Abstract
Background
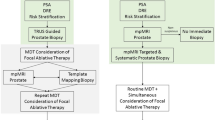
The goal of prostate cancer focal therapy is to achieve oncologic control while reducing the rate of adverse events associated with whole-gland treatments. Numerous focal therapy modalities are currently available with early data demonstrating highly variable rates of cancer control and preservation of sexual/urinary function.
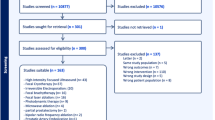
Methods
All English language clinical trial publications evaluating various focal therapies for localized prostate cancer were reviewed. The literature search was limited to studies from the modern era of MRI-guided treatment, as MRI is hypothesized to improve tumor localization and targeting. Primary outcomes were post-treatment cancer-free rates, in-field/out-of-field recurrence rates, and rates of conversion to radical therapy. Secondary outcomes were related to functional status and adverse events.
Results
Numerous focal therapies were identified with clinical data including high-intensity focused ultrasound, transurethral ultrasound ablation, focal laser ablation, focal cryotherapy, irreversible electroporation, and photodynamic therapy. Recurrence rates among all technologies were low to moderate (0–51%) and rates of freedom from radical treatment were highly variable (46–98%). Rates of erectile dysfunction and incontinence generally ranged from 0 to 44% and 0 to 12%, respectively, with variability between focal therapy modalities. Caution should be exercised when comparing studies as outcomes are strongly associated with patient selection. No individual focal therapy is currently recommended by society guidelines. Randomized controlled trials are ongoing in search of a standard of care.
Conclusion
For localized MRI-visible prostate cancer, early clinical trial data demonstrate that focal therapy can provide good to moderate cancer control while having preferable side effect profiles compared to whole-gland treatments. While current studies do not make head-to-head comparisons between technologies, early data suggest a potential for these technologies to provide adequate cancer control in a well-selected patient population. The oncologic outcomes of some focal therapies appear promising; however, longer-term follow-up data are needed to assess the durability of early outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Institute NC. SEER Cancer Stat Facts: Prostate Cancer. https://seer.cancer.gov/statfacts/html/prost.html.
Schröder FH, Hugosson J, Roobol MJ, Tammela TLJ, Zappa M, Nelen V, et al. The European randomized study of screening for prostate cancer – prostate cancer mortality at 13 years of follow-up. Lancet. 2014;384:2027.
Haglind E, Carlsson S, Stranne J, Wallerstedt A, Wilderäng U, Thorsteinsdottir T, et al. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol. 2015;68:216–25.
Ficarra V, Novara G, Ahlering TE, Costello A, Eastham JA, Graefen M, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol. 2012;62:418–30.
Schauer I, Keller E, Müller A, Madersbacher S. Have rates of erectile dysfunction improved within the past 17 years after radical prostatectomy? A systematic analysis of the control arms of prospective randomized trials on penile rehabilitation. Andrology. 2015;3:661–5.
Tilki D, Svatek RS, Novara G, Seitz M, Godoy G, Karakiewicz PI, et al. Stage pT0 at radical cystectomy confers improved survival: an international study of 4,430 patients. J Urol. 2010;184:888–94.
Ahmed HU. The index lesion and the origin of prostate cancer. N Engl J Med. 2009;361:1704–6.
Karavitakis M, Winkler M, Abel P, Livni N, Beckley I, Ahmed HU. Histological characteristics of the index lesion in whole-mount radical prostatectomy specimens: implications for focal therapy. Prostate Cancer Prostatic Dis. 2011;14:46–52.
Liu W, Laitinen S, Khan S, Vihinen M, Kowalski J, Yu G, et al. Copy number analysis indicates monoclonal origin of lethal metastatic prostate cancer. Nat Med. 2009;15:559–65.
Lebastchi AH, George AK, Polascik TJ, Coleman J, de la Rosette J, Turkbey B, et al. Standardized nomenclature and surveillance methodologies after focal therapy and partial gland ablation for localized prostate cancer: an international multidisciplinary consensus. Eur Urol. 2020;78:371–8.
Napoli A, Anzidei M, De Nunzio C, Cartocci G, Panebianco V, De Dominicis C, et al. Real-time magnetic resonance-guided high-intensity focused ultrasound focal therapy for localised prostate cancer: preliminary experience. Eur Urol. 2013;63:395–8. vol
Hildebrandt B, Wust P, Ahlers O, Dieing A, Sreenivasa G, Kerner T, et al. The cellular and molecular basis of hyperthermia. Crit Rev Oncol/Hematol. 2002;43:33–56. vol
Shoji S, Uchida T, Nakamoto M, Kim H, De Castro Abreu AL, Leslie S, et al. Prostate swelling and shift during high intensity focused ultrasound: Implication for targeted focal therapy. J Urol. 2013;190:1224–32.
Clyne M. Prostate cancer: prostatic swelling and shift upon HIFU. Nat Rev Urol. 2013;10:306. vol
Tay KJ, Cheng CWS, Lau WKO, Khoo J, Thng CH, Kwek JW. Focal therapy for prostate cancer with in-bore MR-guided focused ultrasound: two-year follow-up of a phase i trial - Complications and functional outcomes. Radiology. 2017;285:620–8.
Guillaumier S, Peters M, Arya M, Afzal N, Charman S, Dudderidge T, et al. Platinum priority-prostate cancer: a multicentre study of 5-year outcomes following focal therapy in treating clinically significant nonmetastatic prostate cancer. Eur Urol. 2018;74:422–9. https://doi.org/10.1016/j.eururo.2018.06.006.
Stabile A, Orczyk C, Hosking-Jervis F, Giganti F, Arya M, Hindley RG, et al. Medium-term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high-intensity focused ultrasonography for primary localized prostate cancer. BJU Int. 2019;124:431–40.
Johnston MJ, Emara A, Noureldin M, Bott S, Hindley RG. Focal high-intensity focussed ultrasound partial gland ablation for the treatment of localised prostate cancer: a report of medium-term outcomes from a single-center in the United Kingdom. Urology. 2019;133:175–81.
Annoot A, Olivier J, Valtille P, Deken V, Leroy X, Puech P, et al. Extra-target low-risk prostate cancer: implications for focal high-intensity focused ultrasound of clinically significant prostate cancer. World J Urol. 2019;37:261–8.
Shah T, D R, M P, D B, NH K, EG G, et al. Focal therapy compared to radical prostatectomy for non-metastatic prostate cancer: a propensity score-matched study. Prostate Cancer Prostatic Dis. 2021;24:567–74.
Bass R, Fleshner N, Finelli A, Barkin J, Zhang L, Klotz L. Oncologic and functional outcomes of partial gland ablation with high intensity focused ultrasound for localized prostate cancer. J Urol. 2019;201:113–9.
Ahmed HU, Dickinson L, Charman S, Weir S, McCartan N, Hindley RG, et al. Focal ablation targeted to the index lesion in multifocal localised prostate cancer: a prospective development study. Eur Urol. 2015;68:927–36.
Glybochko PV, Amosov AV, Krupinov GE, Petrovskii NV, Lumpov IS. Hemiablation of localized prostate cancer by high-intensity focused ultrasound: a series of 35 cases. Oncology. 2019;97:44–48.
Rosenhammer B, Niessen C, Rotzinger L, Reiss J, Schnabel MJ, Burger M, et al. Oncological outcome and value of postoperative magnetic resonance imaging after focal high-intensity focused ultrasound therapy for prostate cancer. Urol Int. 2019;103:270–8.
Huber PM, Afzal N, Arya M, Boxler S, Dudderidge T, Emberton M, et al. An exploratory study of dose escalation vs standard focal high-intensity focused ultrasound for treating nonmetastatic prostate cancer. J Endourol. 2020;34:641–6.
Nahar B, Bhat A, Reis IM, Soodana-Prakash N, Becerra MF, Lopategui D, et al. Prospective evaluation of focal high intensity focused ultrasound for localized prostate cancer. J Urol. 2020;204:483–9.
von Hardenberg J, Westhoff N, Baumunk D, Hausmann D, Martini T, Marx A, et al. Prostate cancer treatment by the latest focal HIFU device with MRI/TRUS-fusion control biopsies: a prospective evaluation. Urol Oncol Semin Orig Investig. 2018;36:401.e1–401.e9.
Ghai S, Perlis N, Lindner U, Hlasny E, Haider MA, Finelli A, et al. Magnetic resonance guided focused high frequency ultrasound ablation for focal therapy in prostate cancer – phase 1 trial. Eur Radiol. 2018;28:4281–7.
Mortezavi A, Krauter J, Gu A, Sonderer J, Bruhin J, Reeve KA, et al. Extensive histological sampling following focal therapy of clinically significant prostate cancer with high intensity focused ultrasound. J Urol. 2019;202:717–24.
Shoji S, Hiraiwa S, Uemura K, Nitta M, Hasegawa M, Kawamura Y, et al. Focal therapy with high-intensity focused ultrasound for the localized prostate cancer for Asian based on the localization with MRI-TRUS fusion image-guided transperineal biopsy and 12-cores transperineal systematic biopsy: prospective analysis of oncolog. Int J Clin Oncol. 2020;25:1844–53.
Tourinho-Barbosa RR, Sanchez-Salas R, Claros OR, Collura-Merlier S, Bakavicius A, Carneiro A, et al. Focal therapy for localized prostate cancer with either high intensity focused ultrasound or cryoablation: a single institution experience. J Urol. 2020;203:320–30.
Huber PM, Afzal N, Arya M, Boxler S, Dudderidge T, Emberton M, et al. Focal HIFU therapy for anterior compared to posterior prostate cancer lesions. World J Urol. 2021;39:1115–9.
Stabile A, Sanchez-Salas R, Tourinho-Barbosa R, Macek P, Pellegrino F, Gandaglia G, et al. Association between lesion location and oncologic outcomes after focal therapy for localized prostate cancer using either high intensity focused ultrasound or cryotherapy. J Urol. 2021;206:638–45.
Sivaraman A, Barret E. Focal therapy for prostate cancer: an ‘à la Carte’ approach. Eur Urol. 2016;69:973–5.
Lumiani A, Samun D, Sroka R, Muschter R. Single center retrospective analysis of fifty-two prostate cancer patients with customized MR-guided transurethral ultrasound ablation (TULSA). Urol Oncol Semin Orig Investig. 2021;000:0–7.
Colin P, Mordon S, Nevoux P, Marqa MF, Ouzzane A, Puech P, et al. Focal laser ablation of prostate cancer: definition, needs, and future. Adv Urol. 2012;2012:589160.
Stafford RJ, Shetty A, Elliott AM, Klumpp SA, McNichols RJ, Gowda A, et al. Magnetic resonance-guided focal laser-induced interstitial thermal therapy in a canine prostate model. J Urol. 2010;184:1514.
Cordeiro ER, Cathelineau X, Thüroff S, Marberger M, Crouzet S, De La Rosette JJMCH. High-intensity focused ultrasound (HIFU) for definitive treatment of prostate cancer. BJU Int. 2012;110:1228–42.
Natarajan S, Jones TA, Priester AM, Geoghegan R, Lieu P, Delfin M, et al. Focal laser ablation of prostate cancer: feasibility of magnetic resonance imaging-ultrasound fusion for guidance. J Urol. 2017;198:839–47.
Walser E, Nance A, Ynalvez L, Yong S, Aoughsten JS, Eyzaguirre EJ, et al. Focal laser ablation of prostate cancer: results in 120 patients with low- to intermediate-risk disease. J Vasc Interv Radiol. 2019;30:401. e2
Al-Hakeem Y, Raz O, Gacs Z, Maclean F, Varol C. Magnetic resonance image-guided focal laser ablation in clinically localized prostate cancer: safety and efficacy. ANZ J Surg. 2019;89:1610–4.
Lindner U, Weersink RA, Haider MA, Gertner MR, Davidson SRH, Atri M, et al. Image guided photothermal focal therapy for localized prostate cancer: phase I trial. J Urol. 2009;182:1371–7.
Eggener SE, Yousuf A, Watson S, Wang S, Oto A. Phase II evaluation of magnetic resonance imaging guided focal laser ablation of prostate cancer. J Urol. 2016;196:1670–5.
Rastinehad AR, Anastos H, Wajswol E, Winoker JS, Sfakianos JP, Doppalapudi SK, et al. Gold nanoshell-localized photothermal ablation of prostate tumors in a clinical pilot device study. Proc Natl Acad Sci USA. 2019;116:18590–6. https://doi.org/10.1073/pnas.1906929116.
Mehralivand S, George AK, Hoang AN, Rais-Bahrami S, Rastinehad AR, Lebastchi AH, et al. Mri-guided focal laser ablation of prostate cancer: A prospective single-arm, single-center trial with 3 years of follow-up. Diagnostic Interv. Radiology. 2021;27:394–400.
Baust JG, Gage AA, Bjerklund Johansen TE, Baust JM. Mechanisms of cryoablation: clinical consequences on malignant tumors. Cryobiology. 2014;68:1–11.
Onik G, Cobb C, Cohen J, Zabkar J, Porterfield B. US characteristics of frozen prostate. Radiology. 1988;168:629–31. https://doi.org/10.1148/radiology.168.3.3043544.
Marra G, Soeterik T, Oreggia D, Tourinho-Barbosa R, Moschini M, Filippini C, et al. Long-term outcomes of focal cryotherapy for low-to intermediate-risk prostate cancer: results and matched pair analysis with active surveillance. Eur Urol Focus. 2021;S2405–4569.
Shah TT, Peters M, Eldred-Evans D, Miah S, Yap T, Faure-Walker NA, et al. Early-medium-term outcomes of primary focal cryotherapy to treat nonmetastatic clinically significant prostate cancer from a prospective multicentre registry. Eur Urol. 2019;76:98–105. https://doi.org/10.1016/j.eururo.2018.12.030.
Sze C, Tsivian E, Tay KJ, Schulman AA, Davis LG, Gupta RT, et al. Anterior gland focal cryoablation: Proof-of-concept primary prostate cancer treatment in select men with localized anterior cancers detected by multi-parametric magnetic resonance imaging. BMC Urol. 2019;19:1–7.
Oishi M, Gill IS, Tafuri A, Shakir A, Cacciamani GE, Iwata T, et al. Hemigland cryoablation of localized low, intermediate and high risk prostate cancer: oncologic and functional outcomes at 5 years. J Urol. 2019;202:1188–98. https://doi.org/10.1097/JU.0000000000000456.
Tan WP, Chang A, Sze C, Polascik TJ. Oncological and functional outcomes of patients undergoing individualized partial gland cryoablation of the prostate: a single-institution experience. J Endourol. 2021;35:1290–9.
Mendez MH, Passoni NM, Pow-Sang J, Jones JS, Polascik TJ. Comparison of outcomes between preoperatively potent men treated with focal versus whole gland cryotherapy in a matched population. J Endourol. 2015;29:1193–8.
Valerio M, Shah TT, Shah P, Mccartan N, Emberton M, Arya M, et al. Magnetic resonance imaging-transrectal ultrasound fusion focal cryotherapy of the prostate: a prospective development study. Urol Oncol Semin Orig Investig. 2017;35:150.e1–150.e7.
Onik G, Mikus P, Rubinsky B. Irreversible electroporation: implications for prostate ablation. Technol Cancer Res Treat. 2007;6:295–300.
Davalos RV, Mir LM, Rubinsky B. Tissue ablation with irreversible electroporation. Ann Biomed Eng. 2005;33:223–31.
Guenther EI, Klein N, Zapf S, Weil S, Schlosser C, Rubinsky B, et al. Prostate cancer treatment with irreversible electroporation (IRE): safety, efficacy and clinical experience in 471 treatments. PLoS One. 2019;14:e0215093. https://doi.org/10.1371/journal.pone.0215093.
Blazevski A, Scheltema MJ, Yuen B, Masand N, Nguyen TV, Delprado W, et al. Oncological and quality-of-life outcomes following focal irreversible electroporation as primary treatment for localised prostate cancer: a biopsy-monitored prospective cohort. Eur Urol Oncol. 2020;3:283–90. https://doi.org/10.1016/j.euo.2019.04.008.
Collettini F, Enders J, Stephan C, Fischer T, Baur ADJ, Penzkofer T, et al. Image-guided irreversible electroporation of localized prostate cancer: functional and oncologic outcomes. Radiology. 2019;292:250–7.
Blazevski A, Amin A, Scheltema MJ, Balakrishnan A, Haynes A-M, Barreto D, et al. Focal ablation of apical prostate cancer lesions with irreversible electroporation (IRE). World J Urol. 2021;39:1107–14.
Giganti F, Stabile A, Giona S, Marenco J, Orczyk C, Moore CM, et al. Prostate cancer treated with irreversible electroporation: MRI-based volumetric analysis and oncological outcome. Magn Reson Imaging. 2019;58:143–7.
van den Bos W, Scheltema MJ, Siriwardana AR, Kalsbeek AMF, Thompson JE, Ting F, et al. Focal irreversible electroporation as primary treatment for localized prostate cancer. BJU Int. 2018;121:716–24.
Scheltema MJ, Chang JI, Van Den Bos W, Böhm M, Delprado W, Gielchinsky I, et al. Preliminary diagnostic accuracy of multiparametric magnetic resonance imaging to detect residual prostate cancer following focal therapy with irreversible electroporation. Eur Urol Focus. 2019;5:585–91. https://doi.org/10.1016/j.euf.2017.10.007.
Kimm SY, Tarin TV, Monette S, Srimathveeravalli G, Gerber D, Durack JC, et al. Nonthermal ablation by using intravascular oxygen radical generation with WST11: dynamic tissue effects and implications for focal therapy. Radiology. 2016;281:109–18.
Vakrat-Haglili Y, Weiner L, Brumfeld V, Brandis A, Salomon Y, McLlroy B, et al. The microenvironment effect on the generation of reactive oxygen species by Pd-bacteriopheophorbide. J Am Chem Soc. 2005;127:6487–97.
Azzouzi AR, Barret E, Moore CM, Villers A, Allen C, Scherz A, et al. TOOKAD® Soluble vascular-targeted photodynamic (VTP) therapy: determination of optimal treatment conditions and assessment of effects in patients with localised prostate cancer. BJU Int. 2013;112:766–74.
Gill IS, Azzouzi AR, Emberton M, Coleman JA, Coeytaux E, Scherz A, et al. Randomized trial of partial gland ablation with vascular targeted phototherapy versus active surveillance for low risk prostate cancer: extended followup and analyses of effectiveness. J Urol. 2018;200:786–93.
Azzouzi A-R, Vincendeau S, Barret E, Cicco A, Kleinclauss F, Van Der Poel HG, et al. Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer (CLIN1001 PCM301): an open-label, phase 3, randomised controlled trial. Lancet Oncol. 2017;18:181–91.
Flegar L, Buerk B, Proschmann R, Propping S, Groeben C, Baunacke M, et al. Vascular-targeted photodynamic therapy in unilateral low-risk prostate cancer in Germany: 2-yr single-centre experience in a real-world setting compared with radical prostatectomy. Eur Urol Focus. 2021:8;121–7.
Noweski A, Roosen A, Lebdai S, Barret E, Emberton M, Benzaghou F, et al. Medium-term follow-up of vascular-targeted photodynamic therapy of localized prostate cancer using TOOKAD soluble WST-11 (Phase II Trials). Eur Urol Focus. 2019;5:1022–8.
Centers for Medicare & Medicaid Services. Billing and Coding: Salvage High-intensity Focused Ultrasound (HIFU) Treatment in Prostate Cancer (PCa) (A56702). https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=56702&ver=14&Cntrctr=All&UpdatePeriod=488&bc=AQAAFAAAAAAA&=.
Nassiri N, Chang E, Lieu P, Priester AM, Margolis DJA, Huang J, et al. Focal therapy eligibility determined by magnetic resonance imaging/ultrasound fusion biopsy. J Urol. 2018;199:453–8.
Author information
Authors and Affiliations
Contributions
JRH was responsible for collecting and reviewing journal articles, interpreting data, creating summary tables, and writing the manuscript. AN was responsible for interpreting data, editing summary tables, and editing the manuscript. MN provided feedback on the manuscript. MA was responsible for designing the review protocol, editing summary tables, editing the manuscript, and providing feedback.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Heard, J.R., Naser-Tavakolian, A., Nazmifar, M. et al. Focal prostate cancer therapy in the era of multiparametric MRI: a review of options and outcomes. Prostate Cancer Prostatic Dis 26, 218–227 (2023). https://doi.org/10.1038/s41391-022-00501-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00501-0