Abstract
Background
There are few prospective studies comparing race-specific associations between diet, nutrients, and health-related parameters, and prostate cancer risk.
Methods
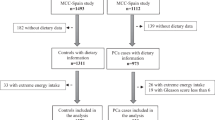
Race-specific prostate cancer risk associations were examined among men in the National Institutes of Health (NIH)-AARP Diet and Health Study. We identified 1417 cases among black men (209 advanced), and 28,845 among white men (3898 advanced). Cox proportional hazards regression models estimated hazard ratios (HRs) and 95% confidence intervals (CIs). We also evaluated the cumulative change in the HR for black race following adjustment for each factor.
Results
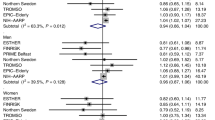
Race-specific prostate cancer associations were similar in black and white men across disease subtypes only for history of diabetes (overall : HR = 0.77, 95% CI: 0.65–0.90 and HR = 0.72, 95% CI: 0.69–0.76, respectively; Pinteraction = 0.66). By contrast, there was a positive risk association with height for white men and inverse for black men (Pinteraction: non-advanced = 0.01; advanced = 0.04). This difference remained among men with at least 2 years of follow-up for non-advanced (Pinteraction = 0.01), but not advanced disease (Pinteraction = 0.24); or after adjustment for prostate cancer screening (non-advanced Pinteraction = 0.53, advanced Pinteraction = 0.31). The only other evidence of interaction with race was observed for dietary vitamin D intake and non-advanced disease, but only after adjustment for screening (Pinteraction = 0.02). Cumulative adjustment for each factor increased the HR for black race by 32.9% for overall cancer and 12.4% for advanced disease.
Conclusions
Our data suggest few of the dietary, nutrient, and health-related factors associated with prostate cancer risk in predominantly non-Hispanic white men were associated with risk in black men, and adjustment for these factors widen the black–white difference in risk. Larger studies of black men, particularly with prospective data, are needed to help identify risk factors relevant to this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
American Cancer Society. Cancer Facts & Figures for African Americans 2016-2018. Atlanta: American Cancer Society, 2016.
Chornokur G, Dalton K, Borysova ME, Kumar NB. Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. Prostate. 2011;71:985–97.
Freedland SJ, Isaacs WB. Explaining racial differences in prostate cancer in the United States: sociology or biology? Prostate. 2005;62:243–52.
Jones BA, Liu WL, Araujo AB, Kasl SV, Silvera SN, Soler-Vila H, et al. Explaining the race difference in prostate cancer stage at diagnosis. Cancer Epidemiol Biomark Prev. 2008;17:2825–34.
Martin DN, Starks AM, Ambs S. Biological determinants of health disparities in prostate cancer. Curr Opin Oncol. 2013;25:235–41.
Martin DN, Lam TK, Brignole K, Ashing KT, Blot WJ, Burhansstipanov L, et al. Recommendations for cancer epidemiologic research in understudied populations and implications for future needs. Cancer Epidemiol Biomark Prev. 2016;25:573–80.
Kolonel LN, Hankin JH, Whittemore AS, Wu AH, Gallagher RP, Wilkens LR, et al. Vegetables, fruits, legumes and prostate cancer: a multiethnic case-control study. Cancer Epidemiol Biomark Prev. 2000;9:795–804.
Vogt TM, Mayne ST, Graubard BI, Swanson CA, Sowell AL, Schoenberg JB, et al. Serum lycopene, other serum carotenoids, and risk of prostate cancer in US Blacks and Whites. Am J Epidemiol. 2002;155:1023–32.
Whittemore AS, Kolonel LN, Wu AH, John EM, Gallagher RP, Howe GR, et al. Prostate cancer in relation to diet, physical activity, and body size in blacks, whites, and Asians in the United States and Canada. J Natl Cancer Inst. 1995;87:652–61.
Vogt TM, Ziegler RG, Graubard BI, Swanson CA, Greenberg RS, Schoenberg JB, et al. Serum selenium and risk of prostate cancer in U.S. blacks and whites. Int J Cancer. 2003;103:664–70.
Jackson M, Tulloch-Reid M, Walker S, McFarlane-Anderson N, Bennett F, Francis D, et al. Dietary patterns as predictors of prostate cancer in Jamaican men. Nutr Cancer. 2013;65:367–74.
Hayes RB, Ziegler RG, Gridley G, Swanson C, Greenberg RS, Swanson GM, et al. Dietary factors and risks for prostate cancer among blacks and whites in the United States. Cancer Epidemiol Biomark Prev. 1999;8:25–34.
Sanderson M, Coker AL, Logan P, Zheng W, Fadden MK. Lifestyle and prostate cancer among older African-American and Caucasian men in South Carolina. Cancer Causes Control. 2004;15:647–55.
Rowland GW, Schwartz GG, John EM, Ingles SA. Calcium intake and prostate cancer among African Americans: effect modification by vitamin D receptor calcium absorption genotype. J Bone Miner Res. 2012;27:187–94.
Ben-Shlomo Y, Evans S, Ibrahim F, Patel B, Anson K, Chinegwundoh F, et al. The risk of prostate cancer amongst black men in the United Kingdom: the PROCESS cohort study. Eur Urol. 2008;53:99–105.
Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154:1119–25.
Michaud D, Midthune D, Hermansen S, Leitzmann M, Harlan L, Kipnis V, et al. Comparison of cancer registry case ascertainment with SEER estimates and self-reporting in a subset of the NIH-AARP Diet and Health Study. J Regist Manag. 2005;32:70–75.
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8:551–61.
Park SY, Haiman CA, Cheng I, Park SL, Wilkens LR, Kolonel LN, et al. Racial/ethnic differences in lifestyle-related factors and prostate cancer risk: the Multiethnic Cohort Study. Cancer Causes Control. 2015;26:1507–15.
Platz EA, Rimm EB, Willett WC, Kantoff PW, Giovannucci E. Racial variation in prostate cancer incidence and in hormonal system markers among male health professionals. J Natl Cancer Inst. 2000;92:2009–17.
Atchison EA, Gridley G, Carreon JD, Leitzmann MF, McGlynn KA. Risk of cancer in a large cohort of U.S. veterans with diabetes. Int J Cancer. 2011;128:635–43.
Bansal D, Bhansali A, Kapil G, Undela K, Tiwari P. Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2013;16:151–8. S151
Rastmanesh R, Hejazi J, Marotta F, Hara N. Type 2 diabetes: a protective factor for prostate cancer? An overview of proposed mechanisms. Clin Genitourin Cancer. 2014;12:143–8.
Travis RC, Appleby PN, Martin RM, Holly JMP, Albanes D, Black A, et al. A meta-analysis of individual participant data reveals an association between circulating levels of IGF-I and prostate cancer risk. Cancer Res. 2016;76:2288–300.
World Cancer Research Fund International/American Institute for Cancer Research Continuous Report Update Project Report. Diet, Nutrition, Physical Acitivity, and Prostate Cancer, 2014.
Mordukhovich I, Reiter PL, Backes DM, Family L, McCullough LE, O’Brien KM, et al. A review of African American-white differences in risk factors for cancer: prostate cancer. Cancer Causes Control. 2011;22:341–57.
Kabat GC, Kim MY, Hollenbeck AR, Rohan TE. Attained height, sex, and risk of cancer at different anatomic sites in the NIH-AARP Diet and Health Study. Cancer Causes Control. 2014;25:1697–706.
Rodriguez C, Patel AV, Calle EE, Jacobs EJ, Chao A, Thun MJ. Body mass index, height, and prostate cancer mortality in two large cohorts of adult men in the United States. Cancer Epidemiol Biomark Prev. 2001;10:345–53.
Habel LA, Van Den Eeden SK, Friedman GD. Body size, age at shaving initiation, and prostate cancer in a large, multiracial cohort. Prostate. 2000;43:136–43.
Zuccolo L, Harris R, Gunnell D, Oliver S, Lane JA, Davis M, et al. Height and prostate cancer risk: a large nested case-control study (ProtecT) and meta-analysis. Cancer Epidemiol Biomark Prev. 2008;17:2325–36.
Ahn J, Moore SC, Albanes D, Huang WY, Leitzmann MF, Hayes RB, et al. Height and risk of prostate cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Br J Cancer. 2009;101:522–5.
Freedland SJ, Aronson WJ, Trock B, Cohen P, Kane CJ, Amling CL, et al. Racial differences in prognostic value of adult height for biochemical progression following radical prostatectomy. Clin Cancer Res. 2005;11:7735–42.
Platz EA, Pollak MN, Rimm EB, Majeed N, Tao Y, Willett WC, et al. Racial variation in insulin-like growth factor-1 and binding protein-3 concentrations in middle-aged men. Cancer Epidemiol Biomark Prev. 1999;8:1107–10.
McGreevy K, Hoel B, Lipsitz S, Bissada N, Hoel D. Racial and anthropometric differences in plasma levels of insulin-like growth factor I and insulin-like growth factor binding protein-3. Urology. 2005;66:587–92.
Gilbert R, Martin RM, Beynon R, Harris R, Savovic J, Zuccolo L, et al. Associations of circulating and dietary vitamin D with prostate cancer risk: a systematic review and dose-response meta-analysis. Cancer Causes Control. 2011;22:319–40.
Xu Y, Shao X, Yao Y, Xu L, Chang L, Jiang Z, et al. Positive association between circulating 25-hydroxyvitamin D levels and prostate cancer risk: new findings from an updated meta-analysis. J Cancer Res Clin Oncol. 2014;140:1465–77.
Swami S, Krishnan AV, Feldman D. Vitamin D metabolism and action in the prostate: implications for health and disease. Mol Cell Endocrinol. 2011;347:61–69.
Layne TM, Weinstein SJ, Graubard BI, Ma X, Mayne ST, Albanes D. Serum 25-hydroxyvitamin D, vitamin D binding protein, and prostate cancer risk in black men. Cancer. 2017;123:2698–704.
Park SY, Murphy SP, Wilkens LR, Stram DO, Henderson BE, Kolonel LN. Calcium, vitamin D, and dairy product intake and prostate cancer risk: the Multiethnic Cohort Study. Am J Epidemiol. 2007;166:1259–69.
Tseng M, Breslow RA, Graubard BI, Ziegler RG. Dairy, calcium, and vitamin D intakes and prostate cancer risk in the National Health and Nutrition Examination Epidemiologic Follow-up Study cohort. Am J Clin Nutr. 2005;81:1147–54.
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81.
O’Neil CE, Nicklas TA, Keast DR, Fulgoni VL. Ethnic disparities among food sources of energy and nutrients of public health concern and nutrients to limit in adults in the United States: NHANES 2003-2006. Food Nutr Res. 2014;58:15784.
Batai K, Murphy AB, Nonn L, Kittles RA. Vitamin D and immune response: implications for prostate cancer in African Americans. Front Immunol. 2016;7:53.
Hardiman G, Savage SJ, Hazard ES, Wilson RC, Courtney SM, Smith MT, et al. Systems analysis of the prostate transcriptome in African-American men compared with European-American men. Pharmacogenomics. 2016;17:1129–43.
Acknowledgements
This research was supported [in part] by the Intramural Research Program of the NIH, National Cancer Institute. Cancer incidence data from the Atlanta metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia. Cancer incidence data from California were collected by the California Cancer Registry, California Department of Public Health’s Cancer Surveillance and Research Branch, Sacramento, California. Cancer incidence data from the Detroit metropolitan area were collected by the Michigan Cancer Surveillance Program, Community Health Administration, Lansing, Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System (Miami, Florida) under contract with the Florida Department of Health, Tallahassee, Florida. The views expressed herein are solely those of the authors and do not necessarily reflect those of the FCDC or FDOH. Cancer incidence data from Louisiana were collected by the Louisiana Tumor Registry, Louisiana State University Health Sciences Center School of Public Health, New Orleans, Louisiana. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, The Rutgers Cancer Institute of New Jersey, New Brunswick, New Jersey. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry, Raleigh, North Carolina. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions. Cancer incidence data from Arizona were collected by the Arizona Cancer Registry, Division of Public Health Services, Arizona Department of Health Services, Phoenix, Arizona. Cancer incidence data from Texas were collected by the Texas Cancer Registry, Cancer Epidemiology and Surveillance Branch, Texas Department of State Health Services, Austin, Texas. Cancer incidence data from Nevada were collected by the Nevada Central Cancer Registry, Division of Public and Behavioral Health, State of Nevada Department of Health and Human Services, Carson City, Nevada. We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. We also thank Sigurd Hermansen and Kerry Grace Morrissey from Westat for study outcomes ascertainment and management and Leslie Carroll at Information Management Services for data support and analysis.
Author contributions
DA, STM, XM, and BIG designed the research; TML conducted and analyzed the data; TML, DA, STM, XM, and BIG wrote the paper; TML and DA have primary responsibility for the final content. All authors read and approved the final manuscript.
Funding
This work was supported by the Yale-NCI pre-doctoral training grant T32 CA105666 to STM and XM, and by the Intramural Research Program of the National Cancer Institute at the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Layne, T.M., Graubard, B.I., Ma, X. et al. Prostate cancer risk factors in black and white men in the NIH-AARP Diet and Health Study. Prostate Cancer Prostatic Dis 22, 91–100 (2019). https://doi.org/10.1038/s41391-018-0070-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0070-9
This article is cited by
-
Prostate cancer presentation and management in the Middle East
BMC Urology (2024)
-
A 28-year prospective analysis of serum vitamin E, vitamin E-related genetic variation and risk of prostate cancer
Prostate Cancer and Prostatic Diseases (2022)
-
Population-level Patterns of Prostate Cancer Occurrence: Disparities in Virginia
Current Molecular Biology Reports (2022)
-
Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies
European Journal of Epidemiology (2021)
-
Racial and ethnic differences in risk of second primary cancers among prostate cancer survivors
Cancer Causes & Control (2020)