Abstract
Background
Racial differences in prostate cancer (PCa) outcomes in the United States may be due to differences in tumor biology and race-based differences in access and treatment. We designed a study to estimate the relative contribution of these factors on Black/White disparities in overall survival (OS) in advanced PCa.
Methods
We identified Black and White men aged ≥ 40 years with metastatic or locally advanced PCa (cN+ cM+ and/or T3/4) between 2004 and 2010 using the National Cancer Database. We employed sequential propensity score weighting procedures to generate simulated cohorts of Black and White patients with equal demographics, access to care, treatment, and tumor characteristics. Adjusted survival analyses were used to compare survival in these simulated cohorts. The changes in relative survival after each weighting procedure were used to infer the contribution of each set of variables on the excess risk of mortality in Blacks.
Results
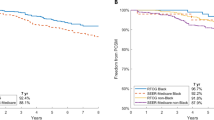
In total, 35,611 men met inclusion criteria, 5927 (16.77%) of whom were Black. Survival was significantly worse for Black men after adjusting for demographics and comorbidities (hazard ratio (HR) 1.27, 95%-confidence interval (95%-CI) 1.2–1.34, p < 0.001). After simulating equal access to care, there was no significant difference in survival between races (HR 1.04, 95%-CI 0.97–1.12, p = 0.276), despite worse tumor characteristics in Blacks. After simulating equal treatment and equivalent tumor characteristics, Black men had a better survival than Whites (HR 0.93, 95%-CI 0.86–1.01, p = 0.071 and HR 0.92, 95%-CI 0.84–1.00, p = 0.043, respectively). Overall, access-related variables explained 84.7% of the excess risk of death in Black men.
Conclusion
Our analysis of men with advanced PCa revealed worse OS among Blacks. However, when access to care, treatment, and cancer characteristics are accounted for, Black race was associated with better OS. These findings suggest that initiatives to improve access to care may represent an effective tool to reduce disparities in PCa outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30.
Hayn MH, Orom H, Shavers VL, Sanda MG, Glasgow M, Mohler JL, et al. Racial/ethnic differences in receipt of pelvic lymph node dissection among men with localized/regional prostate cancer. Cancer. 2011;117:4651–8.
Gaines AR, Turner EL, Moorman PG, Freedland SJ, Keto CJ, McPhail ME, et al. The association between race and prostate cancer risk on initial biopsy in an equal access, multiethnic cohort. Cancer Causes Control. 2014;25:1029–35.
Mukerji B, Baptiste C, Chen L, Tergas AI, Hou JY, Ananth CV, et al. Racial disparities in young women with endometrial cancer. Gynecol Oncol. 2018;148:527–34.
Miller JW, Smith JL, Ryerson AB, Tucker TC, Allemani C. Disparities in breast cancer survival in the United States (2001-2009): findings from the CONCORD-2 study. Cancer. 2017;123(Suppl 24):5100–18.
White A, Joseph D, Rim SH, Johnson CJ, Coleman MP, Allemani C. Colon cancer survival in the United States by race and stage (2001-2009): findings from the CONCORD-2 study. Cancer. 2017;123(Suppl 24):5014–36.
Sundi D, Ross AE, Humphreys EB, Han M, Partin AW, Carter HB, et al. African American men with very low-risk prostate cancer exhibit adverse oncologic outcomes after radical prostatectomy: should active surveillance still be an option for them? J Clin Oncol. 2013;31:2991–7.
Sundi D, Kryvenko ON, Carter HB, Ross AE, Epstein JI, Schaeffer EM. Pathological examination of radical prostatectomy specimens in men with very low risk disease at biopsy reveals distinct zonal distribution of cancer in black American men. J Urol. 2014;191:60–67.
Powell IJ, Dyson G, Land S, Ruterbusch J, Bock CH, Lenk S, et al. Genes associated with prostate cancer are differentially expressed in African American and European American men. Cancer Epidemiol Biomark Prev. 2013;22:891–7.
Taioli E, Sears V, Watson A, Flores-Obando RE, Jackson MD, Ukoli FA, et al. Polymorphisms in CYP17 and CYP3A4 and prostate cancer in men of African descent. Prostate. 2013;73:668–76.
Mahal BA, Chen YW, Muralidhar V, Mahal AR, Choueiri TK, Hoffman KE, et al. Racial disparities in prostate cancer outcome among prostate-specific antigen screening eligible populations in the United States. Ann Oncol. 2017;28:1098–104.
Barocas DA, Grubb R 3rd, Black A, Penson DF, Fowke JH, Andriole G, et al. Association between race and follow-up diagnostic care after a positive prostate cancer screening test in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer. 2013;119:2223–9.
Friedlander DF, Trinh QD, Krasnova A, Lipsitz SR, Sun M, Nguyen PL, et al. Racial disparity in delivering definitive therapy for intermediate/high-risk localized prostate cancer: the impact of facility features and socioeconomic characteristics. Eur Urol. 2017;73:445–51.
Schmid M, Meyer CP, Reznor G, Choueiri TK, Hanske J, Sammon JD, et al. Racial differences in the surgical care of medicare beneficiaries with localized prostate cancer. JAMA Oncol. 2016;2:85–93.
Cullen J, Brassell SA, Chen Y, Porter C, L’Esperance J, Brand T, et al. Racial/ethnic patterns in prostate cancer outcomes in an active surveillance cohort. Prostate Cancer. 2011;2011:234519.
Jemal A, Robbins AS, Lin CC, Flanders WD, DeSantis CE, Ward EM, et al. Factors that contributed to Black-White disparities in survival among nonelderly women with breast cancer between 2004 and 2013. J Clin Oncol. 2018;36:14–24.
Sineshaw HM, Ng K, Flanders WD, Brawley OW, Jemal A. Factors that contribute to differences in survival of Black versus White patients with colorectal cancer. Gastroenterology. 2017;154:906–15.
Cole AP, Friedlander DF, Trinh QD. Secondary data sources for health services research in urologic oncology. Urol Oncol. 2018;36:165–73.
Lerro CC, Robbins AS, Phillips JL, Stewart AK. Comparison of cases captured in the national cancer data base with those in population-based central cancer registries. Ann Surg Oncol. 2013;20:1759–65.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15:683–90.
Klein JB, Nguyen CT, Saffore L, Modlin C 3rd, Modlin CS Jr. Racial disparities in urologic health care. J Natl Med Assoc. 2010;102:108–17.
Gooden KM, Howard DL, Carpenter WR, Carson AP, Taylor YJ, Peacock S, et al. The effect of hospital and surgeon volume on racial differences in recurrence-free survival after radical prostatectomy. Med Care. 2008;46:1170–6.
Cole AP, Trinh QD. Secondary data analysis: techniques for comparing interventions and their limitations. Curr Opin Urol. 2017;27:354–9.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Villarroel MA, Cohen RA. Health insurance continuity and health care access and utilization, 2014. NCHS Data Brief. 2016;249:1–8.
Toscos T, Carpenter M, Flanagan M, Kunjan K, Doebbeling BN. Identifying successful practices to overcome access to care challenges in community health centers: a “positive deviance” approach. Health Serv Res Manag Epidemiol. 2018;5:2333392817743406.
Mahal BA, Ziehr DR, Aizer AA, Hyatt AS, Sammon JD, Schmid M, et al. Getting back to equal: the influence of insurance status on racial disparities in the treatment of African American men with high-risk prostate cancer. Urol Oncol. 2014;32:1285–91.
Pietro GD, Chornokur G, Kumar NB, Davis C, Park JY. Racial differences in the diagnosis and treatment of prostate cancer. Int Neurourol J. 2016;20(Suppl 2):S112–119.
Moses KA, Orom H, Brasel A, Gaddy J, Underwood W 3rd. Racial/ethnic differences in the relative risk of receipt of specific treatment among men with prostate cancer. Urol Oncol. 2016;34:415 e417–15.
George DJ, Heath EI, Sartor AO, Sonpavde G, Berry WR, Healy P, et al. Abi race: a prospective, multicenter study of black (B) and white (W) patients (pts) with metastatic castrate resistant prostate cancer (mCRPC) treated with abiraterone acetate and prednisone (AAP). J Clin Oncol. 2018;36 (Suppl; abstr LBA5009) https://doi.org/10.1200/JCO.2018.36.18_suppl.LBA5009.
Halabi S, Dutta S, Tangen CM, Rosenthal M, Petrylak DP, Thompson IM, et al. Overall survival between African-American (AA) and Caucasian (C) men with metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2018;36 (Abstract LBA5005) https://doi.org/10.1200/JCO.2018.36.18_suppl.LBA5005.
Szklo M, Nieto, FJ. Epidemiology: beyond the basics. Sudbury, MA: Jones and Bartlett; 2004.
Ziehr DR, Mahal BA, Aizer AA, Hyatt AS, Beard CJ, DA AV, et al. Income inequality and treatment of African American men with high-risk prostate cancer. Urol Oncol. 2015;33:18 e17–8.
Watson M, Grande D, Radhakrishnan A, Mitra N, Ward KR, Pollack CE. Racial differences in prostate cancer treatment: the role of socioeconomic status. Ethn Dis. 2017;27:201–8.
Acknowledgements
Q-DT is supported by the Brigham Research Institute Fund to Sustain Research Excellence, the Bruce A. Beal and Robert L. Beal Surgical Fellowship, the Genentech Bio-Oncology Career Development Award from the Conquer Cancer Foundation of the American Society of Clinical Oncology, a Health Services Research pilot test grant from the Defense Health Agency, the Clay Hamlin Young Investigator Award from the Prostate Cancer Foundation, and an unrestricted educational grant from the Vattikuti Urology Institute. The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. Quoc-Dien Trinh and Marieke J. Krimphove had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Q-DT reports honoraria from Bayer and Astellas. ASK reports consulting fees from Sanofi, Dendreon, Tokai, and Profound. PLN consulted for Ferring, Bayer, Astellas, Janssen, Blue Earth, Dendreon and received research funding from Janssen and Astellas. JCH is on the speakers’ bureau for Genomic Health. These financial relationships are outside this submitted work.
Rights and permissions
About this article
Cite this article
Krimphove, M.J., Cole, A.P., Fletcher, S.A. et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis 22, 125–136 (2019). https://doi.org/10.1038/s41391-018-0083-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0083-4
This article is cited by
-
Emerging racial disparities among Medicare beneficiaries and Veterans with metastatic castration-sensitive prostate cancer
Prostate Cancer and Prostatic Diseases (2024)
-
The association of patient and disease characteristics with the overtreatment of low-risk prostate cancer from 2010 to 2016
Prostate Cancer and Prostatic Diseases (2024)
-
Prostate cancer metastasis and health disparities: a systematic review
Prostate Cancer and Prostatic Diseases (2023)
-
Five-year survival of patients with late-stage prostate cancer: comparison of the Military Health System and the U.S. general population
British Journal of Cancer (2023)
-
Trends in prostate cancer mortality in the United States of America, by state and race, from 1999 to 2019: estimates from the centers for disease control WONDER database
Prostate Cancer and Prostatic Diseases (2023)