Abstract
Background
Metabolic syndrome and its pharmacologic treatment can potentially influence the progression of prostate cancer in men receiving androgen deprivation therapy (ADT). We aimed to evaluate the association between metabolic syndrome and its pharmacologic treatment with time to castration-resistant prostate cancer (CRPC).
Methods
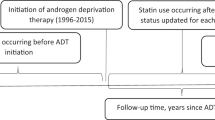
We identified 409 men with metastatic castration-sensitive prostate cancer receiving first line ADT from 1996 to 2014 at our institution. Information concerning metabolic syndrome, statin use, aspirin use, and metformin use at initiation of ADT was collected from medical records. Time to CRPC was defined as the duration between initiating ADT and diagnosis of CRPC based on the Prostate Cancer Working Group 3 definition. Flexible parametric survival models were used to calculate hazard ratios (HR, and 95% confidence intervals, CI) of the association between metabolic conditions and time from ADT initiation to CRPC.
Results
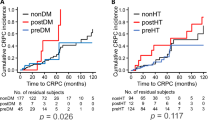
During a median follow-up of 59 months, 87% (N = 356) men progressed to CRPC. Median time to CRPC was 19 months. Fifty-six percent of men met the definition of metabolic syndrome. Controlling for demographic and prostate cancer-specific variables, metabolic syndrome was associated with shorter time to CRPC (HR 1.41, 95% CI 1.09–1.81). Importantly, in men with metabolic syndrome, statin use was associated with a slower progression to CRPC (HR 0.70, 95% CI 0.49–0.98).
Conclusions
Our study suggests that metabolic syndrome is a risk factor for earlier progression from castration-sensitive to castration-resistant prostate cancer and raises the possibility that treatment, such as statin use, may slow the time to progression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Welch HG, Albertsen PC. Reconsidering prostate cancer mortality - the future of PSA screening. N. Engl J Med. 2020;382:1557–63.
Siegel DA, O’Neil ME, Richards TB, Dowling NF, Weir HK. Prostate cancer incidence and survival, by stage and race/ethnicity - United States, 2001-2017. MMWR Morb Mortal Wkly Rep. 2020;69:1473–80.
Cook MB, Hurwitz LM, Geczik AM, Butler EN. An up-to-date assessment of US prostate cancer incidence rates by stage and race: a novel approach combining multiple imputation with age and delay adjustment. Eur Urol. 2021;79:33–41.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381:121–31.
Karantanos T, Corn PG, Thompson TC. Prostate cancer progression after androgen deprivation therapy: mechanisms of castrate resistance and novel therapeutic approaches. Oncogene. 2013;32:5501–11.
Hammarsten J, Damber JE, Haghsheno MA, Mellström D, Peeker R. A stage-dependent link between metabolic syndrome components and incident prostate cancer. Nat Rev Urol. 2018;15:321–33.
Flanagan J, Gray PK, Hahn N, Hayes J, Myers LJ, Carney-Doebbeling C, et al. Presence of the metabolic syndrome is associated with shorter time to castration-resistant prostate cancer. Ann Oncol. 2011;22:801–7.
Hammarsten J, Peeker R. Urological aspects of the metabolic syndrome. Nat Rev Urol. 2011;8:483–94.
Allott EH, Ebot EM, Stopsack KH, Gonzalez-Feliciano AG, Markt SC, Wilson KM, et al. Statin use is associated with lower risk of PTEN-null and lethal prostate cancer. Clin Cancer Res. 2020;26:1086–93.
Wu SY, Fang SC, Shih HJ, Wen YC, Shao YJ. Mortality associated with statins in men with advanced prostate cancer treated with androgen deprivation therapy. Eur J Cancer. 2019;112:109–17.
Richards KA, Liou JI, Cryns VL, Downs TM, Abel EJ, Jarrard DF. Metformin use is associated with improved survival for patients with advanced prostate cancer on androgen deprivation therapy. J Urol. 2018;200:1256–63.
He K, Hu H, Ye S, Wang H, Cui R, Yi L. The effect of metformin therapy on incidence and prognosis in prostate cancer: a systematic review and meta-analysis. Sci Rep. 2019;9:2218.
Downer MK, Allard CB, Preston MA, Wilson KM, Kenfield SA, Chan JM, et al. Aspirin use and lethal prostate cancer in the health professionals follow-up study. Eur Urol Oncol. 2019;2:126–34.
Siltari A, Murtola TJ, Talala K, Taari K, Tammela TLJ, Auvinen A. Antihypertensive drug use and prostate cancer-specific mortality in Finnish men. PloS one. 2020;15:e0234269.
Santala EE, Rannikko A, Murtola TJ. Antihypertensive drugs and prostate cancer survival after radical prostatectomy in Finland-A nationwide cohort study. Int J Cancer. 2019;144:440–7.
Penney KL, Stampfer MJ. The time is ripe for a randomized trial of metformin in clinically localized prostate cancer. J Clin Oncol. 2013;31:3054–5.
Hamilton RJ. Making sense of the statin-prostate cancer relationship: is it time for a randomized controlled trial? Eur Urol Focus. 2017;3:221–2.
Harshman LC, Wang X, Nakabayashi M, Xie W, Valenca L, Werner L, et al. Statin use at the time of initiation of androgen deprivation therapy and time to progression in patients with hormone-sensitive prostate cancer. JAMA Oncol. 2015;1:495–504.
Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2:231–7.
Deedwania P, Barter P, Carmena R, Fruchart JC, Grundy SM, Haffner S, et al. Reduction of low-density lipoprotein cholesterol in patients with coronary heart disease and metabolic syndrome: analysis of the Treating to New Targets study. Lancet. 2006;368:919–28.
Huptas S, Geiss HC, Otto C, Parhofer KG. Effect of atorvastatin (10 mg/day) on glucose metabolism in patients with the metabolic syndrome. Am J Cardiol. 2006;98:66–9.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate cancer clinical trials working group 3. J Clin Oncol. 2016;34:1402–18.
Aluwini SS, Mehra N, Lolkema MP, Oprea-Lager DE, Yakar D, Stoevelaar H, et al. Oligometastatic prostate cancer: results of a dutch multidisciplinary consensus meeting. Eur Urol Oncol. 2020;3:231–38.
Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J. 2009;9:265–90.
Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM, San Antonio Heart Study. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care. 2003;26:3153–9.
Saely CH, Koch L, Schmid F, Marte T, Aczel S, Langer P, et al. Adult Treatment Panel III 2001 but not International Diabetes Federation 2005 criteria of the metabolic syndrome predict clinical cardiovascular events in subjects who underwent coronary angiography. Diabetes Care. 2006;29:901–7.
Tong PC, Kong AP, So WY, Yang X, Ho CS, Ma RC, et al. The usefulness of the International Diabetes Federation and the National Cholesterol Education Program’s Adult Treatment Panel III definitions of the metabolic syndrome in predicting coronary heart disease in subjects with type 2 diabetes. Diabetes Care. 2007;30:1206–11.
Smith MR, Bae K, Efstathiou JA, Hanks GE, Pilepich MV, Sandler HM, et al. Diabetes and mortality in men with locally advanced prostate cancer: RTOG 92-02. J Clin Oncol. 2008;26:4333–9.
Bosco C, Wong C, Garmo H, Crawley D, Holmberg L, Hammar N, et al. Drugs for metabolic conditions and prostate cancer death in men on GnRH agonists. BJU Int. 2018;121:260–7.
Dambal S, Howard LE, Allott EH, Aronson WJ, Kane CJ, Amling CL, et al. Serum lipids prior to starting androgen deprivation therapy and risk of castration resistant prostate cancer and metastasis: results from the SEARCH database. J Urol. 2020;203:120–7.
Hirata Y, Shiota M, Kobayashi T, Kashiwagi E, Takeuchi A, Inokuchi J, et al. Prognostic significance of diabetes mellitus and dyslipidemia in men receiving androgen-deprivation therapy for metastatic prostate cancer. Prostate Int. 2019;7:166–70.
Hu MB, Yang T, Hu JM, Zhu WH, Jiang HW, Ding Q. Prognostic factors in Chinese patients with prostate cancer receiving primary androgen deprivation therapy: validation of Japan Cancer of the Prostate Risk Assessment (J-CAPRA) score and impacts of pre-existing obesity and diabetes mellitus. Int J Clin Oncol. 2018;23:591–8.
Shiota M, Takeuchi A, Sugimoto M, Kashiwagi E, Dejima T, Kiyoshima K, et al. Prognostic impact of serum testosterone and body mass index before androgen-deprivation therapy in metastatic prostate cancer. Anticancer Res. 2015;35:6925–32.
Wright JL, Plymate SR, Porter MP, Gore JL, Lin DW, Hu E, et al. Hyperglycemia and prostate cancer recurrence in men treated for localized prostate cancer. Prostate Cancer Prostatic Dis. 2013;16:204–8.
Marrone MT, Selvin E, Barber JR, Platz EA, Joshu CE. Hyperglycemia, classified with multiple biomarkers simultaneously in men without diabetes, and risk of fatal prostate cancer. Cancer Prev Res (Philos). 2019;12:103–12.
Hamilton RJ, Ding K, Crook JM, O’Callaghan CJ, Higano CS, Dearnaley DP, et al. The association between statin use and outcomes in patients initiating androgen deprivation therapy. Eur Urol. 2021;79:446–52.
Margel D, Urbach DR, Lipscombe LL, Bell CM, Kulkarni G, Austin PC, et al. Metformin use and all-cause and prostate cancer-specific mortality among men with diabetes. J Clin Oncol. 2013;31:3069–75.
Vihervuori VJ, Talala K, Taari K, Lahtela J, Tammela TLJ, Auvinen A, et al. Antidiabetic drugs and prostate cancer prognosis in a finnish population-based cohort. Cancer Epidemiol Biomark Prev. 2021;30:982–9.
Gillessen S, Gilson C, James N, Adler A, Sydes MR, Clarke N, STAMPEDE Trial Management Group. Repurposing metformin as therapy for prostate cancer within the STAMPEDE trial platform. Eur Urol. 2016;70:906–8.
Danaei G, Tavakkoli M, Hernán MA. Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol. 2012;175:250–62.
Emilsson L, García-Albéniz X, Logan RW, Caniglia EC, Kalager M, Hernán MA. Examining bias in studies of statin treatment and survival in patients with cancer. JAMA Oncol. 2018;4:63–70.
Acknowledgements
We thank Dr. Sweeney for critical review of the manuscript, Junaid Nabi and Grace Shaw for administrative assistance.
Funding
JHG was supported by a scholarship from Kaohsiung Municipal Siaogang Hospital. ASK is supported by the DiNovi Family Foundation. AP is supported by William Casey and the Swedish Society for Medical Research. LAM and KLP are supported by the Prostate Cancer Foundation.
Author information
Authors and Affiliations
Contributions
Conception and design JHG, KLP, ASK, LAM; acquisition of data MP, JHG; analysis and interpretation of data All authors; drafting of the manuscript All authors; critical revision of the manuscript for important intellectual content All authors; statistical analysis JHG, AP; obtaining funding ASK; administrative, technical, or material support ASK; supervision LAM, ASK. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki. The study was approved by the institutional IRB (Protocol No: 2018P002714). All participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Geng, JH., Plym, A., Penney, K.L. et al. Metabolic syndrome and its pharmacologic treatment are associated with the time to castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 25, 320–326 (2022). https://doi.org/10.1038/s41391-022-00494-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-022-00494-w
This article is cited by
-
The effects of diet on prostate cancer outcomes
Nature Reviews Urology (2022)