Abstract
Background
The safety of testosterone therapy (TT) after definitive treatment for localized prostate cancer remains undefined. We analyzed the risks of biochemical recurrence and mortality in men receiving TT after treatment for localized prostate cancer.
Methods
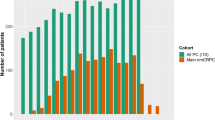
Cohort analysis using the national US Veterans Affairs Informatics and Computing Infrastructure. We identified 69,984 patients with localized prostate cancer diagnosed from 2001 to 2015 treated with surgery or radiation. We coded receipt of TT after treatment as a time-dependent covariate; used the National Death Index to identify cause of death; and defined biochemical recurrence as PSA > 0.2 ng/mL after surgery and nadir + 2 ng/mL after radiation. We analyzed recurrence and mortality using cumulative incidence curves, Fine–Gray competing risk regression, and Cox regression.
Results
This cohort included 28,651 surgery patients and 41,333 radiation patients, of whom 469 (1.64%) and 543 (1.31%), respectively, received TT with a median follow-up of 6.95 years. Comparing testosterone users to nonusers, there were no between-group differences in biochemical recurrence, prostate cancer-specific mortality, or overall mortality after surgery [hazard ratios (HR): 1.07; HR: 0.72 (p = 0.43); and HR: 1.11 (p = 0.43), respectively] or radiation [HR: 1.07; HR: 1.02 (p = 0.95); and HR: 1.02 (p = 0.86), respectively]. Limitations included lack of detailed data on TT duration and serum testosterone concentrations.
Conclusions
In this multi-ethnic national cohort, TT did not increase the risks of biochemical recurrence or prostate cancer-specific or overall mortality after surgery or radiation. These data suggest that TT is safe in appropriate men after definitive treatment of localized prostate cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Araujo AB, Esche GR, Kupelian V, O’Donnell AB, Travison TG, Williams RE, et al. Prevalence of symptomatic androgen deficiency in men. J Clin Endocrinol Metab. 2007;92:4241–7. https://doi.org/10.1210/jc.2007-1245.
Wu FCW, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123–35. https://doi.org/10.1056/NEJMoa0911101.
Corona G, Giagulli VA, Maseroli E, Vignozzi L, Aversa A, Zitzmann M, et al. Therapy of endocrine disease: testosterone supplementation and body composition: results from a meta-analysis study. Eur J Endocrinol. 2016;174:R99–116.
Hackett G. An update on the role of testosterone replacement therapy in the management of hypogonadism. Ther Adv Urol. 2016;8:147–60. https://doi.org/10.1177/1756287215617648.
Fowler JEJ, Whitmore WFJ. The response of metastatic adenocarcinoma of the prostate to exogenous testosterone. J Urol. 1981;126:372–5. https://doi.org/10.1016/s0022-5347(17)54531-0.
Perlmutter MA, Lepor H. Androgen deprivation therapy in the treatment of advanced prostate cancer. Rev Urol. 2007;9 (Suppl 1) :S3–8.
FDA. Highlights of prescribing information on testosterone. 2009. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021015s022lbl.pdf.
Kaufman JM, Graydon RJ. Androgen replacement after curative radical prostatectomy for prostate cancer in hypogonadal MEN. J Urol. 2004;172:920–2. https://doi.org/10.1097/01.ju.0000136269.10161.32.
Agarwal PK, Oefelein MG. Testosterone replacement therapy after primary treatment for prostate cancer. J Urol. 2005;173:533–6. https://doi.org/10.1097/01.ju.0000143942.55896.64.
Pastuszak AW, Khanna A, Badhiwala N, Morgentaler A, Hult M, Conners WP, et al. Testosterone therapy after radiation therapy for low, intermediate and high risk prostate cancer. J Urol. 2015;194:1271–6. https://doi.org/10.1016/j.juro.2015.05.084
Sarosdy MF. Testosterone replacement for hypogonadism after treatment of early prostate cancer with brachytherapy. Cancer. 2007;109:536–41. https://doi.org/10.1002/cncr.22438.
Kaplan AL, Trinh Q, Sun M, Carter SC, Nguyen PL, Shih YT, et al. Testosterone replacement therapy following the diagnosis of prostate cancer: outcomes and utilization trends. J Sex Med. 2014;11:1063–70. https://doi.org/10.1111/jsm.12429.
EUA. Male hypogonadism. 2012. https://uroweb.org/guideline/male-hypogonadism/#5_5.
Mulhall JP, Trost LW, Brannigan RE, Kurtz EG, Redmon JB, Chiles KA, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018;200:423–32. https://doi.org/10.1016/j.juro.2018.03.115.
Duvall S. What is VINCI? 2016. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=1143. Accessed 10 Nov 2016.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–67. https://doi.org/10.1016/s0895-4356(00)00256-0.
Paller CJ, Antonarakis ES. Management of biochemically recurrent prostate cancer after local therapy: evolving standards of care and new directions. Clin Adv Hematol Oncol. 2013;11:14–23.
Cookson MS, Aus G, Burnett AL, Canby-Hagino ED, D’Amico AV, Dmochowski RR, et al. Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol. 2007;177:540–5. https://doi.org/10.1016/j.juro.2006.10.097.
Loeb S, Folkvaljon Y, Damber J-E, Alukal J, Lambe M, Stattin P. Testosterone replacement therapy and risk of favorable and aggressive prostate cancer. J Clin Oncol. 2017;35:1430–6. https://doi.org/10.1200/JCO.2016.69.5304.
Ragde H, Elgamal AA, Snow PB, Brandt J, Bartolucci AA, Nadir BS, et al. Ten-year disease free survival after transperineal sonography-guided iodine-125 brachytherapy with or without 45-gray external beam irradiation in the treatment of patients with clinically localized, low to high Gleason grade prostate carcinoma. Cancer. 1998;83:989–1001.
Critz FA, Williams WH, Levinson AK, Benton JB, Schnell FJ, Holladay CT, et al. Prostate specific antigen bounce after simultaneous irradiation for prostate cancer: the relationship to patient age. J Urol. 2003;170:1864–7. https://doi.org/10.1097/01.ju.0000091644.41330.2a.
Akyol F, Ozyigit G, Selek U, Karabulut E. PSA Bouncing after short term androgen deprivation and 3D-conformal radiotherapy for localized prostate adenocarcinoma and the relationship with the kinetics of testosterone. Eur Urol. 2005;48:40–5. https://doi.org/10.1016/j.eururo.2005.04.007.
Murtola TJ, Kujala PM, Tammela TLJ. High-grade prostate cancer and biochemical recurrence after radical prostatectomy among men using 5alpha-reductase inhibitors and alpha-blockers. Prostate. 2013;73:923–31. https://doi.org/10.1002/pros.22638.
Acknowledgements
This work was supported by the National Institutes of Health (Grant Number TL1TR001443 to RRS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sarkar, R.R., Patel, S.H., Parsons, J.K. et al. Testosterone therapy does not increase the risks of prostate cancer recurrence or death after definitive treatment for localized disease. Prostate Cancer Prostatic Dis 23, 689–695 (2020). https://doi.org/10.1038/s41391-020-0241-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0241-3