Abstract
Background
The aim was to assess health care providers’ (HCPs) visual attention (VA) by using eye-tracking glasses during a simulated neonatal intubation.
Methods
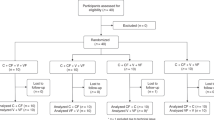
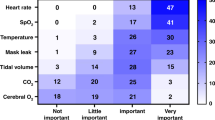
HCPs from three pediatric and neonatal departments (Feldkirch and Vienna, Austria, and Edmonton, Canada) completed a simulated neonatal intubation scenario while wearing eye-tracking glasses (Tobii Pro Glasses 2®, Tobii, Stockholm, Sweden) to record their VA. Main outcomes included duration of intubation, success rate, and VA. We further compared orotracheal and nasotracheal intubations.
Results
30 participants were included. 50% completed the intubation within 30 s (M = 35.40, SD = 16.01). Mostly nasotracheal intubations exceeded the limit. Experience was an important factor in reducing intubation time. VA differed between more and less experienced HCPs as well as between orotracheal and nasotracheal intubations. Participants also focused on different areas of interest (AOIs) depending on the intubator’s experience. More experience was associated with a higher situational awareness (SA) and fewer distractions, which, however, did not transfer to significantly better intubation performance.
Conclusion
Half of the intubations exceeded the recommended time limit. Differences in intubation duration depending on type of intubation were revealed. VA differed between HCPs with different levels of experience and depended on duration and type of intubation.
Impact
-
Simulated neonatal intubation duration differs between orotracheal and nasotracheal intubation.
-
Visual attention during simulated neonatal intubation shows differences depending on intubation duration, intubator experience, type of intubation, and level of distraction.
-
Intubator experience is a vital parameter for reducing intubation duration and improving intubator focus on task-relevant stimuli.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset generated and analyzed during this study is available from the corresponding author on reasonable request.
References
Sawyer, T. et al. Improving neonatal intubation safety: a journey of a thousand miles. J. Neonatal Perinat. Med. 10, 125–131 (2017).
Weiner, G. M., Zaichkin, J., Kattwinkel, J. Textbook of Neonatal Resuscitation 7th edn, (Elk Grove Village, IL: American Academy of Pediatrics, 2016).
Gelbart, B., Hiscock, R. & Barfield, C. Assessment of neonatal resuscitation performance using video recording in a perinatal centre. J. Paediatr. Child Health 46, 378–383 (2010).
Root, L. et al. Improving guideline compliance and documentation through auditing neonatal resuscitation. Front Pediatr. 7, 1–7 (2019).
Simma, B. et al. Delivery room management of infants with very low birth weight in 3 european countries—the video apgar study. J. Pediatr. 222, 106–111 (2020).
Foglia, E. E. et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics 143, 1–10 (2019).
Robinson, M. È. et al. Trainees success rates with intubation to suction meconium at birth. Arch. Dis. Child Fetal Neonatal Ed. 103, F413–F416 (2018).
Leone, T. A., Rich, W. & Finer, N. N. Neonatal intubation: success of pediatric trainees. J. Pediatr. 146, 638–641 (2005).
Belkhatir, K., Scrivens, A., O’Shea, J. E. & Roehr, C. C. Experience and training in endotracheal intubation and laryngeal mask airway use in neonates: results of a national survey. Arch. Dis. Child Fetal Neonatal Ed. 106, 223–224 (2021).
Spence, K., Barr, P. Cochrane Neonatal Group. Nasal versus oral intubation for mechanical ventilation of newborn infants. Cochrane Database Syst Rev. (1999).
Lenclen, R., Narcy, P., Castela, F. & Huard, F. Evaluation of an educational intervention on the standard of neonatal resuscitation: orotracheal versus nasotracheal intubation. Arch. Pediatr. 16, 337–342 (2009).
Wagner, M. et al. Eye-tracking during simulation-based neonatal airway management. Pediatr. Res. 87, 518–522 (2019).
Law, B. H. Y. et al. Analysis of neonatal resuscitation using eye tracking: a pilot study. Arch. Dis. Child Fetal Neonatal Ed. 103, F82–F84 (2018).
Wagner, M. et al. Video-based reflection on neonatal interventions during COVID-19 using eye-tracking glasses: an observational study. Arch. Dis. Child Fetal Neonatal Ed. 107, 156–160 (2022).
Wagner, M. et al. Visual attention during pediatric resuscitation with feedback devices: a randomized simulation study. Pediatr. Res. 91, 1762–1768 (2022).
Endsley, M. R. Measurement of situation awareness in dynamic systems. Hum. Factors J. Hum. Factors Erg. Soc. 37, 65–84 (1995).
Endsley, M. R. Design and evaluation for situation awareness enhancement. Proc. Hum. Factors Soc. 32nd Annu. Meet. 101–197 (1988).
Endsley, M. R. & Hoffman, R. R. The sacagawea principle. IEEE Intell. Syst. 17, 80–85 (2022).
Hamid, H. S., Waternson P. E. Using goal directed task analysis to identify situation awareness requirements of advanced paramedics. In: Advances in Human Factors and Ergonomics in Healthcare (ed. Duffy ViG). First Edition. CRC Press (2011).
Law, B. H. Y. & Schmölzer, G. M. Analysis of visual attention and team communications during neonatal endotracheal intubations using eye-tracking: an observational study. Resuscitation 153, 176–182 (2020).
O’Donnell, C. P. F., Kamlin, C. O. F., Davis, P. G. & Morley, C. J. Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics 117, e16–e21 (2006).
Xue, F. S. et al. Hemodynamic responses to tracheal intubation with the GlideScope® videolaryngoscope: a comparison of oral and nasal routes. Acta Anaesthesiol. Taiwan. 46, 8–15 (2008).
Tien, T. et al. Differences in gaze behaviour of expert and junior surgeons performing open inguinal hernia repair. Surg. Endosc. 29, 405–413 (2015).
McNaughten, B. et al. Clinicians’ gaze behaviour in simulated paediatric emergencies. Arch. Dis. Child 103, 1146–1149 (2018).
Kok, E. M. et al. Systematic viewing in radiology: seeing more, missing less? Adv. Heal Sci. Educ. 21, 189–205 (2016).
Hogan, M. P., Pace, D. E., Hapgood, J. & Boone, D. C. Use of human patient simulation and the situation awareness global assessment technique in practical trauma skills assessment. J. Trauma 61, 1047–1052 (2006).
Acknowledgements
We acknowledge and thank all participants from the three centers for their contributions to this study.
Funding
All authors disclose any type of financial interest related to the manuscript. This study was supported financially by the State of Vorarlberg, Austria (IIb-11.04/35-1/2018). This study was supported by a research grant (Forschungsförderungspreis) from Netzwerk Kindersimulation e.V.
Author information
Authors and Affiliations
Contributions
Conception and design: B.S., M.W., G.S., and L.K. Data collection: G.A., H.A., M.W., G.S., and L.K. Analysis and interpretation of data: P.G. and L.K. The manuscript was drafted and reviewed by all authors and finally approved by all of them.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by each local ethics committee or data protection committee (Ethics Committee of the State of Vorarlberg, Protocol Number: EK-2-7/2018; Health Research Ethics Board – Health Panel in Edmonton, Study ID: Pro00096926; no ethical vote was necessary for this simulation-based study in Vienna).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kessler, L., Gröpel, P., Aichner, H. et al. Eye-tracking during simulated endotracheal newborn intubation: a prospective, observational multi-center study. Pediatr Res 94, 443–449 (2023). https://doi.org/10.1038/s41390-023-02561-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02561-x
This article is cited by
-
Eye-tracking during newborn intubations
Pediatric Research (2023)