Abstract
Background
The cornerstone of prostate cancer diagnosis remains the transrectal ultrasound-guided biopsy (TRUS-BX), which most frequently occurs in the office setting under local anesthesia. However, there are now other techniques of prostate biopsy aimed at improving outcomes such as patient comfort, significant cancer detection, and infectious complications. The purpose of the present study is to compare the cost and efficacy outcomes of five different approaches.
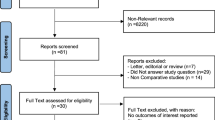
Methods
We compared the comprehensive costs of a random sample size of 20−30 cases from each of the following: (1) local anesthesia TRUS-BX (reference), (2) sedation TRUS-BX, (3) general anesthesia transperineal template biopsy (TP), (4) sedation MRI-TRUS fusion biopsy (FB), and (5) sedation in-bore MRI biopsy (IB-MRI). Cost categories included pre-procedure, anesthesia pharmacy and recovery, and the technical/professional costs from urology, radiology, and pathology services. For procedure outcomes, we compared the larger cohorts of TRUS-BX, TP, and FB in terms of indication, cancer yield, and downstream decision impact.
Results
Compared with standard TRUS-BX, the total costs of sedation TRUS-BX, TP, FB, and IB-MRI increased significantly ×1.9 (90%), ×2.5 (153%), ×2.5 (150%), and ×2.2 (125%), respectively (p < 0.001). Although there was no statistical difference between the total costs of TP, FB, and IB-MRI, these costs were significantly higher than those of TRUS-BX under either local anesthesia or sedation (p < 0.05). The cost of TRUS-BX under sedation was significantly higher than that of TRUS-BX under local anesthesia (p < 0.001). Compared to TRUS-BX, more significant cancers were detected in FB (16% vs. 36%) and TP (16% vs. 34%) groups (p < 0.001).
Conclusions
Compared with standard TRUS-BX, the additions of imaging, sedation anesthesia, and transperineal template increase costs significantly, and can be considered along with known improvements in accuracy and side effects. Ongoing efforts to combine imaging and transperineal biopsy, especially in an outpatient/local anesthesia setting may lead to a higher cost/benefit.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Aubry W, Lieberthal R, Willis A, Bagley G, Willis SM, Layton A. Budget impact model: epigenetic assay can help avoid unnecessary repeated prostate biopsies and reduce healthcare spending. Am Health Drug Benefits. 2013;6:15–24.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65:124–37.
Bjurlin MA, Wysock JS, Taneja SS. Optimization of prostate biopsy: review of technique and complications. Urol Clin North Am. 2014;41:299–313.
Wang J, Wang L, Du Y, He D, Chen X, Li L, et al. Addition of intrarectal local analgesia to periprostatic nerve block improves pain control for transrectal ultrasonography-guided prostate biopsy: a systematic review and meta-analysis. Int J Urol. 2015;22:62–8.
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313:390–7.
Roberts MJ, Bennett HY, Harris PN, Holmes M, Grummet J, Naber K, et al. Prostate biopsy-related infection: a systematic review of risk factors, prevention strategies, and management approaches. Urology. 2017;104:11–21.
Hamoen EHJ, de Rooij M, Witjes JA, Barentsz JO, Rovers MM. Use of the Prostate Imaging Reporting and Data System (PI-RADS) for prostate cancer detection with multiparametric magnetic resonance imaging: a diagnostic meta-analysis. Eur Urol. 2015;67:1112–21.
Yang DD, Mahal BA, Muralidhar V, Vastola ME, Boldbaatar N, Labe SA, et al. Pathologic outcomes of Gleason 6 favorable intermediate-risk prostate cancer treated with radical prostatectomy: implications for active surveillance. Clin Genitourin Cancer. 2018;16:226–34.
Autorino R, De Sio M, Di Lorenzo G, Damiano R, Perdonà S, Cindolo L, et al. How to decrease pain during transrectal ultrasound guided prostate biopsy: a look at the literature. J Urol. 2005;174:2091–7.
Kang SG, Tae BS, Min SH, Ko YH, Kang SH, Lee JG, et al. Efficacy and cost analysis of transrectal ultrasound-guided prostate biopsy under monitored anesthesia. Asian J Androl. 2011;13:724–7.
Turgut AT, Ergun E, Koşar U, Koşar P, Ozcan A. Sedation as an alternative method to lessen patient discomfort due to transrectal ultrasonography-guided prostate biopsy. Eur J Radiol. 2006;57:148–53.
Peters JL, Thompson AC, McNicholas TA, Hines JE, Hanbury DC, Boustead GB. Increased patient satisfaction from transrectal ultrasonography and biopsy under sedation. BJU Int. 2001;87:827–30.
Gershman B, Zietman AL, Feldman AS, McDougal WS. Transperineal template-guided prostate biopsy for patients with persistently elevated PSA and multiple prior negative biopsies. Urol Oncol. 2013;31:1093–7.
Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013;63:125–40.
Natarajan S, Marks LS, Margolis DJ, Huang J, Macairan ML, Lieu P, et al. Clinical application of a 3D ultrasound-guided prostate biopsy system. Urol Oncol. 2011;29:334–42.
Overduin CG, Fütterer JJ, Barentsz JO. MRI-guided biopsy for prostate cancer detection: a systematic review of current clinical results. Curr Urol Rep. 2013;14:209–13.
Ekwueme DU, Stroud LA, Chen Y. Cost analysis of screening for, diagnosing, and staging prostate cancer based on a systematic review of published studies. Prev Chronic Dis. 2007;4:A100.
de Rooij M, Crienen S, Witjes JA, Barentsz JO, Rovers MM, Grutters JP. Cost-effectiveness of magnetic resonance (MR) imaging and MR-guided targeted biopsy versus systematic transrectal ultrasound-guided biopsy in diagnosing prostate cancer: a modelling study from a health care perspective. Eur Urol. 2014;66:430–6.
Lotan Y, Haddad AQ, Costa DN, Pedrosa I, Rofsky NM, Roehrborn CG. Decision analysis model comparing cost of multiparametric magnetic resonance imaging vs. repeat biopsy for detection of prostate cancer in men with prior negative findings on biopsy. Urol Oncol. 2015;33:266.e9–16.
Cerantola Y, Dragomir A, Tanguay S, Bladou F, Aprikian A, Kassouf W. Cost-effectiveness of multiparametric magnetic resonance imaging and targeted biopsy in diagnosing prostate cancer. Urol Oncol. 2016;34:119.e1–9.
Venderink W, Govers TM, de Rooij M, Fütterer JJ, Sedelaar JP. Cost-effectiveness comparison of imaging-guided prostate biopsy techniques: systematic transrectal ultrasound, direct in-bore MRI, and image fusion. AJR Am J Roentgenol. 2017;22:1–6.
Davis JW, Ward JF, Pettaway CA, Wang X, Kuban D, Frank SJ, et al. Disease reclassification risk with stringent criteria and frequent monitoring in men with favourable-risk prostate cancer undergoing active surveillance. BJU Int. 2016;118:68–76.
Acknowledgements
The University of Texas MD Anderson Cancer Center is supported in part by the National Institutes of Health through Cancer Center Support Grant P30CA016672.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Davis: education grant from Intuitive Surgical and research support from Janssen, Genome DX. The remaining authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Altok, M., Kim, B., Patel, B.B. et al. Cost and efficacy comparison of five prostate biopsy modalities: a platform for integrating cost into novel-platform comparative research. Prostate Cancer Prostatic Dis 21, 524–532 (2018). https://doi.org/10.1038/s41391-018-0056-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-018-0056-7
This article is cited by
-
Transrectal prostate biopsy: easy, effective and safe
Prostate Cancer and Prostatic Diseases (2024)
-
A cost-effective transperineal prostate biopsy method utilizes the original transrectal setting
International Urology and Nephrology (2023)
-
Should Transperineal Prostate Biopsy Be the Standard of Care?
Current Urology Reports (2023)
-
Transrectal ultrasound-guided prostate needle biopsy remains a safe method in confirming a prostate cancer diagnosis: a multicentre Australian analysis of infection rates
World Journal of Urology (2022)
-
Transrectal versus transperineal prostate biopsy under intravenous anaesthesia: a clinical, microbiological and cost analysis of 2048 cases over 11 years at a tertiary institution
Prostate Cancer and Prostatic Diseases (2021)