Abstract
Background
Multiparametric magnetic resonance imaging (MP-MRI) and MRI/ultrasound (US) fusion-guided biopsy are becoming more widely used techniques for prostate cancer (PCa) diagnosis and management. However, their widespread adoption and use, where available, are limited by cost and added time. These limitations could be minimized if a biparametric MRI (BP-MRI) focusing on T2-weighted and diffusion-weighted imaging is performed. Herein we report the cancer detection rate of BP-MRI compared with full MP-MRI.
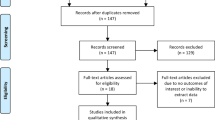
Methods
Biopsy-naive and prior negative biopsy patients with clinical suspicion for PCa underwent MP-MRI with an imaging protocol incorporating narrow field-of-view T2-weighted, diffusion-weighted, and DCE pelvic MRI. Then patients underwent MRI/US fusion-guided biopsy of target lesions between November 2013 and October 2017. The pathology results were compared to the positivity of the DCE sequence compared to the BP-MRI findings alone.
Results
There were 648 targeted lesions biopsied in 344 patients. We defined biparametric screen filter positivity as both T2-weighted and diffusion-weighted imaging positivity for the same lesion. The majority of target lesions (552/648, 85%) were screen filter positive. For those that were screen filter negative, a minority (14/96, 15%) had DCE-positive findings. Of these, 2/3 (67%) cancer-positive cases were seen on T2-weighted imaging. For those 82 that were screen filter negative and DCE negative, the DCE phase would not have added imaging suspicion. Only 3/82 (3.7%) were cancer positive; 2 with low risk, grade group 1 cancer and 1 with intraductal carcinoma, all identified on targeted T2-weighted MRI positivity.
Conclusions
BP-MRI for the evaluation of PCa and for guiding MRI/US fusion-targeted biopsy has the advantages of reducing cost, time, and contrast exposure of MP-MRI by eliminating the DCE phase. These benefits are realized without forfeiting valuable diagnostic information, as shown by similar cancer detection rates of BP-MRI and MP-MRI in this study, particularly for clinically significant cases of PCa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7.
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol. 2015;68:438.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390.
Kuhl CK, Bruhn R, Krämer N, Nebelung S, Heidenreich A, Schrading S. Abbreviated biparametric prostate MR imaging in men with elevated prostate-specific antigen. Radiology. 2017;285:493–505.
Bjurlin MA, Meng X, Nobin JL, Wysock JS, Lepor H, Rosenkrantz AB, et al. Optimization of prostate biopsy: the role of magnetic resonance imaging targeted biopsy in detection, localization and risk assessment. J Urol. 2014;192:648–58.
Rais-Bahrami S, Siddiqui MM, Vourganti S, Turkbey B, Rastinehad AR, Stamatakis L, et al. Diagnostic value of biparametric magnetic resonance imaging (MRI) as an adjunct to prostate-specific antigen (PSA)-based detection of prostate cancer in men without prior biopsies. BJU Int. 2015;115:381–8.
Porter KK, King A, Galgano S, et al. Financial implications of biparametric prostate MRI. In preparation (2018).
Lai WS, Gordetsky JB, Thomas JV, Nix JW, Rais-Bahrami S, et al. Factors predicting prostate cancer upgrading on magnetic resonance imaging-targeted biopsy in an active surveillance population. Cancer. 2017;123:1941–8.
Yarlagadda VK, Lai WS, Gordetsky JB, Porter KK, Nix JW, Thomas JV, et al. MRI/US fusion-guided prostate biopsy allows for equivalent cancer detection with significantly fewer needle cores in biopsy-naive men. Diagn Interv Radiol. 2018 ;24:115–20.
Gaur S, Harmon S, Mehralivand S, Bednarova S, Calio BP, Sugano D, et al. Prospective comparison of PI-RADS version 2 and qualitative in-house categorization system in detection of prostate cancer. J Magn Reson Imaging. 2018;48:1326–35.
Muthigi A, Sidana A, George AK, Kongnyuy M, Maruf M, Valayil S, et al. Current beliefs and practice patterns among urologists regarding prostate magnetic resonance imaging and magnetic resonance-targeted biopsy. Urol Oncol. 2017;35:32.e1–7.
Vourganti S, Starkweather N, Wojtowycz A. MR/US fusion technology: what makes it tick? Curr Urol Rep. 2017;18:20.
Gorin MA, Walsh PC. Magnetic resonance imaging prior to first prostate biopsy-are we there yet? Eur Urol. 2018. https://doi.org/10.1016/j.eururo.2018.05.018
Faria R, Soares MO, Spackman E, Ahmed HU, Brown LC, Kaplan R, et al. Optimising the diagnosis of prostate cancer in the era of multiparametric magnetic resonance imaging: a cost-effectiveness analysis based on the Prostate MR Imaging Study (PROMIS). Eur Urol. 2018;73:23–30.
Wilt TJ, Brawer MK, Jones KM, Barry MJ, Aronson WJ, Fox S, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367:203–13.
Glaser ZA, Gordetsky JB, Porter KK, Varambally S, Rais-Bahrami S. Prostate cancer imaging and biomarkers guiding safe selection of active surveillance. Front Oncol. 2017;7:256.
Loeb S, Byrne N, Makarov DV, Lepor H, Walter D. Use of conservative management for low-risk prostate cancer in the Veterans Affairs Integrated Health Care System from 2005–15. JAMA. 2018. https://doi.org/10.1001/jama.2018.5616
Gordetsky JB, Saylor B, Bae S, Nix JW, Rais-Bahrami S. Prostate cancer management choices in patients undergoing multiparametric magnetic resonance imaging/ultrasound fusion biopsy compared to systematic biopsy. Urol Oncol. 2018;36:241.e7–13.
Rosenkrantz AB, Verma S, Choyke P, Eberhardt SC, Eggener SE, Gaitonde K, et al. Prostate magnetic resonance imaging and magnetic resonance imaging targeted biopsy in patients with a prior negative biopsy: a Consensus Statement by AUA and SAR. J Urol. 2016;196:1613–8.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Fascelli M, Rais-Bahrami S, Sankineni S, Brown AM, George AK, Ho R, et al. Combined biparametric prostate magnetic resonance imaging and prostate-specific antigen in the detection of prostate cancer: a validation study in a biopsy-naïve patient population. Urology. 2016;88:125–34.
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS prostate imaging - reporting and data system: 2015, Version 2. Eur Urol. 2016;69:16–40.
Sheridan AD, Nath SK, Syed JS, Aneja S, Sprenkle PC, Weinreb JC, et al. Risk of clinically significant prostate cancer associated with prostate imaging reporting and data system category 3 (equivocal) lesions identified on multiparametric prostate MRI. AJR Am J Roentgenol. 2017;210:347–57.
American College of Radiology. Manual on contrast media, version 10.3. American College of Radiology; 2017.
Jung JW, Kang HR, Kim MH, Lee W, Min KU, Han MH, et al. Immediate hypersensitivity reaction to gadolinium-based MR contrast media. Radiology. 2012;264:414–22.
Malayeri AA, Brooks KM, Bryant LH, Evers R, Kumar P, Reich DS, et al. National Institutes of Health perspective on reports of gadolinium deposition in the brain. J Am Coll Radiol. 2016;13:237–41.
FDA in brief: FDA requires new class warning and additional research on retention in the body of gadolinium from gadolinium-based contrast agents used in magnetic resonance imaging. 2017. https://www.fda.gov/NewsEvents/Newsroom/FDAInBrief/ucm589604.htm
Acknowledgements
This work was funded in part by Junior Faculty Development Grant (ACS-IRG 001-53) and by Developmental funds from the UAB Comprehensive Cancer Center Support Grant (NCI P30 CA 013148) to Soroush Rais-Bahrami.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JWN and SR-B serve as consultants to Philips/InVivo Corp. The other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sherrer, R.L., Glaser, Z.A., Gordetsky, J.B. et al. Comparison of biparametric MRI to full multiparametric MRI for detection of clinically significant prostate cancer. Prostate Cancer Prostatic Dis 22, 331–336 (2019). https://doi.org/10.1038/s41391-018-0107-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0107-0
This article is cited by
-
A nomogram based on biparametric magnetic resonance imaging for detection of clinically significant prostate cancer in biopsy-naïve patients
Cancer Imaging (2023)
-
The role of preoperative prostatic shape in the recovery of urinary continence after robotic radical prostatectomy: a single cohort analysis
Prostate Cancer and Prostatic Diseases (2023)
-
Parametric maps of spatial two-tissue compartment model for prostate dynamic contrast enhanced MRI - comparison with the standard tofts model in the diagnosis of prostate cancer
Physical and Engineering Sciences in Medicine (2023)
-
Radiomics vs radiologist in prostate cancer. Results from a systematic review
World Journal of Urology (2023)
-
Head-to-head comparison of biparametric versus multiparametric MRI of the prostate before robot-assisted transperineal fusion prostate biopsy
World Journal of Urology (2022)