Abstract
Background
Organ dysfunction (ODF) in late-onset bloodstream infection (LBSI) is associated with increased risk of adverse outcomes. However, no established definition of ODF exists among preterm neonates. Our objective was to describe an outcome-based ODF definition for preterm infants, and assess factors associated with mortality.
Methods
This is a six-year retrospective study of neonates <35 weeks gestational age, >72 h of age, with non-CONS bacterial/fungal LBSI. Discriminatory ability of each parameter for mortality was evaluated: base deficit ≤−8 mmol/L (BD8), renal dysfunction (urine output <1 cc/kg/h or creatinine ≥100 μmol/L), hypoxic respiratory failure (HRF, ventilated, FiO2 = 1.0), or vasopressor/inotrope use (V/I). Multivariable logistic regression analysis was performed to derive a mortality score.
Results
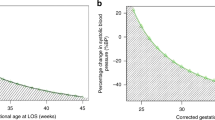
One hundred and forty-eight infants had LBSI. BD8 had the highest individual predictive ability for mortality (AUROC = 0.78). The combination BD8 + HRF + V/I was used to define ODF (AUROC = 0.84). Fifty-seven (39%) infants developed ODF, among which 28 (49%) died. Mortality increased inversely relative to GA at LBSI-onset (aOR 0.81 [0.67, 0.98]) and directly relative to ODF occurrence (12.15 [4.48, 33.92]). Compared to no-ODF, ODF infants had lower GA and age at illness, and higher frequency of Gram-negative pathogen.
Conclusions
Among preterm neonates with LBSI, significant metabolic acidosis, HRF, and vasopressor/inotrope use may identify infants high risk for mortality. These criteria could help identify patients for future studies of adjunctive therapies.
Impact
-
Sepsis-related organ dysfunction is associated with increased risk of adverse outcomes.
-
Among preterm neonates, significant metabolic acidosis, use of vasopressors/inotropes, and hypoxic respiratory failure may identify high-risk infants.
-
This can be used to target research and quality improvement efforts toward the most vulnerable infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during the current study are not publicly available due patient confidentiality; all analyzed data are included in this article.
References
Dong, Y. & Speer, C. P. Late-onset neonatal sepsis: recent developments. Arch. Dis. Child. Fetal Neonatal Ed. 100, F257–F263 (2015).
Klinger, G., Chin, C.-N., Beyene, J. & Perlman, M. Predicting the outcome of neonatal bacterial meningitis. Pediatrics 106, 477–482 (2000).
Lin, M.-C., Chi, H., Chiu, N.-C., Huang, F.-Y. & Ho, C.-S. Factors for poor prognosis of neonatal bacterial meningitis in a medical center in Northern Taiwan. J. Microbiol. Immunol. Infect. 45, 442–447 (2012).
Glass, H. C. et al. Clinical neonatal seizures are independently associated with outcome in infants at risk for hypoxic-ischemic brain injury. J. Pediatr. 155, 318–323 (2009).
Martens, S. E. et al. Is hypotension a major risk factor for neurological morbidity at term age in very preterm infants? Early Hum. Dev. 75, 79–89 (2003).
Volpe, J. J. Neurobiology of periventricular leukomalacia in the premature infant. Pediatr. Res. 50, 553–562 (2001).
Watkins, A., West, C. & Cooke, R. Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum. Dev. 19, 103–110 (1989).
Miall-Allen, V., De Vries, L. & Whitelaw, A. Mean arterial blood pressure and neonatal cerebral lesions. Arch. Dis. Child. 62, 1068–1069 (1987).
Bada, H. S. et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J. Pediatr. 117, 607–614 (1990).
Goh, G. L. et al. Risk factors for mortality from late-onset sepsis among preterm very-low-birthweight infants: a single-center cohort study from Singapore. Front. Pediatr. 9, 801955 (2021).
Turhan, E. E., Gürsoy, T. & Ovalı, F. Factors which affect mortality in neonatal sepsis. Turk. Arch. Pediatr. 50, 170 (2015).
Chakraborty, R. K. & Burns, B. Systemic Inflammatory Response Syndrome (StatPearls, 2019).
Matics, T. J. & Sanchez-Pinto, L. N. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatr. 171, e172352 (2017).
Fujishima, S. Organ dysfunction as a new standard for defining sepsis. Inflamm. Regener. 36, 1–6 (2016).
Goldstein, B., Giroir, B. & Randolph, A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 6, 2–8 (2005).
Hotchkiss, R. S. et al. Sepsis and septic shock. Nat. Rev. Dis. Prim. 2, 1–21 (2016).
Wynn, J. L. & Polin, R. A. A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr. Res. 88, 85–90 (2020).
Grace, J.-U. A. & Obara, S. K. A systematic review of coagulase-negative Staphylococci in neonatal sepsis. Clin. Microbiol. 8, 326 (2019).
Rennie, J. M. & Roberton, N. C. Textbook of Neonatology (Churchill Livingstone, 1999).
Srikrishna, S., Reddy, K. S. & Kiran, M. R. Correlation of metabolic acidosis in neonate with morbidity, mortality and neurodevelopmental outcome. Asian J. Clin. Pediatr. Neonatol. 7, 40–45 (2019).
Aramburo, A. et al. Lactate clearance as a prognostic marker of mortality in severely ill febrile children in East. Africa 16, 1–12 (2018).
Maitland, K. et al. Mortality after fluid bolus in African children with severe infection. N. Engl. J. Med. 364, 2483–2495 (2011).
Bruel, A. et al. Critical serum creatinine values in very preterm newborns. PLoS ONE 8, e84892 (2013).
Kellum, J. A. & Lameire, N. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit. Care 17, 204 (2013).
Kunitake, R. C., Kornblith, L. Z., Cohen, M. J. & Callcut, R. A. Trauma early mortality prediction tool (TEMPT) for assessing 28-day mortality. Trauma Surg. Acute Care Open 3, e000131 (2018).
Mohammad, M. A. et al. Development and validation of an artificial neural network algorithm to predict mortality and admission to hospital for heart failure after myocardial infarction: a nationwide population-based study. Lancet Digit. Health 4, e37–e45 (2022).
Graham, P. L. Simple strategies to reduce healthcare associated infections in the neonatal intensive care unit: line, tube, and hand hygiene. Clin. Perinatol. 37, 645–653 (2010).
Sadeghi, K. et al. Immaturity of infection control in preterm and term newborns is associated with impaired toll-like receptor signaling. J. Infect. Dis. 195, 296–302 (2007).
Schultz, C. et al. Immature anti‐inflammatory response in neonates. Clin. Exp. Immunol. 135, 130–136 (2004).
Kharrat, A. & Jain, A. Hemodynamic dysfunction in neonatal sepsis. Pediatr. Res. 91, 413–424 (2022).
Wynn, J. L. & Wong, H. R. Pathophysiology and treatment of septic shock in neonates. Clin. Perinatol. 37, 439–479 (2010).
Kermorvant-Duchemin, E., Laborie, S., Rabilloud, M., Lapillonne, A. & Claris, O. Outcome and prognostic factors in neonates with septic shock. Pediatr. Crit. Care Med. 9, 186–191 (2008).
Wilkinson, J. D. et al. Mortality associated with multiple organ system failure and sepsis in pediatric intensive care unit. J. Pediatr. 111, 324–328 (1987).
Leteurtre, S. et al. Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362, 192–197 (2003).
Proulx, F., Fayon, M., Farrell, C. A., Lacroix, J. & Gauthier, M. J. C. Epidemiology of sepsis and multiple organ dysfunction syndrome in children. Chest 109, 1033–1037 (1996).
Vincent, J. L. et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 22, 707–710 (1996).
Abraham, E. & Singer, M. Mechanisms of sepsis-induced organ dysfunction. Crit. Care Med. 35, 2408–2416 (2007).
Despond, O., Proulx, F., Carcillo, J. A. & Lacroix, J. Pediatric sepsis and multiple organ dysfunction syndrome. Curr. Opin. Pediatr. 13, 247–253 (2001).
Leclerc, F. et al. Cumulative influence of organ dysfunctions and septic state on mortality of critically ill children. Am. J. Respir. Crit. Care Med. 171, 348–353 (2005).
Typpo, K. V. et al. Day one MODS is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr. Crit. Care Med. 10, 562 (2009).
Agyeman, P. K. et al. Epidemiology of blood culture-proven bacterial sepsis in children in Switzerland: a population-based cohort study. Lancet Child Adolesc. Health 1, 124–133 (2017).
Duke, T., Butt, W. & South, M. Predictors of mortality and multiple organ failure in children with sepsis. Intensive Care Med. 23, 684–692 (1997).
Jat, K. R., Jhamb, U. & Gupta, V. K. Serum lactate levels as the predictor of outcome in pediatric septic shock. Indian J. Crit. Care Med. 15, 102 (2011).
Hatherill, M., Waggie, Z., Purves, L., Reynolds, L. & Argent, A. Mortality and the nature of metabolic acidosis in children with shock. Intensive Care Med. 29, 286–291 (2003).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810 (2016).
Schlapbach, L. J., Straney, L., Bellomo, R., MacLaren, G. & Pilcher, D. Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. Intensive Care Med. 44, 179–188 (2018).
Balamuth, F. et al. Protocolized treatment is associated with decreased organ dysfunction in pediatric severe sepsis. Pediatr. Crit. Care Med. 17, 817 (2016).
Wynn, J. L. Defining neonatal sepsis. Curr. Opin. Pediatr. 28, 135–140 (2016).
Abdel-Hady, H., Shouman, B. & Aly, H. Early weaning from CPAP to high flow nasal cannula in preterm infants is associated with prolonged oxygen requirement: a randomized controlled trial. Early Hum. Dev. 87, 205–208 (2011).
Peters, O., Ryan, S., Matthew, L., Cheng, K. & Lunn, J. Randomised controlled trial of acetate in preterm neonates receiving parenteral nutrition. Arch. Dis. Child. Fetal Neonatal Ed. 77, F12–F15 (1997).
Wernly, B. et al. Acidosis predicts mortality independently from hyperlactatemia in patients with sepsis. Eur. J. Intern. Med. 76, 76–81 (2020).
Plötz, F. B. et al. Effect of acute renal failure on outcome in children with severe septic shock. Pediatr. Nephrol. 20, 1177–1181 (2005).
Walker, O., Kenny, C. B. & Goel, N. Neonatal sepsis. Paediatr. Child Health 29, 263–268 (2019).
Mathur, N., Singh, A., Sharma, V. & Satyanarayana, L. Evaluation of risk factors for fatal neonatal sepsis. Indian Pediatr. 33, 817–822 (1996).
Chisti, M. J. et al. Clinical predictors and outcome of metabolic acidosis in under-five children admitted to an urban hospital in Bangladesh with diarrhea and pneumonia. PLoS ONE 7, e39164 (2012).
O’Dell, E., Tibby, S. M., Durward, A. & Murdoch, I. A. Hyperchloremia is the dominant cause of metabolic acidosis in the postresuscitation phase of pediatric meningococcal sepsis. Crit. Care Med. 35, 2390–2394 (2007).
Bissinger, R. et al. Secondary surfactant administration in neonates with respiratory decompensation. J. Perinatol. 28, 192–198 (2008).
Abdel Mohsen, A. H. & Amin, A. S. Risk factors and outcomes of persistent pulmonary hypertension of the newborn in neonatal intensive care unit of Al-Minya University hospital in Egypt. J. Clin. Neonatol. 2, 78–82 (2013).
Fahmey, S. S., Hodeib, M., Refaat, K. & Mohammed, W. Evaluation of myocardial function in neonatal sepsis using tissue Doppler imaging. J. Matern. Fetal Neonatal Med. 33, 3752–3756 (2020).
Verma, B., Daga, S. R. & Mahapankar, A. Persistent pulmonary hypertension among neonates with sepsis. Indian J. Pediatr. 73, 250–251 (2006).
Tomerak, R. H., El-Badawy, A. A., Hussein, G., Kamel, N. R. & Razak, A. R. A. Echocardiogram done early in neonatal sepsis: what does it add? J. Investig. Med. 60, 680–684 (2012).
Wong, J. et al. Inotrope use among extremely preterm infants in Canadian NICUs: variations and outcomes. Paediatr. Child Health 17, 34A–34A (2012).
Author information
Authors and Affiliations
Contributions
A.K. and A.J. conceived, designed, and planned the study, contributed to planning data extraction and analysis, interpretation of results, wrote first and final draft of the publication, and approved the final publication. M.B. and F.Z. contributed to data collection, critically reviewed the manuscript, and approved the final publication. D.W. critically reviewed the study design and the manuscript and approved the final publication. X.Y.Y. performed the statistical analysis and contributed to and approved the final publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Patient consent was not required for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kharrat, A., Zhu, F., Baczynski, M. et al. Organ dysfunction and mortality in preterm neonates with late-onset bloodstream infection. Pediatr Res 94, 1044–1050 (2023). https://doi.org/10.1038/s41390-023-02541-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02541-1