Abstract
Background and objective
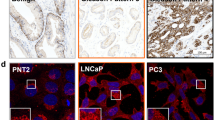
Our patient cohort revealed that obesity is strongly associated with steroid-5α reductase type 2 (SRD5A2) promoter methylation and reduced protein expression. The underlying mechanism of prostatic growth in this population is poorly understood. Here we addressed the question of how obesity, inflammation, and steroid hormones affect the development of benign prostatic hyperplasia (BPH).
Material and methods
We used preadipocytes, macrophages, primary human prostatic stromal cells, prostate tissues from high-fat diet-induced obese mice, and 35 prostate specimens that were collected from patients who underwent transurethral resection of the prostate (TURP). RNA was isolated and quantified with RT-PCR. Genome DNA was extracted and SRD5A2 promoter methylation was determined. Sex hormones were determined by high-performance liquid chromatography–tandem mass spectrometry. Protein was extracted and determined by ELISA test.
Results
In prostatic tissues with obesity, the levels of inflammatory mediators were elevated. SRD5A2 promoter methylation was promoted, but SRD5A2 expression was inhibited. Inflammatory mediators and saturated fatty acid synergistically regulated aromatase activity. Obesity promoted an androgenic to estrogenic switch in the prostate.
Conclusions
Our findings suggest that obesity-associated inflammation induces androgenic to estrogenic switch in the prostate gland, which may serve as an effective strategy for alternative therapies for management of lower urinary tract symptoms associated with BPH in select individuals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Saigal CS, Joyce G. Economic costs of benign prostatic hyperplasia in the private sector. J Urol. 2005;173:1309–13.
McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. Finasteride Long-Term Efficacy and Safety Study Group. N Engl J Med. 1998;338:557–63.
Wang Z, Hu L, Salari K, Bechis SK, Ge R, Wu S, et al. Androgenic to oestrogenic switch in the human adult prostate gland is regulated by epigenetic silencing of steroid 5alpha-reductase 2. J Pathol. 2017;243:457–67.
Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW. Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol. 2002;168:599–604.
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7.
Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31:219–30.
Giri A, Edwards TL, Motley SS, Byerly SH, Fowke JH. Genetic determinants of metabolism and benign prostate enlargement: associations with prostate volume. PloS ONE. 2015;10:e0132028.
Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016;13:108–19.
Jasuja GK, Travison TG, Davda M, Murabito JM, Basaria S, Zhang A, et al. Age trends in estradiol and estrone levels measured using liquid chromatography tandem mass spectrometry in community-dwelling men of the Framingham Heart Study. J Gerontol Ser A Biol Sci Med Sci. 2013;68:733–40.
Fowke JH, Koyama T, Fadare O, Clark PE. Does inflammation mediate the obesity and BPH relationship? An epidemiologic analysis of body composition and inflammatory markers in blood, urine, and prostate tissue, and the relationship with prostate enlargement and lower urinary tract symptoms. PloS ONE. 2016;11:e0156918.
Bechis SK, Otsetov AG, Ge R, Wang Z, Vangel MG, Wu CL, et al. Age and obesity promote methylation and suppression of 5-alpha reductase 2-implications for personalized therapy in benign prostatic hyperplasia. J Urol. 2015;194:1031–7.
Goldstein AS, Drake JM, Burnes DL, Finley DS, Zhang H, Reiter RE, et al. Purification and direct transformation of epithelial progenitor cells from primary human prostate. Nat Protoc. 2011;6:656–67.
Strand DW, Aaron L, Henry G, Franco OE, Hayward SW. Isolation and analysis of discreet human prostate cellular populations. Differ; Res Biol Divers. 2016;91:139–51.
Zhang B, Kwon OJ, Henry G, Malewska A, Wei X, Zhang L, et al. Non-cell-autonomous regulation of prostate epithelial homeostasis by androgen receptor. Mol Cell. 2016;63:976–89.
Kwon OJ, Zhang B, Zhang L, Xin L. High fat diet promotes prostatic basal-to-luminal differentiation and accelerates initiation of prostate epithelial hyperplasia originated from basal cells. Stem Cell Res. 2016;16:682–91.
Nguyen MT, Favelyukis S, Nguyen AK, Reichart D, Scott PA, Jenn A, et al. A subpopulation of macrophages infiltrates hypertrophic adipose tissue and is activated by free fatty acids via Toll-like receptors 2 and 4 and JNK-dependent pathways. J Biol Chem. 2007;282:35279–92.
Perreault M, Roke K, Badawi A, Nielsen DE, Abdelmagid SA, El-Sohemy A, et al. Plasma levels of 14:0, 16:0, 16:1n-7, and 20:3n-6 are positively associated, but 18:0 and 18:2n-6 are inversely associated with markers of inflammation in young healthy adults. Lipids. 2014;49:255–63.
Ge R, Wang Z, Bechis SK, Otsetov AG, Hua S, Wu S, et al. DNA methyl transferase 1 reduces expression of SRD5A2 in the aging adult prostate. Am J Pathol. 2015;185:870–82.
Polari L, Yatkin E, Martinez Chacon MG, Ahotupa M, Smeds A, Strauss L, et al. Weight gain and inflammation regulate aromatase expression in male adipose tissue, as evidenced by reporter gene activity. Mol Cell Endocrinol. 2015;412:123–30.
Majumdar S, Rinaldi JC, Malhotra NR, Xie L, Hu DP, Gauntner TD, et al. Differential actions of estrogen receptor alpha and beta via nongenomic signaling in human prostate stem and progenitor cells. Endocrinology. 2019;160:2692–708.
Benton MC, Johnstone A, Eccles D, Harmon B, Hayes MT, Lea RA, et al. An analysis of DNA methylation in human adipose tissue reveals differential modification of obesity genes before and after gastric bypass and weight loss. Genome Biol. 2015;16:8.
Dick KJ, Nelson CP, Tsaprouni L, Sandling JK, Aissi D, Wahl S, et al. DNA methylation and body-mass index: a genome-wide analysis. Lancet. 2014;383:1990–8.
Dobosy JR, Roberts JL, Fu VX, Jarrard DF. The expanding role of epigenetics in the development, diagnosis and treatment of prostate cancer and benign prostatic hyperplasia. J Urol. 2007;177:822–31.
Lin-Tsai O, Clark PE, Miller NL, Fowke JH, Hameed O, Hayward SW, et al. Surgical intervention for symptomatic benign prostatic hyperplasia is correlated with expression of the AP-1 transcription factor network. Prostate. 2014;74:669–79.
Muller RL, Gerber L, Moreira DM, Andriole G Jr, Hamilton RJ, Fleshner N, et al. Obesity is associated with increased prostate growth and attenuated prostate volume reduction by dutasteride. Eur Urol. 2013;63:1115–21.
Parsons JK, Schenk JM, Arnold KB, Messer K, Till C, Thompson IM, et al. Finasteride reduces the risk of incident clinical benign prostatic hyperplasia. Eur Urol. 2012;62:234–41.
Ellem SJ, Risbridger GP. Treating prostate cancer: a rationale for targeting local oestrogens. Nat Rev Cancer. 2007;7:621–7.
King KJ, Nicholson HD, Assinder SJ. Effect of increasing ratio of estrogen: androgen on proliferation of normal human prostate stromal and epithelial cells, and the malignant cell line LNCaP. Prostate. 2006;66:105–14.
Subbaramaiah K, Howe LR, Bhardwaj P, Du B, Gravaghi C, Yantiss RK, et al. Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res. 2011;4:329–46.
Fessler MB, Rudel LL, Brown JM. Toll-like receptor signaling links dietary fatty acids to the metabolic syndrome. Curr Opin Lipido. 2009;20:379–85.
Suganami T, Tanimoto-Koyama K, Nishida J, Itoh M, Yuan X, Mizuarai S, et al. Role of the Toll-like receptor 4/NF-kappaB pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler Thromb Vasc Biol. 2007;27:84–91.
Dias JP, Melvin D, Shardell M, Ferrucci L, Chia CW, Gharib M, et al. Effects of transdermal testosterone gel or an aromatase inhibitor on prostate volume in older men. J Clin Endocrinol Metab. 2016;101:1865–71.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–46.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808.
Aaron-Brooks LM, Sasaki T, Vickman RE, Wei L, Franco OE, Ji Y, et al. Hyperglycemia and T Cell infiltration are associated with stromal and epithelial prostatic hyperplasia in the nonobese diabetic mouse. Prostate. 2019;79:980–93.
Parsons JK, Sarma AV, McVary K, Wei JT. Obesity and benign prostatic hyperplasia: clinical connections, emerging etiological paradigms and future directions. J Urol. 2009;182(6 Suppl):S27–31.
Williams G. Aromatase up-regulation, insulin and raised intracellular oestrogens in men, induce adiposity, metabolic syndrome and prostate disease, via aberrant ER-alpha and GPER signalling. Mol Cell Endocrinol. 2012;351:269–78.
Kaplan SA, Lee JY, Meehan AG, Kusek JW. Time course of incident adverse experiences associated with doxazosin, finasteride, and combination therapy in men with benign prostatic hyperplasia: the medical therapy of prostatic symptoms (MTOPS) trial. J Urol. 2015;195:1825–9.
Roehrborn CG, Spann ME, Myers SL, Serviss CR, Hu L, Jin Y. Estrogen receptor beta agonist LY500307 fails to improve symptoms in men with enlarged prostate secondary to benign prostatic hypertrophy. Prostate Cancer Prostatic Dis. 2015;18:43–8.
Acknowledgements
AFO gratefully acknowledges financial support from NIH/NIDDK (NIH/R01 DK091353). ZW was supported by the Urology Care Foundation/American Urological Association Research Scholar Award. We gratefully thank Dr Li Xin at University of Washington for supplying prostate tissues of mice fed with HFD or RFD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xue, B., Wu, S., Sharkey, C. et al. Obesity-associated inflammation induces androgenic to estrogenic switch in the prostate gland. Prostate Cancer Prostatic Dis 23, 465–474 (2020). https://doi.org/10.1038/s41391-020-0208-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-0208-4
This article is cited by
-
Exploring the Enigma of 5-ARIs Resistance in Benign Prostatic Hyperplasia: Paving the Path for Personalized Medicine
Current Urology Reports (2023)
-
Upregulation of mir-1199-5p is associated with reduced type 2 5-α reductase expression in benign prostatic hyperplasia
BMC Urology (2022)
-
Improvement of quality of life and symptom burden after robot-assisted radical prostatectomy in patients with moderate to severe LUTS
Scientific Reports (2021)