Abstract
Background
Many studies on prostate cancer (PCa) germline variants have been published in the last 15 years. This review critically assesses their clinical validity and explores their utility in prediction of PCa detection rates from prostate biopsy.
Methods
An integrative review was performed to (1) critically synthesize findings on PCa germline studies from published papers since 2016, including risk-associated single nucleotide polymorphisms (SNPs), polygenic risk score methods such as genetic risk score (GRS), and rare pathogenic mutations (RPMs); (2) exemplify the findings in a large population-based cohort from the UK Biobank (UKB); (3) identify gaps for implementing inherited risk assessment in clinic based on experience from a healthcare system; (4) evaluate available GRS data on their clinical utility in predicting PCa detection rates from prostate biopsies; and (5) describe a prospective germline-based biopsy trial to address existing gaps.
Results
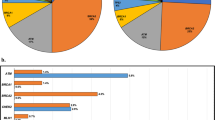
SNP-based GRS and RPMs in four genes (HOXB13, BRCA2, ATM, and CHEK2) were significantly and consistently associated with PCa risk in large well-designed studies. In the UKB, positive family history, RPMs in the four implicated genes, and a high GRS (>1.5) identified 8.12%, 1.61%, and 17.38% of men to be at elevated PCa risk, respectively, with hazard ratios of 1.84, 2.74, and 2.39, respectively. Additionally, the performance of GRS for predicting PCa detection rate on prostate biopsy was consistently supported in several retrospective analyses of transrectal ultrasound (TRUS)-biopsy cohorts. Prospective studies evaluating the performance of all three inherited measures in predicting PCa detection rate from contemporary multiparametric MRI (mpMRI)-based biopsy are lacking. A multicenter germline-based biopsy trial to address these gaps is warranted.
Conclusions
The complementary performance of three inherited risk measures in PCa risk stratification is consistently supported. Their clinical utility in predicting PCa detection rate, if confirmed in prospective clinical trials, may improve current decision-making for prostate biopsy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Amundadottir LT, Sulem P, Gudmundsson J, Helgason A, Baker A, Agnarsson BA, et al. A common variant associated with prostate cancer in European and African populations. Nat Genet. 2006;38:652–8.
Gudmundsson J, Sulem P, Manolescu A, Amundadottir LT, Gudbjartsson D, Helgason A, et al. Genome-wide association study identifies a second prostate cancer susceptibility variant at 8q24. Nat Genet. 2007;39:631–7.
Yeager M, Orr N, Hayes RB, Jacobs KB, Kraft P, Wacholder S, et al. Genome-wide association study of prostate cancer identifies a second risk locus at 8q24. Nat Genet. 2007;39:645–9.
Thomas G, Jacobs KB, Yeager M, Kraft P, Wacholder S, Orr N, et al. Multiple loci identified in a genome-wide association study of prostate cancer. Nat Genet. 2008;40:310–5.
Yeager M, Chatterjee N, Ciampa J, Jacobs KB, Gonzalez-Bosquet J, Hayes RB, et al. Identification of a new prostate cancer susceptibility locus on chromosome 8q24. Nat Genet. 2009;41:1055–7.
Gudmundsson J, Sulem P, Steinthorsdottir V, Bergthorsson JT, Thorleifsson G, Manolescu A, et al. Two variants on chromosome 17 confer prostate cancer risk, and the one in TCF2 protects against type 2 diabetes. Nat Genet. 2007;39:977–83.
Gudmundsson J, Sulem P, Rafnar T, Bergthorsson JT, Manolescu A, Gudbjartsson D, et al. Common sequence variants on 2p15 and Xp11.22 confer susceptibility to prostate cancer. Nat Genet. 2008;40:281–3.
Eeles RA, Kote-Jarai Z, Giles GG, Olama AA, Guy M, Jugurnauth SK, et al. Multiple newly identified loci associated with prostate cancer susceptibility. Nat Genet. 2008;40:316–21.
Sun J, Zheng SL, Wiklund F, Isaacs SD, Purcell LD, Gao Z, et al. Evidence for two independent prostate cancer risk-associated loci in the HNF1B gene at 17q12. Nat Genet. 2008;40:1153–5.
Al Olama AA, Kote-Jarai Z, Giles GG, Guy M, Morrison J, Severi G, et al. Multiple loci on 8q24 associated with prostate cancer susceptibility. Nat Genet. 2009;41:1058–60.
Eeles RA, Kote-Jarai Z, Al Olama AA, Giles GG, Guy M, Severi G, et al. Identification of seven new prostate cancer susceptibility loci through a genome-wide association study. Nat Genet. 2009;41:1116–21.
Gudmundsson J, Sulem P, Gudbjartsson DF, Blondal T, Gylfason A, Agnarsson BA, et al. Genome-wide association and replication studies identify four variants associated with prostate cancer susceptibility. Nat Genet. 2009;41:1122–6.
Takata R, Akamatsu S, Kubo M, Takahashi A, Hosono N, Kawaguchi T, et al. Genome-wide association study identifies five new susceptibility loci for prostate cancer in the Japanese population. Nat Genet. 2010;42:751–4.
Akamatsu S, Takata R, Haiman CA, Takahashi A, Inoue T, Kubo M, et al. Common variants at 11q12, 10q26 and 3p11.2 are associated with prostate cancer susceptibility in Japanese. Nat Genet. 2012;44:426–9. S421
Haiman CA, Chen GK, Blot WJ, Strom SS, Berndt SI, Kittles RA, et al. Genome-wide association study of prostate cancer in men of African ancestry identifies a susceptibility locus at 17q21. Nat Genet. 2011;43:570–3.
Kote-Jarai Z, Olama AA, Giles GG, Severi G, Schleutker J, Weischer M, et al. Seven prostate cancer susceptibility loci identified by a multi-stage genome-wide association study. Nat Genet. 2011;43:785–91.
Xu J, Mo Z, Ye D, Wang M, Liu F, Jin G, et al. Genome-wide association study in Chinese men identifies two new prostate cancer risk loci at 9q31.2 and 19q13.4. Nat Genet. 2012;44:1231–5.
Eeles RA, Olama AA, Benlloch S, Saunders EJ, Leongamornlert DA, Tymrakiewicz M, et al. Identification of 23 new prostate cancer susceptibility loci using the iCOGS custom genotyping array. Nat Genet. 2013;45:385–91. 391e381-382
Al Olama AA, Kote-Jarai Z, Berndt SI, Conti DV, Schumacher F, Han Y, et al. A meta-analysis of 87,040 individuals identifies 23 new susceptibility loci for prostate cancer. Nat Genet. 2014;46:1103–9.
Wang M, Takahashi A, Liu F, Ye D, Ding Q, Qin C, et al. Large-scale association analysis in Asians identifies new susceptibility loci for prostate cancer. Nat Commun. 2015;6:8469.
Hoffmann TJ, Van Den Eeden SK, Sakoda LC, Jorgenson E, Habel LA, Graff RE, et al. A large multiethnic genome-wide association study of prostate cancer identifies novel risk variants and substantial ethnic differences. Cancer Discov. 2015;5:878–91.
Conti DV, Wang K, Sheng X, Bensen JT, Hazelett DJ, Cook MB, et al. Two novel susceptibility loci for prostate cancer in men of African ancestry. J Natl Cancer Inst. 2017;109:djx084.
Schumacher FR, Al Olama AA, Berndt SI, Benlloch S, Ahmed M, Saunders EJ, et al. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat Genet. 2018;50:928–36.
Du Z, Hopp H, Ingles SA, Huff C, Sheng X, Weaver B, et al. A genome-wide association study of prostate cancer in Latinos. Int J Cancer. 2020;146:1819–26.
Conti DV, Darst BF, Moss LC, Saunders EJ, Sheng X, Chou A, et al. Trans-ancestry genome-wide association meta-analysis of prostate cancer identifies new susceptibility loci and informs genetic risk prediction. Nat Genet. 2021;53:65–75.
Zheng SL, Sun J, Wiklund F, Smith S, Stattin P, Li G, et al. Cumulative association of five genetic variants with prostate cancer. N Engl J Med. 2008;358:910–9.
Kader AK, Sun J, Reck BH, Newcombe PJ, Kim ST, Hsu FC, et al. Potential impact of adding genetic markers to clinical parameters in predicting prostate biopsy outcomes in men following an initial negative biopsy: findings from the REDUCE trial. Eur Urol. 2012;62:953–61.
Ren S, Xu J, Zhou T, Jiang H, Chen H, Liu F, et al. Plateau effect of prostate cancer risk-associated SNPs in discriminating prostate biopsy outcomes. Prostate. 2013;73:1824–35.
Jiang H, Liu F, Wang Z, Na R, Zhang L, Wu Y, et al. Prediction of prostate cancer from prostate biopsy in Chinese men using a genetic score derived from 24 prostate cancer risk-associated SNPs. Prostate. 2013;73:1651–9.
Gronberg H, Adolfsson J, Aly M, Nordstrom T, Wiklund P, Brandberg Y, et al. Prostate cancer screening in men aged 50-69 years (STHLM3): a prospective population-based diagnostic study. Lancet Oncol. 2015;16:1667–76.
Chen H, Liu X, Brendler CB, Ankerst DP, Leach RJ, Goodman PJ, et al. Adding genetic risk score to family history identifies twice as many high-risk men for prostate cancer: Results from the prostate cancer prevention trial. Prostate. 2016;76:1120–9.
Seibert TM, Fan CC, Wang Y, Zuber V, Karunamuni R, Parsons JK, et al. Polygenic hazard score to guide screening for aggressive prostate cancer: development and validation in large scale cohorts. BMJ. 2018;360:j5757.
Na R, Labbate C, Yu H, Shi Z, Fantus RJ, Wang CH, et al. Single-nucleotide polymorphism-based genetic risk score and patient age at prostate cancer diagnosis. JAMA Netw Open. 2019;2:e1918145.
Karunamuni RA, Huynh-Le MP, Fan CC, Thompson W, Eeles RA, Kote-Jarai Z, et al. African-specific improvement of a polygenic hazard score for age at diagnosis of prostate cancer. Int J Cancer. 2020;148:99–105.
Huynh-Le MP, Fan CC, Karunamuni R, Thompson WK, Martinez ME, Eeles RA, et al. Polygenic hazard score is associated with prostate cancer in multi-ethnic populations. Nat Commun. 2021;12:1236.
Yu H, Shi Z, Lin X, Bao Q, Jia H, Wei J, et al. Broad- and narrow-sense validity performance of three polygenic risk score methods for prostate cancer risk assessment. Prostate. 2020;80:83–7.
Black MH, Li S, LaDuca H, Lo M-T, Chen J, Hoiness R, et al. Validation of a prostate cancer polygenic risk score. The Prostate. 2020;80:1314–21.
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31:1748–57.
Ewing CM, Ray AM, Lange EM, Zuhlke KA, Robbins CM, Tembe WD, et al. Germline mutations in HOXB13 and prostate-cancer risk. N Engl J Med. 2012;366:141–9.
Xu J, Lange EM, Lu L, Zheng SL, Wang Z, Thibodeau SN, et al. HOXB13 is a susceptibility gene for prostate cancer: results from the International Consortium for Prostate Cancer Genetics (ICPCG). Hum Genet. 2013;132:5–14.
Karlsson R, Aly M, Clements M, Zheng L, Adolfsson J, Xu J, et al. A population-based assessment of germline HOXB13 G84E mutation and prostate cancer risk. Eur Urol. 2014;65:169–76.
Kote-Jarai Z, Mikropoulos C, Leongamornlert DA, Dadaev T, Tymrakiewicz M, Saunders EJ, et al. Prevalence of the HOXB13 G84E germline mutation in British men and correlation with prostate cancer risk, tumour characteristics and clinical outcomes. Ann Oncol. 2015;26:756–61.
Pritchard CC, Mateo J, Walsh MF, De Sarkar N, Abida W, Beltran H, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375:443–53.
Na R, Zheng SL, Han M, Yu H, Jiang D, Shah S, et al. Germline mutations in ATM and BRCA1/2 distinguish risk for lethal and indolent prostate cancer and are associated with early age at death. Eur Urol. 2017;71:740–7.
Wu Y, Yu H, Zheng SL, Na R, Mamawala M, Landis T, et al. A comprehensive evaluation of CHEK2 germline mutations in men with prostate cancer. Prostate. 2018;78:607–15.
Wokolorczyk D, Kluzniak W, Huzarski T, Gronwald J, Szymiczek A, Rusak B, et al. Mutations in ATM, NBN and BRCA2 predispose to aggressive prostate cancer in Poland. Int J Cancer. 2020;147:2793–800.
Wu Y, Yu H, Li S, Wiley K, Zheng SL, LaDuca H, et al. Rare germline pathogenic mutations of dna repair genes are most strongly associated with grade group 5 prostate cancer. Eur Urol Oncol. 2020;3:224–30.
Leongamornlert DA, Saunders EJ, Wakerell S, Whitmore I, Dadaev T, Cieza-Borrella C, et al. Germline DNA repair gene mutations in young-onset prostate cancer cases in the UK: evidence for a more extensive genetic panel. Eur Urol. 2019;76:329–37.
Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O’Leary E, et al. Prevalence of germline variants in prostate cancer and implications for current genetic testing guidelines. JAMA Oncol. 2019;5:523–8.
Pritzlaff M, Tian Y, Reineke P, Stuenkel AJ, Allen K, Gutierrez S, et al. Diagnosing hereditary cancer predisposition in men with prostate cancer. Genet Med. 2020;22:1517–23.
Momozawa Y, Iwasaki Y, Hirata M, Liu X, Kamatani Y, Takahashi A, et al. Germline pathogenic variants in 7636 Japanese patients with prostate cancer and 12,366 controls. J Natl Cancer Inst. 2020;112:369–76.
Shi Z, Platz EA, Wei J, Na R, Fantus RJ, Wang CH, et al. Performance of three inherited risk measures for predicting prostate cancer incidence and mortality: a population-based prospective analysis. Eur Urol. 2020;79:419–26.
Darst BF, Seng X, Eeles RA, Kote-Jarai Z, Conti DV, Haiman CA. Combined effect of a polygenic risk score and rare genetic variants on prostate cancer risk. Eur Urol. in press. 2021;80:134–8.
Mohler JL, Antonarakis ES, Armstrong AJ, D’Amico AV, Davis BJ, Dorff T, et al. Prostate Cancer, Version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17:479–505.
Carroll PR, Parsons JK, Andriole G, Bahnson RR, Castle EP, Catalona WJ, et al. NCCN guidelines insights: prostate cancer early detection, version 2.2016. J Natl Compr Canc Netw. 2016;14:509–19.
Grossman DC, Preventive US Services Task Force Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB. et al. Screening for Prostate Cancer: US preventive services task force recommendation statement. JAMA.2018;319:1901–13.
Bell N, Connor Gorber S, Shane A, Joffres M, Singh H, Dickinson J, et al. Recommendations on screening for prostate cancer with the prostate-specific antigen test. CMAJ. 2014;186:1225–34.
Xu J. The Xu’s chart for prostate biopsy: a visual presentation of the added value of biomarkers to prostate-specific antigen for estimating detection rates of prostate cancer. Asian J Androl. 2014;16:536–40.
Deng YS, He YH, Ying WW, Liu HL, Li PZ, Ma CY, et al. Value of three biopsy methods in prostate cancer detection: a meta-analysis and systematic review. Eur Rev Med Pharmacol Sci. 2021;25:2221–34.
Siddiqui MM, Rais-Bahrami S, Truong H, Stamatakis L, Vourganti S, Nix J, et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol. 2013;64:713–9.
Borkowetz A, Platzek I, Toma M, Laniado M, Baretton G, Froehner M, et al. Comparison of systematic transrectal biopsy to transperineal magnetic resonance imaging/ultrasound-fusion biopsy for the diagnosis of prostate cancer. BJU Int. 2015;116:873–9.
Cool DW, Romagnoli C, Izawa JI, Chin J, Gardi L, Tessier D, et al. Comparison of prostate MRI-3D transrectal ultrasound fusion biopsy for first-time and repeat biopsy patients with previous atypical small acinar proliferation. Can Urol Assoc J. 2016;10:342–8.
de Gorski A, Roupret M, Peyronnet B, Le Cossec C, Granger B, Comperat E, et al. Accuracy of magnetic resonance imaging/ultrasound fusion targeted biopsies to diagnose clinically significant prostate cancer in enlarged compared to smaller prostates. J Urol. 2015;194:669–73.
Delongchamps NB, Portalez D, Bruguiere E, Rouviere O, Malavaud B, Mozer P, et al. Are magnetic resonance imaging-transrectal ultrasound guided targeted biopsies noninferior to transrectal ultrasound guided systematic biopsies for the detection of prostate cancer? J Urol. 2016;196:1069–75.
Fiard G, Hohn N, Descotes JL, Rambeaud JJ, Troccaz J, Long JA. Targeted MRI-guided prostate biopsies for the detection of prostate cancer: initial clinical experience with real-time 3-dimensional transrectal ultrasound guidance and magnetic resonance/transrectal ultrasound image fusion. Urology. 2013;81:1372–8.
Filson CP, Natarajan S, Margolis DJ, Huang J, Lieu P, Dorey FJ, et al. Prostate cancer detection with magnetic resonance-ultrasound fusion biopsy: the role of systematic and targeted biopsies. Cancer. 2016;122:884–92.
Junker D, Schafer G, Heidegger I, Bektic J, Ladurner M, Jaschke W, et al. Multiparametric magnetic resonance imaging/transrectal ultrasound fusion targeted biopsy of the prostate: preliminary results of a prospective single-centre study. Urol Int. 2015;94:313–8.
Kulis T, Zekulic T, Alduk AM, Lusic M, Bulimbasic S, Ferencak V, et al. Targeted prostate biopsy using a cognitive fusion of multiparametric magnetic resonance imaging and transrectal ultrasound in patients with previously negative systematic biopsies and non-suspicious digital rectal exam. Croat Med J. 2020;61:49–54.
Lian H, Zhuang J, Wang W, Zhang B, Shi J, Li D, et al. Assessment of free-hand transperineal targeted prostate biopsy using multiparametric magnetic resonance imaging-transrectal ultrasound fusion in Chinese men with prior negative biopsy and elevated prostate-specific antigen. BMC Urol. 2017;17:52.
Mariotti GC, Falsarella PM, Garcia RG, Queiroz MRG, Lemos GC, Baroni RH. Incremental diagnostic value of targeted biopsy using mpMRI-TRUS fusion versus 14-fragments prostatic biopsy: a prospective controlled study. Eur Radiol. 2018;28:11–16.
Mendhiratta N, Rosenkrantz AB, Meng X, Wysock JS, Fenstermaker M, Huang R, et al. Magnetic resonance imaging-ultrasound fusion targeted prostate biopsy in a consecutive cohort of men with no previous biopsy: reduction of over detection through improved risk stratification. J Urol. 2015;194:1601–6.
Puech P, Rouviere O, Renard-Penna R, Villers A, Devos P, Colombel M, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy-prospective multicenter study. Radiology. 2013;268:461–9.
Salami SS, Ben-Levi E, Yaskiv O, Ryniker L, Turkbey B, Kavoussi LR, et al. In patients with a previous negative prostate biopsy and a suspicious lesion on magnetic resonance imaging, is a 12-core biopsy still necessary in addition to a targeted biopsy? BJU Int. 2015;115:562–70.
Vourganti S, Rastinehad A, Yerram N, Nix J, Volkin D, Hoang A, et al. Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies. J Urol. 2012;188:2152–7.
Wysock JS, Rosenkrantz AB, Huang WC, Stifelman MD, Lepor H, Deng FM, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol. 2014;66:343–51.
Zhang Q, Wang W, Yang R, Zhang G, Zhang B, Li W, et al. Free-hand transperineal targeted prostate biopsy with real-time fusion imaging of multiparametric magnetic resonance imaging and transrectal ultrasound: single-center experience in China. Int Urol Nephrol. 2015;47:727–33.
Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876–92.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–53.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Rivera-Munoz EA, Milko LV, Harrison SM, Azzariti DR, Kurtz CL, Lee K, et al. ClinGen Variant Curation Expert Panel experiences and standardized processes for disease and gene-level specification of the ACMG/AMP guidelines for sequence variant interpretation. Hum Mutat. 2018;39:1614–22.
Yu H, Shi Z, Wu Y, Wang CH, Lin X, Perschon C, et al. Concept and benchmarks for assessing narrow-sense validity of genetic risk score values. Prostate. 2019;79:1099–105.
Darst BF, Wan P, Sheng X, Bensen JT, Ingles SA, Rybicki BA, et al. A germline variant at 8q24 contributes to familial clustering of prostate cancer in men of African ancestry. Eur Urol. 2020;78:316–20.
Kader AK, Sun J, Isaacs SD, Wiley KE, Yan G, Kim ST, et al. Individual and cumulative effect of prostate cancer risk-associated variants on clinicopathologic variables in 5,895 prostate cancer patients. Prostate. 2009;69:1195–205.
Ahn J, Berndt SI, Wacholder S, Kraft P, Kibel AS, Yeager M, et al. Variation in KLK genes, prostate-specific antigen and risk of prostate cancer. Nat Genet. 2008;40:1032–4. author reply 1035-6
Parikh H, Wang Z, Pettigrew KA, Jia J, Daugherty S, Yeager M, et al. Fine mapping the KLK3 locus on chromosome 19q13.33 associated with prostate cancer susceptibility and PSA levels. Hum Genet. 2011;129:675–85.
Xu J, Isaacs SD, Sun J, Li G, Wiley KE, Zhu Y, et al. Association of prostate cancer risk variants with clinicopathologic characteristics of the disease. Clin Cancer Res. 2008;14:5819–24.
Helfand BT, Roehl KA, Cooper PR, McGuire BB, Fitzgerald LM, Cancel-Tassin G, et al. Associations of prostate cancer risk variants with disease aggressiveness: results of the NCI-SPORE Genetics Working Group analysis of 18,343 cases. Hum Genet. 2015;134:439–50.
Gallagher DJ, Vijai J, Cronin AM, Bhatia J, Vickers AJ, Gaudet MM, et al. Susceptibility loci associated with prostate cancer progression and mortality. Clin Cancer Res. 2010;16:2819–32.
Pomerantz MM, Werner L, Xie W, Regan MM, Lee GS, Sun T, et al. Association of prostate cancer risk Loci with disease aggressiveness and prostate cancer-specific mortality. Cancer Prev Res (Phila). 2011;4:719–28.
Shui IM, Lindstrom S, Kibel AS, Berndt SI, Campa D, Gerke T, et al. Prostate cancer (PCa) risk variants and risk of fatal PCa in the National Cancer Institute Breast and Prostate Cancer Cohort Consortium. Eur Urol. 2014;65:1069–75.
Khera AV, Chaffin M, Aragam KG, Haas ME, Roselli C, Choi SH, et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet. 2018;50:1219–24.
Wei J, Shi Z, Na R, Resurreccion WK, Wang CH, Duggan D, et al. Calibration of polygenic risk scores is required prior to clinical implementation: results of three common cancers in UKB. J Med Genet. 2020;59:243–7.
Ahmed M, Goh C, Saunders E, Cieza-Borrella C, consortium P, Kote-Jarai Z, et al. Germline genetic variation in prostate susceptibility does not predict outcomes in the chemoprevention trials PCPT and SELECT. Prostate Cancer Prostatic Dis. 2020;23:333–42.
Chen H, Na R, Packiam VT, Conran CA, Jiang D, Tao S, et al. Reclassification of prostate cancer risk using sequentially identified SNPs: results from the REDUCE trial. Prostate. 2017;77:1179–86.
Strande NT, Riggs ER, Buchanan AH, Ceyhan-Birsoy O, DiStefano M, Dwight SS, et al. Evaluating the clinical validity of gene-disease associations: an evidence-based framework developed by the clinical genome resource. Am J Hum Genet. 2017;100:895–906.
Ankerst DP, Boeck A, Freedland SJ, Thompson IM, Cronin AM, Roobol MJ, et al. Evaluating the PCPT risk calculator in ten international biopsy cohorts: results from the Prostate Biopsy Collaborative Group. World J Urol. 2012;30:181–7.
Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003;349:215–24.
Andriole GL, Bostwick DG, Brawley OW, Gomella LG, Marberger M, Montorsi F, et al. Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010;362:1192–202.
Xu J, Isaacs WB, Mamawala M, Shi Z, Landis P, Petkewicz J, et al. Association of prostate cancer polygenic risk score with number and laterality of tumor cores in active surveillance patients. Prostate. 2021;81:703–9.
Acknowledgements
We are grateful to the Ellrodt-Schweighauser, Chez, and Melman families for establishing Endowed Chairs of Cancer Genomic Research and Personalized Prostate Cancer Care at NorthShore University HealthSystem in support of Dr. Xu and Dr. Helfand. Likewise, the support of W.T. Gerrard, Mario Duhon, Jennifer, and John Chalsty is gratefully acknowledged by Dr. Isaacs as is the support from Bernard L. Schwartz by Dr. Pavlovich. The authors gratefully acknowledge the generous support from donors to The Patrick C. Walsh Hereditary Prostate Cancer Research Program at The Brady Urological Institute.
Author information
Authors and Affiliations
Contributions
XJ was responsible for designating the review protocol, conducting the integrative review, guiding the analysis, interpreting results, and drafting the review. WBI was responsible for designating the review protocol, conducting the integrative review, guiding the analysis, interpreting results, and revising the review. WKR was responsible for conducting the integrative review, performing the analysis, interpreting results, revising the review, and submitting the review. ZS was responsible for conducting the integrative review, performing the analysis, interpreting results, and revising the review. JW was responsible for conducting the integrative review, performing the analysis, interpreting results, and revising the review. CHW was responsible for conducting the integrative review, performing the analysis, interpreting results, and revising the review. SLZ was responsible for conducting the integrative review, interpreting results, and revising the review. PJH was responsible for conducting the integrative review, interpreting results, and revising the review. AER was responsible for conducting the integrative review, interpreting results, and revising the review. CPP was responsible for conducting the integrative review, interpreting results, and revising the review. BTH was responsible for conducting the integrative review, interpreting results, and revising the review.
Corresponding author
Ethics declarations
Competing interests
Authors Jianfeng Xu, W. Kyle Resurreccion, Zhuqing Shi, Jun Wei, S. Lilly Zheng, and Brian T. Helfand are employees of NorthShore University HealthSystem which has an agreement with GoPath Labs for genetic tests of polygenic risk score.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xu, J., Resurreccion, W.K., Shi, Z. et al. Inherited risk assessment and its clinical utility for predicting prostate cancer from diagnostic prostate biopsies. Prostate Cancer Prostatic Dis 25, 422–430 (2022). https://doi.org/10.1038/s41391-021-00458-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00458-6
This article is cited by
-
Perceived benefits and barriers to implementing precision preventive care: Results of a national physician survey
European Journal of Human Genetics (2023)