Abstract
Background
Sustained systemic inflammatory response (SIR) was associated with poor postnatal growth in very preterm infants (VPI). We hypothesize that VPI with sustained SIR will exhibit linear growth retardation related to lower bone mass accrual mediated by GH/IGF-1 axis inhibition at term corrected age (CA).
Methods
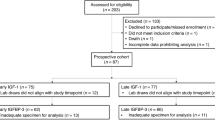
C-reactive protein (CRP), procalcitonin (PCT), growth hormone (GH), insulin-like growth factor 1 (IGF-1), calcium, phosphorus, alkaline phosphatase, anthropometric, nutritional, neonatal and maternal data were collected prospectively in 23 infants <32 weeks gestational age. Body composition using dual-energy X-ray absorptiometry was performed at term CA. Analysis was undertaken with multiple linear regression models.
Results
At term CA 11 infants with sustained SIR compared with 12 infants without sustained SIR present significantly lower IGF-1, length z-score (LZS), bone mineral content (BMC) and lean mass (LM), and higher GH and fat mass (FM). LZS was associated significantly with PCT, BMC with IGF-1, FM and LM with CRP, GH with bronchopulmonary dysplasia and CRP, and IGF-1 with invasive mechanical ventilation, CRP and PCT.
Conclusions
In addition to the known effect on linear growth failure, sustained SIR induces lower bone mass accrual related to higher GH and lower IGF-1 levels in VPI.
Impact
-
Very preterm infants (VPI) with sustained systemic inflammatory response (SIR) compared with VPI without SIR present stunting, lower bone mass, higher GH and lower IGF-1 levels at term corrected age.
-
SIR may help to explain the influence of non-nutritional factors on growth and body composition in VPI.
-
SIR induces postnatal stunting related to lower bone mass accrual via GH/IGF-1 axis inhibition in VPI.
-
VPI with SIR need special attention to minimize inflammatory stress, which could result in improved postnatal growth.
-
Research on inflammatory-endocrine interactions involved in the pathophysiology of postnatal stunting is needed as a basis for new interventional approaches.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during the present study are available to others upon reasonable request via email to the corresponding author.
References
Johnson, L., Llewellyn, C. H., van Jaarsveld, C. H. M., Cole, T. J. & Wardle, J. Genetic and environmental influences on infant growth: prospective analysis of the gemini twin birth cohort. PLoS One 6, e19918 (2011).
Young, A., Beattie, R. M. & Johnson, M. J. Optimising growth in very preterm infants: reviewing the evidence. Arch. Dis. Child. Fetal Neonatal Ed. 108, 2–9. https://doi.org/10.1136/archdischild-2021-322892 (2023).
Möllers, L. S. et al. Metabolic-endocrine disruption due to preterm birth impacts growth, body composition, and neonatal outcome. Pediatr. Res. 91, 1350–1360 (2022).
Maitre, L. et al. Human Early Life Exposome (HELIX) study: a European population-based exposome cohort. BMJ Open 8, e021311 (2018).
Cuestas, E. et al. Socioeconomic inequalities in low birth weight risk before and during the COVID-19 pandemic in Argentina: a cross-sectional study. Lancet Reg. Health Am. 2, 100049 (2021).
Manzar, S. Poor postnatal growth in preterm infants. Acta Paediatr. 111, 1458 (2022).
Ramel, S. E. et al. The relationship of poor linear growth velocity with neonatal illness and two-year neurodevelopment in preterm infants. Neonatology 102, 19–24 (2012).
Morgan, A. S., Mendonça, M., Thiele, N. & David, A. L. Management and outcomes of extreme preterm birth. BMJ 376, e055924 (2022).
Lucaccioni, L., Iughetti, L., Berardi, A. & Predieri, B. Challenges in the growth and development of newborns with extra-uterine growth restriction. Expert Rev. Endocrinol. Metab. 17, 415–423 (2022).
Cuestas, E., Aguilera, B., Cerutti, M. & Rizzotti, A. Sustained neonatal inflammation is associated with poor growth in infants born very preterm during the first year of life. J. Pediatr. 205, 91–97 (2019).
Synnes, A. & Hicks, M. Neurodevelopmental outcomes of preterm children at school age and beyond. Clin. Perinatol. 45, 393–408 (2018).
Bavineni, M. et al. Mechanisms linking preterm birth to onset of cardiovascular disease later in adulthood. Eur. Heart J. 40, 1107–1112 (2019).
Forbes, G. B. Relation of lean body mass to height in children and adolescents. Pediatr. Res. 6, 32–37 (1972).
Belfort, M. B. et al. Systemic inflammation in the first 2 weeks after birth as a determinant of physical growth outcomes in hospitalized infants with extremely low gestational age. J. Pediatr. 240, 37–43.e1 (2022).
Pfister, K. M. & Ramel, S. E. Linear growth and neurodevelopmental outcomes. Clin. Perinatol. 41, 309–321 (2014).
Bell, K. A. et al. Body composition measurement for the preterm neonate: using a clinical utility framework to translate research tools into clinical care. J. Perinatol. 42, 1550–1555 https://doi.org/10.1038/s41372-022-01529-9 (2022).
DeBoer, M. D. et al. Mice with infectious colitis exhibit linear growth failure and subsequent catch-up growth related to systemic inflammation and IGF-1. Nutr. Res. 39, 34–42 (2017).
Cirillo, F., Lazzeroni, P., Sartori, C. & Street, M. E. Inflammatory diseases and growth: effects on the GH–IGF axis and on growth plate. Int. J. Mol. Sci. 18, 1878 (2017).
DeBoer, M. D. et al. Systemic inflammation, growth factors, and linear growth in the setting of infection and malnutrition. Nutrition 33, 248–253 (2017).
Villar, J. et al. INTERGROWTH-21st very preterm size at birth reference charts. Lancet 387, 844–845 (2016).
Villar, J. et al. Postnatal growth standards for preterm infants: the Preterm Postnatal Follow-up Study of the INTERGROWTH-21(st) Project. Lancet Glob. Health 3, e681–e691 (2015).
Mazess, R. B., Barden, H. S., Bisek, J. P. & Hanson, J. Dual-energy x-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am. J. Clin. Nutr. 51, 1106–1112 (1990).
Godang, K. et al. Assessing body composition in healthy newborn infants: reliability of dual-energy x-ray absorptiometry. J. Clin. Densitom. 13, 151–160 (2010).
ICD-10 Version. https://icd.who.int/browse10/2016/en#/ (2016).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Ehrenkranz, R. A. et al. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 117, 1253–1261 (2006).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Chiang, M. F. et al. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmology 128, e51–e68 (2021).
American Academy of Pediatrics. Committee on Nutrition. Nutritional needs of the preterm infant. In Pediatric Nutrition 8th edn (eds Kleinman, R. E. & Greer, F. R.) 113–162 (American Academy of Pediatrics, 2019).
Champely, S. et al. pwr: Basic Functions for Power Analysis (2020).
Kim, S. ppcor: an R package for a fast calculation to semi-partial correlation coefficients. Commun. Stat. Appl. Methods 22, 665–674 (2015).
Jafari, M. & Ansari-Pour, N. Why, when and how to adjust your P values?. Cell J. 20, 604–607 (2019).
Kumar, P. & Seshadri, R. Neonatal morbidity and growth in very low birth-weight infants after multiple courses of antenatal steroids. J. Perinatol. 25, 698–702 (2005).
McElrath, T. F. et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am. J. Epidemiol. 168, 980–989 (2008).
Chisholm, K. M., Norton, M. E., Penn, A. A. & Heerema-McKenney, A. Classification of preterm birth with placental correlates. Pediatr. Dev. Pathol. 21, 548–560 (2018).
Mestan, K. et al. Placental inflammatory response is associated with poor neonatal growth: preterm birth cohort study. Pediatrics 125, e891–898 (2010).
Scharf, R. J., Stroustrup, A., Conaway, M. R. & DeBoer, M. D. Growth and development in children born very low birthweight. Arch. Dis. Child. Fetal Neonatal Ed. 101, F433–F438 (2016).
Ballinger, A. B., Azooz, O., El-Haj, T., Poole, S. & Farthing, M. J. Growth failure occurs through a decrease in insulin-like growth factor 1 which is independent of undernutrition in a rat model of colitis. Gut 46, 694–700 (2000).
Zemel, B. S. et al. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J. Clin. Endocrinol. Metab. 95, 1265–1273 (2010).
Heaney, R. P. Bone mineral content, not bone mineral density, is the correct bone measure for growth studies. Am. J. Clin. Nutr. 78, 350–351 (2003).
Mølgaard, C., Thomsen, B. L., Prentice, A., Cole, T. J. & Michaelsen, K. F. Whole body bone mineral content in healthy children and adolescents. Arch. Dis. Child. 76, 9–15 (1997).
Magnusson, A., Swolin-Eide, D. & Elfvin, A. Body composition and bone mass among 5-year-old survivors of necrotizing enterocolitis. Pediatr. Res. https://doi.org/10.1038/s41390-022-02236-z (2022).
Vohlen, C. et al. Dynamic regulation of GH-IGF1 signaling in injury and recovery in hyperoxia-induced neonatal lung injury. Cells 10, 2947 (2021).
Blair, C. et al. Liver IGF-1 mRNA expression is decreased by mechanical ventilation of preterm lambs. J. Investig. Med. 58, 105–105 (2010).
Löfqvist, C. et al. Low postnatal serum IGF-I levels are associated with bronchopulmonary dysplasia (BPD). Acta Paediatr. 101, 1211–1216 (2012).
DeBoer, M. D. & Denson, L. A. Delays in puberty, growth, and accrual of bone mineral density in pediatric Crohn’s disease: despite temporal changes in disease severity, the need for monitoring remains. J. Pediatr. 163, 17–22 (2013).
Wong, S. C. et al. Growth and the growth hormone-insulin like growth factor 1 axis in children with chronic inflammation: current evidence, gaps in knowledge, and future directions. Endocr. Rev. 37, 62–110 (2016).
Kubicky, R. A., Wu, S., Kharitonenkov, A. & De Luca, F. Role of fibroblast growth factor 21 (FGF21) in undernutrition-related attenuation of growth in mice. Endocrinology 153, 2287–2295 (2012).
Misra, M. et al. Alterations in growth hormone secretory dynamics in adolescent girls with anorexia nervosa and effects on bone metabolism. J. Clin. Endocrinol. Metab. 88, 5615–5623 (2003).
Yumani, D. F. J., Calor, A. K. & van Weissenbruch, M. M. The course of IGF-1 levels and nutrient intake in extremely and very preterm infants during hospitalisation. Nutrients 12, 675 (2020).
Cooke, R. J. & Griffin, I. Altered body composition in preterm infants at hospital discharge. Acta Paediatr. 1992 98, 1269–1273 (2009).
Tremblay, G. et al. Body composition in very preterm infants: role of neonatal characteristics and nutrition in achieving growth similar to term infants. Neonatology 111, 214–221 (2017).
Moldawer, L. L. & Copeland, E. M. Proinflammatory cytokines, nutritional support, and the cachexia syndrome: interactions and therapeutic options. Cancer 79, 1828–1839 (1997).
Roubenoff, R. Inflammatory and hormonal mediators of cachexia. J. Nutr. 127, 1014S–1016S (1997).
Giannì, M. L. et al. Adiposity in small for gestational age preterm infants assessed at term equivalent age. Arch. Dis. Child Fetal Neonatal Ed. 94, F368–F372 (2009).
Sauer, P. J. J. Can extrauterine growth approximate intrauterine growth? Should it? Am. J. Clin. Nutr. 85, 608S–613S (2007).
Sethi, J. K. & Vidal-Puig, A. J. Thematic review series: adipocyte biology. Adipose tissue function and plasticity orchestrate nutritional adaptation. J. Lipid Res. 48, 1253–1262 (2007).
Ramel, S. E. et al. Body composition changes in preterm infants following hospital discharge: comparison with term infants. J. Pediatr. Gastroenterol. Nutr. 53, 333–338 (2011).
Acknowledgements
The authors thank Nicholas Basily for editing the English language of this manuscript.
Funding
This study was supported by the Agencia Nacional de Promoción Científica y Tecnológica (FONCYT) grant PICT 2019-3062.
Author information
Authors and Affiliations
Contributions
E.C. conceptualized and designed the study, coordinated and supervised data collection, carried out the final data analyses, drafted the manuscript, and reviewed and revised the final manuscript. M.H., S.G., M.I.G., V.S. and A.R. designed the data collection instruments, manually collected data, carried out the initial analyses, and reviewed and revised the manuscript for important intellectual content. All authors have approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at Hospital Privado Universitario de Córdoba, and the infants’ parents gave written informed consent (HP 4-308). This study used anonymized and deidentified data, fulfilling local data protection regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cuestas, E., Hillman, M., Galetto, S. et al. Inflammation induces stunting by lowering bone mass via GH/IGF-1 inhibition in very preterm infants. Pediatr Res 94, 1136–1144 (2023). https://doi.org/10.1038/s41390-023-02559-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02559-5