shared resource. This research was financially supported by Pfizer, as part of an alliance between Pfizer and Merck (CrossRef Funder ID:10.13039/100004755). Merck and Pfizer reviewed the manuscript for medical accuracy only before journal submission. The authors are fully responsible for the content of this manuscript, and the views and opinions described in the publication reflect solely those of the authors.
Author information
Authors and Affiliations
Contributions
LCB: writing-original draft, conceptualization, investigation. SH, JAS, and AJA: conceptualization, investigation, supervision, writing—review and editing. MH: conceptualization, writing—review and editing. YW, TO, and LH: formal analysis. JH, MRH, and TZ: investigation, writing—review and editing. MA, CD, PP, JS, and KJW: formal analysis, writing—review and editing. DJG: conceptualization, investigation, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
LCB declares the following relationships: Consulting with Seattle Genetics. SH, JAS, MH, YW, TO, LH, MA, CD, MRH, PP, JS, and KJW declare that they have no conflicts of interest that might be relevant to the contents of this manuscript. JH is a consultant for or owns shares in the following companies: Kingmed, MoreHealth, OptraScan, Genetron, Omnitura, Vetonco, York Biotechnology, Genecode, VIVA Biotech and Sisu Pharma, and received grants from Zenith Epigenetics, BioXcel Therapeutics, Inc., and Fortis Therapeutics. TZ declares the following: Research funding: Acerta, Novartis, Merrimack, Abbvie/StemCentrx, Merck, Regeneron, Mirati Therapeutics, Janssen, AstraZeneca, Pfizer, OmniSeq, Personal Genome Diagnostics, Astellas. Speaker: Sanofi-Aventis (end 2020), Genomic Health (end 2020). Advisory Board: Merck, Exelixis, Sanofi-Aventis, Janssen, AstraZeneca, Pfizer, Amgen, BMS, Pharmacyclics, SeaGen, Calithera, Eisai, Aveo. Consultant: Pfizer, MJH Associates, Vaniam Group, Aptitude Health, Nanorobotics (spouse). Employee: Capio Biosciences (spouse), Archimmune Therapeutics (spouse). Stockholder: Capio Biosciences, Archimmune Therapeutics, Nanorobotics (all spouse). DJG declares the following relationships: Acerta Pharmaceuticals—Research, American Association for Cancer Research—Sr Editor, Astellas—Consultant, Research, Advisory Board, AstraZeneca—Consultant, Advisory Board, Axess Oncology—Independent Contractor, Bayer H/C Pharmaceuticals—Research, Consultant, Speaker, Honorarium, Travel accommodations, SC, BMS—Consultant, Research, Steering Committee, Calithera—Research, Capio Biosciences—Scientific Advisory Board, EMD Serono—Honorarium, Exelixis, Inc—Research, Consultant, Speaker, Honorarium, Travel accommodations, Flatiron—Consultant, Ipsen—Honorarium, Janssen Pharmaceuticals—Research, Consultant, Independent Data Monitoring Committee (IDMC), Leidos Biomedical Research—Consultant, Merck Sharp & Dohme—Consultant, Michael J Hennessey Associates—Honorarium, Consultant, Millennium Medical Publishing, Clinical Advances in Hematology & Oncology—Co-Editor-in-Chief, Modra Pharmaceuticals B.V.—Advisory Board, Myovant Sciences, Inc—Consultant, Nektar Therapeutics—Steering Committee, Novartis—Research, Physician Education Resource LLC—Consultant, Pfizer—Research, Consultant, Steering Committee, Honorarium, Sanofi—Research, Consultant, Speaker, Honorarium, Travel accommodations, UroGPO—Honorarium, UroToday—Honorarium, Travel accommodations, Vizuri Health Sciences, LLC—Consultant, NCI—Steering Committee. AJA declares the following relationships: paid consultant with Pfizer, Astellas, Janssen, Bayer, AstraZeneca, Epic Sciences, Exelixis, Myovant, NCCN, BMS, Forma and Merck and receives research funding (to his institution) from Amgen, Forma, Celgene, Pfizer, Astellas, Janssen, Bayer, Dendreon, Novartis, Genentech/Roche, Merck, BMS, AstraZeneca, Constellation, Beigene. Steering committee for Astellas/Pfizer, AstraZeneca, BMS, Merck, Myovant.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brown, L.C., Halabi, S., Somarelli, J.A. et al. A phase 2 trial of avelumab in men with aggressive-variant or neuroendocrine prostate cancer. Prostate Cancer Prostatic Dis 25, 762–769 (2022). https://doi.org/10.1038/s41391-022-00524-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00524-7
This article is cited by
-
Immunogenomic profiles associated with response to life-prolonging agents in prostate cancer
British Journal of Cancer (2023)
-
Repurposing ketotifen as a therapeutic strategy for neuroendocrine prostate cancer by targeting the IL-6/STAT3 pathway
Cellular Oncology (2023)