Abstract
Objective
To explore pediatric subspecialist distress and well-being during the pandemic, with a particular focus on relationships between compassion fatigue (CF), burnout (BO), and compassion satisfaction (CS), and physicians’ perception of “feeling valued” by their institution.
Methods
The Compassion Fatigue and Satisfaction Self-Test and a questionnaire of personal/professional characteristics were distributed electronically to pediatric subspecialists. Content analysis was performed for responses to the question “How has your institution made you feel valued?”
Results
During the 16-month study period, CF and BO scores significantly increased, and CS scores decreased over time. By Epoch 3, 52% of respondents did not feel valued by their employing institution. When controlling for the effect of time, CF and BO scores remained higher, and CS scores lower, in participants who did not feel valued by their institution. Themes from the content analysis of “value” included expressions of gratitude, perks vs. penalties, safety, and leadership. The same overture from leadership provoked disparate responses in recipients, seemingly over the sincerity behind the offering, which may reflect underlying workplace culture.
Conclusions
Increasingly, pediatric subspecialists are not feeling valued for their work. Institutional leadership must prioritize healthy workplace culture, and re-think emotional and mental health support within the health system.
Impact
-
A total of 52% of our study population did not “feel valued” by their employing institution by late 2021, which is cause for concern.
-
This is the first longitudinal analysis of distress and well-being in a national cohort of pediatric subspecialists during the COVID-19 pandemic.
-
The same overture or messaging from leadership sparked disparate responses in recipients, seemingly over the sincerity behind the offering, which relates to the underlying workplace culture of the department or institution.
-
Institutional leadership must prioritize a healthy workplace culture, and re-think and re-invent emotional and mental health support within the health system.
Similar content being viewed by others
Introduction
Physicians caring for children have faced unique challenges during the SARS-CoV-2 (COVID-19) pandemic. Though COVID-19 has been perceived to be a virus that largely spares young people, children and families have been subject to significant consequences of the ongoing pandemic.1,2,3,4 Pediatric COVID-19 cases have increased over time and caused rare but critical complications such as cardiac sequelae and multisystem inflammatory syndrome in children.5,6 In addition, children have suffered psychosocial morbidities, including anxiety and depression, as a result of the pandemic’s substantial disruption to school, home life, and social networks.2,3 Vaccine development for children has lagged significantly, resulting in higher risk for pediatric providers exposed to a largely unvaccinated patient population, and increased stress for parents of young children.7,8 The impact of these challenges on the mental health of pediatric physicians has been largely unexamined.
The practice of medicine during the COVID-19 pandemic has led to “epidemic” levels of burnout (BO) across healthcare roles, disciplines, and specialties.9,10,11,12,13,14 Many physicians have also suffered acute stress, post-traumatic stress, and secondary traumatic stress or compassion fatigue (CF) after 2 years of intense exposure to patient suffering and death.15,16,17,18 CF and BO have likely contributed to providers leaving healthcare, resulting in severe staffing shortages in all roles.19,20 While compassion satisfaction (CS), the professional satisfaction engendered through providing patient care and “caring” about one’s patients,21 is thought to mitigate the effects of CF and BO, little is known about how it has impacted physicians’ distress during the pandemic. Even less is known about how institutions have supported physicians in order to foster CS and limit CF and BO during this unprecedented time.
Because pandemic-related challenges have differed for providers caring for adults and those caring for children, we sought to better understand the impact of the COVID-19 pandemic on the mental health of pediatric subspecialists. In our foundational work, we characterized CF, BO, and CS in national cohorts of pediatric subspecialists (neonatologists, and palliative care, critical care, emergency medicine, and hematology-oncology physicians) prior to the COVID-19 pandemic.22,23,24,25,26 More recently, we compared pre-pandemic CF, BO, and CS scores in this group of pediatric subspecialists with scores obtained early in the pandemic.27 In our current study, we continued our exploration of pediatric physician distress and well-being in the latter half of 2020 and in 2021, with a particular focus on the relationship between CF, BO, and CS scores and physicians’ perception of “feeling valued” by their institution.
Methods
Survey
To assess physician distress and well-being, we invited potential subjects to complete a survey that included a questionnaire (Supplementary Material 1) and the modified Compassion Fatigue and Satisfaction Self-Test (CFST, Supplementary Material 2). The questionnaire included demographic information (pediatric subspecialty, U.S. geographic location, age, sex, race, and household members), professional roles and responsibilities, sources of distress, activities to off-set work-related distress, supports and programs available through the participant’s place of employment, and self-appraisal of extent of physical exhaustion and emotional depletion. Participants were also asked to reflect and respond to the sentiments “I have put myself at significant risk as part of my clinical work” and “My institution has valued my contribution to the COVID-19 crisis” using a 5-point Likert scale (0 = strongly disagree; 1 = disagree; 2 = neutral; 3 = agree; 4 = strongly agree) and/or a free text response. The modified CFST is a well-validated instrument that contains 54 statements, with 18, 13, and 23 items on the CF, BO, and CS scales, respectively. It uses a 5-point Likert scale (0 = never; 1 = rarely; 2 = a few times; 3 = somewhat often; 4 = often; 5 = very often) for participants to quantify the frequency of experiencing the content in each statement.15,22,23,24,25,26
Subjects
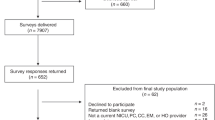
This study was designated as exempt human subjects’ research by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai. Email addresses for pediatric subspecialists in neonatology, palliative care, critical care, emergency medicine, and hematology-oncology, compiled in our previous studies of CF, BO, and CS,22,23,24,25,26 were used to contact potential subjects for the current study. Invitations to participate, which consisted of a brief description of the study and a hyperlink to the survey, were distributed anonymously by Survey Monkey to potential subjects in June–July 2020 (Epoch 1, data previously published,27 December 2020–January 2021 (Epoch 2), and September–October 2021 (Epoch 3). At each survey time point, participants were asked to reflect and respond based on their experiences in the prior 6 months.
Data analysis
Responses were coded and SPSS Statistics, Version 24 (IBM, Armonk, NY) was utilized for all analyses. Our previously published, early pandemic data (Epoch 1, collected in June–July 202027) was included in the analyses described below. Descriptive statistics were performed for the demographic elements of the survey. As in our prior work, CF, BO, and CS scores for each participant were derived by summing the Likert value for each statement in the relevant subscale.22,23,24,25,26 Pearson’s r was used to examine correlations between subscales. For the statements “I have put myself at significant risk as part of my clinical work” and “My institution has valued my contribution to the COVID-19 crisis”, responses were dichotomized into “agree” (combining Likert scale options “agree” and “strongly agree”) or “disagree” (combining Likert scale options “neutral”, “disagree”, “strongly disagree”).
Univariate analyses were used to compare the characteristics of the study population over the three time epochs surveyed. One-way between-groups analyses of variance were done to examine the impact of time epoch on CF, BO, and CS scores. Two-way analyses of variance were performed to explore the impact of time on CF, BO, and CS scores in relation to selected additional factors of interest: subspecialty, sex, U.S geographic region, and the sentiments “I have put myself at significant risk as part of my clinical work” and “My institution has valued my contribution to the COVID-19 crisis”. Qualitative content analysis was performed for free text answers to the question “How has your institution made you feel valued during the SARS-CoV-2 pandemic?”
Results
A total of 499 surveys from Epoch 1, 314 surveys from Epoch 2, and 260 surveys from Epoch 3 were included in our analysis (survey response rates 26%, 17%, and 16%, respectively). The demographics of the study population are presented in Table 1. The majority of participants self-identified as white and female. Participants were fairly evenly distributed geographically across the U.S. With the exception of fewer neonatologists participating in Epoch 3 (vs. Epoch 1, p = 0.024), there were no significant differences in the demographic composition of the study population over time.
Participant distress and coping strategies
Details of participant distress and coping strategies are shown in Table 2. The most commonly reported sources of distress changed over time. In later epochs, more participants expressed concern about their “mental health” and were distressed over “witnessing frequent patient suffering and death”, while fewer respondents worried about “economic uncertainty” and “uncertain future”. More participants expressed concern about “family health” and “social isolation” in Epoch 2 than at earlier or later time points. Personal coping strategies remained remarkably constant over time, with the exception of “socializing” and use of “professional mental health services”, both of which increased significantly in Epoch 3. The availability of some workplace wellness activities significantly increased over time (peer support, Schwartz Rounds, and pet therapy), while others (holistic activities and team building) significantly decreased. Of note, by Epoch 3, 52% of participants did not feel their contribution to the pandemic was valued by their employing institution, which was a significant decline from Epochs (Table 2).
Compassion fatigue, burnout, and compassion satisfaction: changes over time
CF, BO, and CS scores over the three time epochs are presented in Table 3. CF and BO scores significantly increased, and CS scores significantly decreased over time. When controlling for the effect of time, CF and BO scores remained significantly higher, and CS scores significantly lower, in participants who did not feel valued by their employing institutions (Fig. 1). Similar results were obtained when examining the impact of time and the sentiment, “I have put myself at significant risk as part of my clinical work” on CF, BO, and CS scores, with nearly 40% of study participants affirming the statement “I have put myself at significant risk as part of my clinical work” (data not shown). When controlling for the effect of time, we considered three additional factors that might significantly impact CF, BO, and CS scores: subspecialty, gender, and U.S. geographic location. When controlled for the effect of time, subspecialty had no significant impact on CF or CS scores. However, a significant effect of subspecialty on BO score was identified, with higher BO scores in pediatric critical care physicians when compared with neonatologists (p = 0.008) and pediatric emergency medicine physicians (p = 0.030). When controlling for the effect of time, gender had no significant effect on BO or CS scores. There was, however, a significant impact of gender on CF score, with higher scores identified in females (p = 0.000). When controlling for the effect of time, geographic location had no significant effect on CF, BO, or CS scores.
a Compassion fatigue scores over time (Epoch 1 = June/July 2020, Epoch 2 = December 2020/January 2021, Epoch 3 = September/October 2021). b Burnout scores over time (Epoch 1 = June/July 2020, Epoch 2 = December 2020/January 2021, Epoch 3 = September/October 2021). c Compassion satisfaction scores over time (Epoch 1 = June/July 2020, Epoch 2 = December 2020/January 2021, Epoch 3 = September/October 2021).
Sense of feeling valued
Over time, significantly fewer participants felt valued by their employing institution (p = 0.002). We reviewed participant free text responses to the question, “How has your institution made you feel valued during the SARS-CoV-2 pandemic?” and organized them into themes. Themes that emerged included: expressions of gratitude (verbal or written), perks (gained or retained) vs. penalties, safety, and leadership (Table 4). Positive and negative comments were returned for each category. For the theme “expressions of gratitude”, one respondent commented: “…Almost constant positive feedback. Frequent check-ins with other members of my team. Recognition by our medical director when someone needs extra help, support, or time off”. Another participant reported: “They tell me they value me. They ask for my opinion about things. They keep me informed. They are clearly taking this seriously.” Other respondents expressed frustration with and an impression of insincerity in the verbal and written expressions of gratitude they received: “It feels like lip service. We are interchangeable cogs in a wheel. They need us, but they don’t care about us”; “They say it, but I don’t feel it. It seems very much ‘same old, same old’”; and “I feel unappreciated and frankly abused by my institution”.
Perks were recognized as both items gained and items retained. Participants most often reported receiving “free food” and “small gifts”. Others described “financial support”, such as “pay raises”, “small bonuses”, and “free childcare”. Some respondents viewed not having their compensation or benefits reduced as a perk. Others expressed dismay: “salary cuts and constant focus on financial hardship signifies a lack of respect for what we provide the hospital”; “by decreasing our salaries and benefits during our most dire time of exposure on a daily basis, it is clear our employers do not value our contribution as frontline workers to this pandemic”; and “a lot of talk about how we are heroes. But it’s hard to feel that way when budgets are tight. Personally I have not had a salary decrease but am working more for the same salary…”
Attention to physician safety, in the form of “PPE provided”, “early access to vaccines”, “always reassessing safety protocols” and “following recommended protocol”, was viewed by many participants as an expression of value. Others felt frustrated and disrespected: “at the beginning of the pandemic, I was asked not to wear a mask. This was humiliating and it really showed me that we…did not matter and neither did the patients we see” and “our leadership actually wrote us up for wearing N95s”. Leadership was described favorably by some respondents as “visible…good role modeling…accessible” and “increased integration between hospital administrators and clinicians…excellent engagement with physician leaders…communication has been consistent, clear, and at an appropriate frequency”. Another participant commented “…they continue to make terrible leadership decisions with our lack of adequate RN staffing. Instead they… send[ing] out values-oriented emails which provide no functional support….nauseating.”
Discussion
We present the first longitudinal analysis of distress and well-being in a national cohort of pediatric subspecialists during the COVID-19 pandemic. The evolution in number, complexity, and severity of pediatric COVID-19 cases over time during the pandemic has transformed the clinical landscape for many pediatric subspecialists.5,6 It is perhaps, then, not surprising that nearly 40% of study participants agreed with the statement “I have put myself at significant risk as part of my clinical work”. CF and BO scores were significantly higher and CS scores lower for participants who felt themselves at increased risk.
Beyond a sense of profound risk, sources of participant distress shifted over the study period. Significantly more participants were concerned about their mental health, and specifically about “witnessing frequent patient suffering and death,” which is well known to lead to CF,15,28,29,30 at later time points in the pandemic. At the same time, while most personal coping strategies did not change, there was a parallel increase in the number of participants “socializing” and “using professional mental health services” later in the pandemic. With increasing adult vaccination rates and easing of social distancing restrictions, more and safer opportunities for social gathering may have become more accessible later in the pandemic. We cannot know with certainty what led to these changes. It may also be, for example, that physicians grew tired of pandemic-related restrictions and chose to socialize more liberally, regardless of the safety of such activities. Historically, physicians have been reluctant to seek out mental health services for fear of stigma in the workplace if discovered by an employer or licensing board.31 The shift in seeking mental healthcare outside of the workplace in our study cohort may indicate a change in perception, or simply increased need due to intolerable levels of distress. It is possible that the shift in perceived sources of stress may have also led to more physician awareness that usual coping strategies were insufficient.
Over a 16-month period, we identified a significant increase in CF and BO scores in parallel with a significant decrease in CS scores. Why female participants had higher CF scores than their male counterparts is unclear but particular attention should be paid to the unique emotional stressors placed on female physicians and ways these might be mitigated.1 Over that 16-month period, the percentage of participants who “felt valued” by their employing institution fell significantly from 61% to 48%. After controlling for the effect of time, we found that CF and BO scores remained significantly higher, and CS scores significantly lower, in participants who did not “feel valued” by their employing institution, suggesting that factors relating to institutional leadership, messaging, and culture may play an important role in these changes.
That less than half of our study population “felt valued” by their employing institution by Epoch 3 of the pandemic is cause for concern. The themes identified in our content analysis for free text answers to this prompt echo prior literature,32,33 and offer clues as to how institutional leadership might work to show that physicians are valued. Supportive institutional leadership is integral to promoting a healthy workplace culture that helps to mitigate physician distress.34 One theme that emerged was that the same overture or messaging from leadership can spark disparate responses in recipients, ranging from feelings of “value” for some to “insult” for others, seemingly over the sincerity behind the offering. We speculate that the perception of sincerity (or lack thereof) relates to the underlying workplace culture of the department or institution. While we did not specifically query participants about how institutions expressed “sincerity”, this theme emerged in our thematic analysis. It is an interesting area for future research, not only because it seemed important to participants, but also because it might be useful to institutional leadership to understand what they can do to be perceived as “sincere”.
Ultimately, provision of a safe work environment by ensuring adequate personal protective equipment and well-defined, consistently articulated safety protocols should be baseline essentials in any workplace.35 However, participant responses suggest that at many institutions, such essentials were elevated to the status of a “perk,” which may have further impacted the extent to which physicians felt valued. In addition, many participants expressed they felt “valued” by being spared a pay cut, a reduction in benefits, or a furlough, when one might anticipate that “value” would be perceived through a raise, bonus, or promotion. Together, these findings suggest opportunities for institutions to reconsider how they show value to their physician employees, and likely others.
Limitations
There are several limitations to our study. The survey response rate was low and decreased over time, although it was within range of the response rates for our previous surveys on physician distress in this population of subspecialists,22,23,24,25,26 and for other web-based surveys in subspecialists.36 Over the 16-month study period, the response rate decreased for each time epoch. This may be related to increasing levels of overwork and weariness in healthcare workers as the pandemic progressed. As with all surveys, there is the risk of non-response bias.36 It is possible that individuals with the greatest levels of distress chose not to participate, or the reverse may be true. The generalizability of our findings may be limited by the fact that the majority of study participants were white and female, although this mirrors the demographic make-up for pediatric providers in general. We cannot know the influence of confounding factors outside of the workplace which may have worsened the impact of COVID on individual physicians’ personal health and the health of their families. Finally, while we asked participants how their institution made them feel valued, we did not ask how their institutions made people feel undervalued. This would be an interesting area for future study.
Conclusions
After 2 years of unprecedented stress, clinical challenges, and vigilance, pediatricians are mentally and physically exhausted. This exhaustion is cumulative; there is no full recovery to baseline after each COVID-19 wave with interim relief.19,20,37,38,39,40,41 Increasing numbers of contemporary physicians are not feeling valued for the work they do and the risks they take. This is occurring against a backdrop of a shifting public reaction to physicians, healthcare workers, science, and a healthcare system teetering on the brink of collapse.35,37,41,42,43 Institutional leadership must prioritize a healthy workplace culture, and re-think and re-invent emotional and mental health support within the health system. Without such action, our system will fail not only physicians, but all who need medical care, and especially the most vulnerable among us.
Data availability
All datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Frank, E. et al. Experiences of work-family conflict and mental health symptoms by gender among physician parents during the COVID-19 pandemic. JAMA Netw. Open. 4, e2134315 (2021).
Krass, P., Dalton, E., Doupnik, S. K. & Esposito, J. US Pediatric Emergency Department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw. Open. 4, e218533 (2021).
Loades, M. E. et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 59, 1218–1239.e3 (2020).
Feinberg, M. E. et al. Impact of the COVID-19 pandemic on parent, child, and family functioning. Fam. Process. 61, 361–374. https://doi.org/10.1111/famp.12649 (2022).
American Academy of Pediatrics. Children and COVID-19: State-level Data Report. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ (2022).
Feldstein, L. R. et al. Characteristics and outcomes of us children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA 325, 1074–1087 (2021).
Rezaei, N. COVID-19 affects healthy pediatricians more than pediatric patients. Infect. Control Hosp. Epidemiol. 49, 1106–1107 (2020).
de St. Maurice, A. et al. Pediatrician’s role in vaccinating children and families for COVID-19: no one left behind. Pediatr. Res. 90, 1105–1107 (2021).
Maslach, C. & Jackson, S. E. The measurement of experienced burnout. J. Organ. Behav. 2, 99–113 (1981).
Lai, J. et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 3, e203976 (2020).
Salazar de Pablo, G. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275, 48–57 (2020).
Hummel, S. et al. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study. J. Med. Internet Res. 23, e24983 (2021).
Prasad, K. et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine 35, 100879 (2021).
Rodriguez, R. M. et al. Symptoms of anxiety, burnout, and PTSD and the mitigation effect of serologic testing in emergency department personnel during the COVID-19 pandemic. Ann. Emerg. Med. 78, 35–43 (2021).
Figley, C. R. (ed.) Compassion fatigue as secondary traumatic stress disorder: an overview. In: Compassion Fatigue 1–20 (Taylor & Francis Group, New York, NY, 1995).
Schecter, A. et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 6, 1–8 (2020).
Schwartz, R. M. et al. The impact of physicians’ COVID-19 pandemic occupational experiences on mental health. J. Occup. Environ. Med. 64, 151–157 (2022).
Van Wert, M. J. et al. Healthcare worker mental health after the initial peak of the COVID-19 pandemic: a US medical center cross-sectional survey. J. Gen. Intern. Med. 37, 1169–1176 (2022).
Levine, D. U.S. faces crisis of burned-out health care workers. US News and World Report. https://www.usnews.com/news/health-news/articles/2021-11-15/us-faces-crisis-of-burned-out-health-care-workers (15 November 2021).
Yong, E. Why health-care workers are quitting in droves. The Atlantic. https://www.theatlantic.com/health/archive/2021/11/the-mass-exodus-of-americas-health-care-workers/620713/ (16 November 2021).
Stamm, B. H. Measuring compassion satisfaction as well as fatigue: developmental history of the compassion satisfaction and fatigue test. In Treating Compassion Fatigue (ed. Figley, C. R.) 107–119 (Routledge, New York, NY, 2002).
Weintraub, A. S., Geithner, E. M. & Waldman, E. D. Compassion fatigue, burnout, and compassion satisfaction in neonatologists in the US. J. Perinatol. 36, 1021–1026 (2016).
Kase, S. M., Waldman, E. D. & Weintraub, A. S. A cross-sectional pilot study of compassion fatigue, burnout, and compassion satisfaction in pediatric palliative care providers in the United States. Palliat. Support. Care 17, 269–275 (2019).
Gribben, J. L., Kase, S. M., Waldman, E. D. & Weintraub, A. S. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric critical care physicians in the United States. Pediatr. Crit. Care Med. 20, 213–222 (2019).
Gribben, J. L., MacLean, S. A., Pour, T., Waldman, E. D. & Weintraub, A. S. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric emergency medicine physicians in the United States. Acad. Emerg. Med. 26, 732–743 (2019).
Weintraub, A. S., Sarosi, A., Goldberg, E. & Waldman, E. D. A cross-sectional analysis of compassion fatigue, burnout, and compassion satisfaction in pediatric hematology-oncology physicians in the United States. J. Pediatr. Hematol. Oncol. 42, e50–e55 (2020).
Kase, S. M., Gribben, J. L., Guttmann, K. F., Waldman, E. D. & Weintraub, A. S. Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic. Pediatr. Res. 91, 143–148 (2022).
Meadors, P., Lamson, A., Swanson, M., White, M. & Sira, N. Secondary traumatization in pediatric healthcare providers: compassion fatigue, burnout, and secondary traumatic stress. Omega 60, 103–1288 (2009).
van Mol, M. M., Kompanje, E. J., Benoit, D. D., Bakker, J. & Nijkamp, M. D. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS One 10, e0136955 (2015).
Laor-Maayany, R. et al. Compassion fatigue among oncologists: the roles of grief, sense of failure, and exposure to suffering and death. Support. Care Cancer 28, 2025–2031 (2020).
Cho, H. L. & Huang, C. J. Why mental health-related stigma matters for physician wellbeing, burnout, and patient care. J. Gen. Intern. Med. 35, 1579–1581 (2020).
Adeyemo, O. O., Tu, S. & Keene, D. How to lead health care workers during unprecedented crises: a qualitative study of the COVID-19 pandemic in Connecticut, USA. PLoS One 16, e0257423 (2021).
Razu, S. R. et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: a qualitative inquiry from Bangladesh. Front. Public Health 9, 647315 (2021).
Dewey, C., Hingle, S., Goelz, E. & Linzer, M. Supporting clinicians during the COVID-19 pandemic. Ann. Intern. Med. 172, 752–753 (2020).
Kirsch, T. What happens if health-care workers stop showing up? The Atlantic. https://www.theatlantic.com/ideas/archive/2020/03/were-failing-doctors/608662/ (24 March 2020).
Cunningham, C. T. et al. Exploring physician specialist response rates to web-based surveys. BMC Med. Res. Methodol. 15, 32 (2015).
Wolfe, J. Coronavirus briefing: a burnout crisis. The New York Times. https://www.nytimes.com/2022/01/14/briefing/coronavirus-briefing-a-pandemic-burnout-crisis.html (14 January 2022).
Jauhar, S. You know what would help exhausted doctors and nurses? More money. The New York Times. https://www.nytimes.com/2022/01/08/opinion/hazard-pay-covid-nurse-doctor.html (8 January 2022).
Wan, W. Burned out by the pandemic, 3 in 10 health-care workers consider leaving the profession. The Washington Post. https://www.washingtonpost.com/health/2021/04/22/health-workers-covid-quit/ (22 April 2021).
Jacobs, A. Frontline health care workers aren’t feeling the ‘Summer of Joy”. The New York Times. https://www.nytimes.com/2021/07/01/health/covid-nurses-doctors-burnout.html (1 July 2021).
Kisner, J. What the chaos in hospitals is doing to doctors. The Atlantic. https://www.theatlantic.com/magazine/archive/2021/01/covid-ethics-committee/617261/ (8 December 2020).
Yong, E. Hospitals are in serious trouble. The Atlantic. https://www.theatlantic.com/health/archive/2022/01/omicron-mild-hospital-strain-health-care-workers/621193/ (7 January 2022).
Thomas, S. The COVID-19 pandemic is breaking the U.S. healthcare system–but that’s only a symptom of the underlying disease. Forbes. https://www.forbes.com/sites/coronavirusfrontlines/2022/01/19/the-covid-19-pandemic-is-breaking-the-us-healthcare-system--but-thats-only-a-symptom-of-the-underlying-disease/?sh=45a4735841ee (19 January 2022).
Author information
Authors and Affiliations
Contributions
J.L.G., S.M.K., K.F.G., E.D.W. and A.S.W. made substantial contributions to study conception and design; J.L.G. and S.M.K. to data acquisition; A.S.W. to data analysis; J.L.G., S.M.K., K.F.G. and A.S.W. to writing the first draft of the manuscript; E.D.W. to critical revision of the manuscript for important intellectual content. All authors approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This project was designated as exempt human research by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai. Participants consented to the research by clicking “I agree” before beginning the survey.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gribben, J.L., Kase, S.M., Guttmann, K.F. et al. Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value. Pediatr Res 94, 581–587 (2023). https://doi.org/10.1038/s41390-023-02474-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02474-9
This article is cited by
-
Compassion fatigue in healthcare providers: a scoping review
BMC Health Services Research (2023)