Abstract
Objective
To test whether body mass index (BMI) amongst patients with metastatic castration-resistant prostate cancer (mCRPC) is associated with overall survival (OS) and cancer-specific survival.
Methods
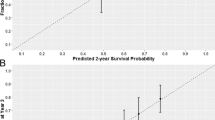
Individual patient data from 1577 men with mCRPC treated with docetaxel and prednisone from the control arms of ASCENT2, VENICE, and MAINSAIL were considered. The role of BMI on survival outcomes was investigated both as a continuous and categorical variable (≤24.9 vs. 25–29.9 vs. ≥30 km/m2). BMI ≥ 30 kg/m2 was considered obese. Analyses were adjusted for age, PSA, ECOG performance status, number of metastases and prior treatment. The Cox semi-proportional hazard model was used to predict OS, whereas competing risks regression was used for predicting cancer-specific mortality (CSM). To exclude any possible effect attributable to higher doses of chemotherapy (titrated according to body-surface area), we checked for eventual interactions between BMI and chemotherapy dose (both as continuous-continuous and categorical-continuous interactions).
Results
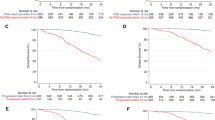
The median (IQR) age for the patient population was 69 (63,74) years with a median (IQR) BMI of 28 (25–31) kg/m2. Median follow-up for survivors was 12 months. Of the 1577 patients included, 655 were deceased by the end of the studies. Regarding OS, BMI emerged as a protective factor both as a continuous variable (HR: 0.96; 95% CI: 0.94, 0.99; p = 0.015) and as a categorical variable (obesity: HR: 0.71, 95% CI: 0.53, 0.96; p = 0.027, relatively to normal weight). The protective effect of high BMI on CSM was confirmed both as a continuous (SHR: 0.94; 95% CI: 0.91, 0.98; p = 0.002) and as a categorical variable (obesity SHR: 0.65; 95% CI: 0.45, 0.93; p = 0.018). No interaction was detected between the BMI categories and the docetaxel dose at any level in our analyses (all p » 0.05).
Conclusions
Obese patients with mCRPC had better cancer-specific and overall survival as compared to overweight and normal weight patients. The protective effect of BMI was not related to receiving higher chemotherapy doses. Further studies aimed at elucidating the biological mechanism behind this effect are warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Organization WH. Obesity https://www.who.int/topics/obesity/en/.
Steele CB, Thomas CC, Henley SJ, Massetti GM, Galuska DA, Agurs-Collins T, et al. Vital Signs: trends in Incidence of Cancers Associated with Overweight and Obesity - United States, 2005-2014. MMWR Morb Mortal Wkly Rep. 2017;66:1052–8.
Armstrong AJ, Halabi S, de Wit R, Tannock IF, Eisenberger M. The relationship of body mass index and serum testosterone with disease outcomes in men with castration-resistant metastatic prostate cancer. Prostate Cancer Prostatic Dis. 2009;12:88–93.
Cushen SJ, Power DG, Murphy KP, McDermott R, Griffin BT, Lim M, et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin Nutr ESPEN. 2016;13:e39–e45.
Halabi S, Small EJ, Vogelzang NJ. Elevated Body Mass Index Predicts for Longer Overall Survival Duration in Men With Metastatic Hormone-Refractory Prostate Cancer. J Clin Oncol. 2005;23:2434–5.
Park JM, Nam JS, Na W, Oh JJ, Lee S, Hong SK, et al. Prognostic value of body mass index in korean patients with castration-resistant prostate cancer. Korean J Urol. 2012;53:761–5.
Vidal AC, Howard LE, de Hoedt A, Kane CJ, Terris MK, Aronson WJ, et al. Obese patients with castration-resistant prostate cancer may be at a lower risk of all-cause mortality: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. BJU Int. 2018;122:76–82.
Wu W, Liu X, Chaftari P, Cruz Carreras MT, Gonzalez C, Viets-Upchurch J, et al. Association of body composition with outcome of docetaxel chemotherapy in metastatic prostate cancer: a retrospective review. PLoS One. 2015;10:e0122047.
Freedland SJ, Wen J, Wuerstle M, Shah A, Lai D, Moalej B, et al. Obesity is a significant risk factor for prostate cancer at the time of biopsy. Urology. 2008;72:1102–5.
Freedland SJ, Aronson WJ. Examining the relationship between obesity and prostate cancer. Rev Urol. 2004;6:73–81.
Vidal AC, Howard LE, Sun SX, Cooperberg MR, Kane CJ, Aronson WJ, et al. Obesity and prostate cancer-specific mortality after radical prostatectomy: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Prostate Cancer Prostatic Dis. 2017;20:72–8.
Halabi S, Ou S-S, Vogelzang NJ, Small EJ. Inverse correlation between body mass index and clinical outcomes in men with advanced castration–recurrent prostate cancer. Cancer. 2007;110:1478–84.
Lee JS, Lee HS, Ha JS, Han KS, Rha KH, Hong SJ, et al. Subcutaneous Fat Distribution is a Prognostic Biomarker for Men with Castration Resistant Prostate Cancer. J Urol. 2018;200:114–20.
Scher HI, Jia X, Chi K, de Wit R, Berry WR, Albers P, et al. Randomized, open-label phase III trial of docetaxel plus high-dose calcitriol versus docetaxel plus prednisone for patients with castration-resistant prostate cancer. J Clin Oncol. 2011;29:2191–8.
Tannock IF, Fizazi K, Ivanov S, Karlsson CT, Flechon A, Skoneczna I, et al. Aflibercept versus placebo in combination with docetaxel and prednisone for treatment of men with metastatic castration-resistant prostate cancer (VENICE): a phase 3, double-blind randomised trial. Lancet Oncol. 2013;14:760–8.
Petrylak DP, Vogelzang NJ, Budnik N, Wiechno PJ, Sternberg CN, Doner K, et al. Docetaxel and prednisone with or without lenalidomide in chemotherapy-naive patients with metastatic castration-resistant prostate cancer (MAINSAIL): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2015;16:417–25.
LLC PDS. Project Data Sphere https://www.projectdatasphere.org/projectdatasphere/html/home.
Albiges L, Hakimi AA, Xie W, McKay RR, Simantov R, Lin X, et al. Body Mass Index and Metastatic Renal Cell Carcinoma: clinical and Biological Correlations. J Clin Oncol. 2016;34:3655–63.
McQuade JL, Daniel CR, Hess KR, Mak C, Wang DY, Rai RR, et al. Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncol. 2018;19:310–22.
Nguyen PL, Ma J, Chavarro JE, Freedman ML, Lis R, Fedele G, et al. Fatty acid synthase polymorphisms, tumor expression, body mass index, prostate cancer risk, and survival. J Clin Oncol. 2010;28:3958–64.
Donnelly D, Bajaj S, Yu J, Hsu M, Balar A, Pavlick A, et al. The complex relationship between body mass index and response to immune checkpoint inhibition in metastatic melanoma patients. J Immunother Cancer. 2019;7:222.
Wang Z, Aguilar EG, Luna JI, Dunai C, Khuat LT, Le CT, et al. Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat Med. 2019;25:141–51.
Desmedt C, Fornili M, Clatot F, Demicheli R, De Bortoli D, Di Leo A, et al. Differential Benefit of Adjuvant Docetaxel-Based Chemotherapy in Patients With Early Breast Cancer According to Baseline Body Mass Index. J Clin Oncol. 2020;38:2883–91.
Utech AE, Tadros EM, Hayes TG, Garcia JM. Predicting survival in cancer patients: the role of cachexia and hormonal, nutritional and inflammatory markers. J Cachexia Sarcopenia Muscle. 2012;3:245–51.
Banack HR, Kaufman JS. The obesity paradox: understanding the effect of obesity on mortality among individuals with cardiovascular disease. Prev Med. 2014;62:96–102.
Banack HR, Kaufman JS. The “obesity paradox” explained. Epidemiology. 2013;24:461–2.
Martini A, Parikh AB, Sfakianos JP, Montorsi F, Galsky MD, Oh WK, et al. Predicting toxicity-related docetaxel discontinuation and overall survival in metastatic castration-resistant prostate cancer: a pooled analysis of open phase 3 clinical trial data. Prostate Cancer Prostatic Dis. 2021. https://pubmed.ncbi.nlm.nih.gov/33531652/.
Acknowledgements
This publication is based on research using information obtained from www.ProjectDataSphere.org, which is maintained by Project Data Sphere, LLC. Neither Project Data Sphere, LLC nor the owner(s) of any information from the web site have contributed to, approved or are in any way responsible for the contents of this publication. EJG received salary support from NIH/NCI K08CA190770.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MDG has served as consultant for BioMotiv, Janssen, Merk, Dendreon, GlaxoSmithKline, Lilly, Astellas, Genetech, BMS, Novartis, Pfizer, EMD Serono, AZ, Seattle Genetics, Incyte, Aileron Therapeutics, Dracen, Inovio Pharmaceuticals, NuMab, has received research funding from Janssen, Merk, Dendreon, Novartis, BMS, AZ, Genentech/Roche, and owns stock of Rapt Therapeutics, outside the submitted work. AN has served as a consultant for Merck, Astra Zeneca, Janssen, Incyte, Roche, Rainier Therapeutics, Clovis Oncology, Bayer, and Astellas/Seattle Genetics, Ferring, Immunomedics. has received research funding from Merck, Ipsen, and Astra Zeneca. has received Travel expenses/Honoraria from Roche, Merck, Astra Zeneca, and Janssen.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Martini, A., Shah, Q.N., Waingankar, N. et al. The obesity paradox in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 25, 472–478 (2022). https://doi.org/10.1038/s41391-021-00418-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-021-00418-0
This article is cited by
-
A healthy diet, a healthy prostate? A brief commentary on the latest research on diet and prostate cancer
Prostate Cancer and Prostatic Diseases (2023)
-
Survival of veterans treated with enzalutamide and abiraterone for metastatic castrate resistant prostate cancer based on comorbid diseases
Prostate Cancer and Prostatic Diseases (2023)