Abstract
Background
Molecular and immunohistochemistry-based profiling of prostatic adenocarcinoma has revealed frequent Androgen Receptor (AR) gene and protein alterations in metastatic disease. This includes an AR-null non-neuroendocrine phenotype of metastatic castrate resistant prostate cancer which may be less sensitive to androgen receptor signaling inhibitors. This AR-null non-neuroendocrine phenotype is thought to be associated with TP53 and RB1 alterations. Herein, we have correlated molecular profiling of metastatic castrate resistant prostate cancer with AR/P53/RB immunohistochemistry and relevant clinical correlates.
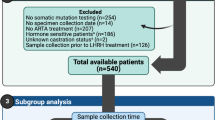
Design
Twenty-seven cases of metastatic castrate resistant prostate cancer were evaluated using histopathologic examination to rule out neuroendocrine differentiation. A combination of a hybridization exon-capture next-generation sequencing-based assay (n = 26), fluorescence in situ hybridization for AR copy number status (n = 16), and immunohistochemistry for AR (n = 27), P53 (n = 24) and RB (n = 25) was used to profile these cases.
Results
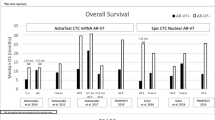
Of 27 metastatic castrate resistant prostate cancer cases, 17 had AR amplification and showed positive nuclear expression of AR by immunohistochemistry. Nine cases lacked AR copy number alterations using next-generation sequencing/fluorescence in situ hybridization. A subset of these metastatic castrate resistant prostate cancer cases demonstrated the AR-null phenotype by immunohistochemistry (five cases and one additional case where next-generation sequencing failed). Common co-alterations in these cases involved the TP53, RB1, and PTEN genes and all these patients received prior therapy with androgen receptor signaling inhibitors (abiraterone and/or enzalutamide).
Conclusions
Our study suggests that AR immunohistochemistry may distinguish AR-null from AR-expressing cases in the metastatic setting. AR-null status informs clinical decision-making regarding continuation of therapy with androgen receptor signaling inhibitors and consideration of other treatment options. This might be a relevant and cost-effective diagnostic strategy when there is limited access and/or limited tumor material for molecular testing.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Crawford ED, Higano CS, Shore ND, Hussain M, Petrylak DP. Treating patients with metastatic castration resistant prostate cancer: a comprehensive review of available therapies. J Urol. 2015;194:1537–47.
Wale DJ, Viglianti BL, Gross MD, Ferretti A, Rubello D, Wong KK. Nuclear medicine therapy with 223radium-dichloride for osseous metastases in prostate carcinoma. Am J Clin Oncol. 2019;42:99–106.
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl J Med. 2010;363:411–22.
Bluemn EG, Coleman IM, Lucas JM, Coleman RT, Hernandez-Lopez S, Tharakan R, et al. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. Cancer Cell. 2017;32:474–89. e476.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the prostate Cancer Clinical Trials Working Group 3. J Clin Oncol. 2016;34:1402–18.
Abida W, Armenia J, Gopalan A, Brennan R, Walsh M, Barron D et al. Prospective genomic profiling of prostate cancer across disease states reveals germline and somatic alterations that may affect clinical decision making. JCO Precis Oncol. 2017;1:1–26.
Abida W, Cyrta J, Heller G, Prandi D, Armenia J, Coleman I, et al. Genomic correlates of clinical outcome in advanced prostate cancer. Proc Natl Acad Sci USA. 2019;116:11428–36.
Aggarwal R, Huang J, Alumkal JJ, Zhang L, Feng FY, Thomas GV, et al. Clinical and genomic characterization of treatment-emergent small-cell neuroendocrine prostate cancer: a multi-institutional prospective study. J Clin Oncol. 2018;36:2492–503.
Davies AH, Beltran H, Zoubeidi A. Cellular plasticity and the neuroendocrine phenotype in prostate cancer. Nat Rev Urol. 2018;15:271–86.
Cheng DT, Mitchell TN, Zehir A, Shah RH, Benayed R, Syed A, et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J Mol Diagn. 2015;17:251–64.
Hyman DM, Solit DB, Arcila ME, Cheng DT, Sabbatini P, Baselga J, et al. Precision medicine at Memorial Sloan Kettering Cancer Center: clinical next-generation sequencing enabling next-generation targeted therapy trials. Drug Discov Today. 2015;20:1422–8.
Zehir A, Benayed R, Shah RH, Syed A, Middha S, Kim HR, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23:703–13.
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 2013;6:pl1–pl1.
Epstein JI, Amin MB, Beltran H, Lotan TL, Mosquera JM, Reuter VE, et al. Proposed morphologic classification of prostate cancer with neuroendocrine differentiation. Am J Surg Pathol. 2014;38:756–67.
Gupta S, Cheville JC, Jungbluth AA, Zhang Y, Zhang L, Chen YB et al. JAK2/PD-L1/PD-L2 (9p24.1) amplifications in renal cell carcinomas with sarcomatoid transformation: implications for clinical management. Mod Pathol. 2019;32:1344–58.
Gupta S, Vanderbilt CM, Cotzia P, Arias-Stella JA 3rd, Chang JC, Zehir A, et al. Next-generation sequencing-based assessment of JAK2, PD-L1, and PD-L2 copy number alterations at 9p24.1 in breast cancer: potential implications for clinical management. J Mol Diagn. 2019;21:307–17.
Ross DS, Zehir A, Cheng DT, Benayed R, Nafa K, Hechtman JF, et al. Next-generation assessment of human epidermal growth factor receptor 2 (ERBB2) amplification status: clinical validation in the context of a hybrid capture-based, comprehensive solid tumor genomic profiling assay. J Mol Diagn. 2017;19:244–54.
Yemelyanova A, Vang R, Kshirsagar M, Lu D, Marks MA, Shih Ie M, et al. Immunohistochemical staining patterns of p53 can serve as a surrogate marker for TP53 mutations in ovarian carcinoma: an immunohistochemical and nucleotide sequencing analysis. Mod Pathol. 2011;24:1248–53.
Tan HL, Sood A, Rahimi HA, Wang W, Gupta N, Hicks J, et al. Rb loss is characteristic of prostatic small cell neuroendocrine carcinoma. Clin Cancer Res. 2014;20:890–903.
Beltran H, Yelensky R, Frampton GM, Park K, Downing SR, MacDonald TY, et al. Targeted next-generation sequencing of advanced prostate cancer identifies potential therapeutic targets and disease heterogeneity. Eur Urol. 2013;63:920–6.
Aparicio AM, Shen L, Tapia EL, Lu JF, Chen HC, Zhang J, et al. Combined tumor suppressor defects characterize clinically defined aggressive variant prostate cancers. Clin Cancer Res. 2016;22:1520–30.
Tao DL, Bailey S, Beer TM, Foss E, Beckett B, Fung A, et al. Molecular testing in patients with castration-resistant prostate cancer and its impact on clinical decision making. JCO Precis Oncol. 2017;1:1–11.
Hamid AA, Gray KP, Shaw G, MacConaill LE, Evan C, Bernard B, et al. Compound genomic alterations of TP53, PTEN, and RB1 tumor suppressors in localized and metastatic prostate cancer. Eur Urol. 2019;76:89–97.
Watson PA, Arora VK, Sawyers CL. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat Rev Cancer. 2015;15:701–11.
Takeda DY, Spisak S, Seo JH, Bell C, O’Connor E, Korthauer K, et al. A somatically acquired enhancer of the androgen receptor is a noncoding driver in advanced prostate cancer. Cell. 2018;174:422–32. e413.
Antonarakis ES, Lu C, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl J Med. 2014;371:1028–38.
Scher HI, Graf RP, Schreiber NA, McLaughlin B, Lu D, Louw J, et al. Nuclear-specific AR-V7 protein localization is necessary to guide treatment selection in metastatic castration-resistant prostate cancer. Eur Urol. 2017;71:874–82.
Conteduca V, Wetterskog D, Sharabiani MTA, Grande E, Fernandez-Perez MP, Jayaram A, et al. Androgen receptor gene status in plasma DNA associates with worse outcome on enzalutamide or abiraterone for castration-resistant prostate cancer: a multi-institution correlative biomarker study. Ann Oncol. 2017;28:1508–16.
Annala M, Vandekerkhove G, Khalaf D, Taavitsainen S, Beja K, Warner EW, et al. Circulating tumor DNA genomics correlate with resistance to abiraterone and enzalutamide in prostate cancer. Cancer Discov. 2018;8:444–57.
Roudier MP, True LD, Higano CS, Vesselle H, Ellis W, Lange P, et al. Phenotypic heterogeneity of end-stage prostate carcinoma metastatic to bone. Hum Pathol. 2003;34:646–53.
Shah RB, Mehra R, Chinnaiyan AM, Shen R, Ghosh D, Zhou M, et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. Cancer Res. 2004;64:9209–16.
Wang W, Epstein JI. Small cell carcinoma of the prostate. A morphologic and immunohistochemical study of 95 cases. Am J Surg Pathol. 2008;32:65–71.
Scher HI, Graf RP, Schreiber NA, McLaughlin B, Jendrisak A, Wang Y, et al. Phenotypic heterogeneity of circulating tumor cells informs clinical decisions between AR signaling inhibitors and taxanes in metastatic prostate cancer. Cancer Res. 2017;77:5687–98.
Fox JJ, Gavane SC, Blanc-Autran E, Nehmeh S, Gonen M, Beattie B, et al. Positron emission tomography/computed tomography-based assessments of androgen receptor expression and glycolytic activity as a prognostic biomarker for metastatic castration-resistant prostate cancer. JAMA Oncol. 2018;4:217–24.
Acknowledgements
The authors would like to thank Irina Ostrovnaya and Marina Asher from the Precision Pathology Biobanking Center (PPBC) at Memorial Sloan Kettering Cancer Center, New York, NY for technical assistance as well as Jennifer Posada and Christine Moon for administrative assistance.
Funding
This study was supported in part through NIH/NCI Prostate Cancer SPORE Award P50CA092629 (MSKCC), NIH/NCI Cancer Center Support grant P30CA008748, CDMRP Prostate Cancer Research Program Award W81XWH-12-PCRP-TIA (to AG, VER, and HS), CDMRP W81XWH-14-2-0186 and Prostate Cancer Biorepository Network-PCRP Pathology Resource Network Award (to AG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gupta, S., Vanderbilt, C., Abida, W. et al. Immunohistochemistry-based assessment of androgen receptor status and the AR-null phenotype in metastatic castrate resistant prostate cancer. Prostate Cancer Prostatic Dis 23, 507–516 (2020). https://doi.org/10.1038/s41391-020-0214-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0214-6
This article is cited by
-
Genomic and Phenotypic Biomarkers for Precision Medicine Guidance in Advanced Prostate Cancer
Current Treatment Options in Oncology (2023)
-
Adjuvant enzalutamide for the treatment of early-stage androgen-receptor positive, triple-negative breast cancer: a feasibility study
Breast Cancer Research and Treatment (2022)