Abstract
Background
There is no consensus on the benefits of physical activity (PA) regarding upper respiratory tract infections (URTIs) among children. This study aimed to determine an association between the PA level and URTIs in preschoolers.
Methods
In 4–7-year-old participants, URTI symptoms were monitored using the Polish version of the Wisconsin Upper Respiratory System Survey for Kids. The daily number of steps, PA intensity, and sleep duration were measured with a Garmin-vivofit pedometer. The lag effect between the initial level of daily PA and the frequency of infections was evaluated.
Results
The average daily step count from healthy days was a significant determinant of the total number of days with the URTI symptoms, and it accounted for 44% (p < 0.001) of this variable variance. A low level of baseline PA (initial 14-day “run-in” observation period) was associated with an increased risk of URTI. In the non-sport group, the severity of the URTI symptoms depended on the number of daily steps. No significant correlation was found between sleep duration and the number of URTI days.
Conclusion
Low levels of PA in preschoolers result in increased susceptibility to respiratory infections. Parents should encourage children to engage in PA to prevent URTIs.
Impact
-
In pre-school children, higher physical activity (PA) is associated with fewer days of upper respiratory tract infection symptoms (URTIS).
-
Children with a higher average daily step count have fewer days with URTIS over a long-term observation period.
-
A change in the average number of steps per day by 1000 changed the number of days with symptoms of URTI by 4 days.
-
The severity of URTIS was inversely related to the degree of PA.
-
Children who participate in sports 3 or more hours per week have fewer URTIS than those who do not engage in sports regularly.
Similar content being viewed by others
Introduction
Respiratory tract infections (RTIs) continue to pose significant clinical and economic problems worldwide.1,2 In the United States, upper respiratory tract infections (URTIs) impose a direct and indirect cost burden of approximately $40 billion on the economy3 and account for 10% of all outpatient and emergency department visits.4 In Europe, for the pre-pandemic influenza seasons from 2001 to 2009, the direct medical cost of acute RTIs equaled Euro 100 million annually in the UK.5
Pre-school children (up to 6 years of age) are especially vulnerable to infections due to their immature immune and respiratory systems.6 Even in the absence of any primary pathological condition, they experience numerous episodes of URTIs. Though generally mild and resolving spontaneously, such episodes can affect the patient’s quality of life (QoL), cause parental distress, and in the long-term, lead to family dysfunction, occupational disruption, and health care burden.7,8
The most common causes of RTIs in the pediatric population are respiratory viruses such as rhinoviruses, respiratory syncytial viruses, influenza and parainfluenza viruses, and seasonal coronaviruses.8 Several factors have been held responsible for children’s increased susceptibility to frequent respiratory infections. These can be divided into two groups: non-modifiable, such as (i) the function of local immune mechanisms, particularly nonspecific immunity in the respiratory system,9 (ii) asthma, allergies, and atopy in the family, (iii) anatomical abnormalities such as craniofacial or airway abnormalities2,6,8,10 and modifiable, like (i) exposure to tobacco smoke and air pollution,11,12 (ii), presence in crowded places (kindergartens and nurseries).13,14 Other rarely analyzed risk factors impacting RTI prevalence include exposure to livestock, including pets, and behavioral factors such as pacifier use and the amount and quality of physical activity (PA).6,9,13
The beneficial effects of PA on the physical health of children and adolescents have been chronicled in the literature for long and include improvements in the metabolic profile, bone mineral density, cardiorespiratory fitness, and insulin sensitivity.15 World Health Organization (WHO) guidelines recommend an average of 60 min of moderate-to-vigorous PA (MVPA) per day for all ages.16 PA is also defined as a limited time spent passively (i.e., “any waking behavior characterized by an energy expenditure of ≤1.5 metabolic equivalents, while seated, lying down, or sprawled out”17) in front of the screen, sitting in cars, and reading.18
PA level is generally determined based on the number of steps taken per day, ascertained through pedometers or accelerometers, a method accepted by researchers, practitioners, and the public.19 Results of reports examining the association between regular PA and the frequency and severity of URTIs in the pediatric population are inconclusive.20,21,22,23 Furthermore, most studies in this regard concern older children21,22,23 with few studying such association in preschoolers. Therefore, this study aimed to ascertain whether there is an association between an active lifestyle, specifically the level of PA expressed as the average daily number of steps, and recurrent URIs in pre-school children, considering environmental and familial factors.
Methods
Study design
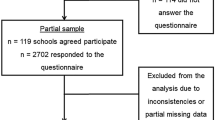
The study was conducted as per the protocol published in 2019,24 which describes the study design (details in Fig. 1). A cross-sectional study conducted on a single population, the research was managed and monitored by the Department of Pediatric Pneumonology and Allergy, Medical University of Warsaw, Warsaw.
Based on the study protocol published in 2019.24
Setting
The research was conducted in three kindergartens in the Warsaw city region (Poland) in 2018. Data were collected in the autumn and winter seasons. The study was approved by the Bioethics Committee of the Medical University of Warsaw. In the beginning, parents or legal guardians signed a written consent to their child’s participation in the study and received participant information sheets containing all relevant details about the purpose and course of the study, possible inconveniences related to participation, the possibility of withdrawing at will.24
Participants
The study included pre-school children aged 4–7, both boys and girls who attend pre-school regularly and who met the inclusion criteria.24 We included both children regularly engaging in sports (in the parents’ questionnaire we defined regular sports activities as equal to or more than 3 h a week) and children not engaging in sports activities.
Sample size
The aim was to study the target population of children aged 4–7 years from the Mazowieckie Voivodeship. A Simple Size Calculator25 was used to determine the number of people in the target study cohort. The following assumptions were made: 95% confidence level, 0.5 proportion, 0.1 confidence interval and 0.05 standard error. It was also assumed that around 10% of the results could potentially be excluded from the study as “incomplete”. Ultimately, our study was selected from a final cohort of approximately 110 participants.24
Measurements
Health status, lifestyle factors
At the beginning of the fall–winter season, parents of pre-school children received a two-part questionnaire package consisting of qualifications and a personal questionnaire. The first part outlined the eligibility criteria, while the second discussed issues such as PA, health status, and risk factors that might affect the study. The data from the questionnaires formed the basis for establishing the research group. This questionnaire was developed by the authors specifically for the study.24
PA measurement
Eligible children were given activity trackers to measure their daily step count, average exercise intensity, and sleep time. The monitoring device was Vivofit® fitness band (Garmin Ltd., Olathe Kansas). Each child wore the armband 24 h a day for 40 days. Participants were instructed to remove the band while bathing and periodically verify their skin for blemishes or allergies.24 The amounts of PA intensity levels were retracted from the Vivofit® fitness band and established based on the Garmin-patented algorithm system adjusted for the age of the participants.
URTI measurement
At the same time, parents/guardians were given a set of 60 questionnaires, one daily, to assess URTI symptoms daily. The Polish version of validated previously26 the Wisconsin Upper Respiratory System Survey for Kids (WURSSk–PL) was used. The questionnaires were completed for 60 days by the subject, with parental assistance. Regarding the questionnaire, the role of the parent was to clearly read the questions and link the selection of answers appropriate to the child’s intentions. We named the part of the questionnaire on the occurrence and severity of somatic symptoms of infection (runny nose, stuffy nose, sneezing, sore throat, cough, feeling tired) as the symptoms subscale. A score of 360 points on this subscale means no symptoms during the 60-day observation period. A group of questions regarding well-being and activity (thinking, sleeping, breathing, talking, walking, going to school, playing) was named a function subscale.
Statistical analysis
Quantitative and categorical variables were described by methods of descriptive statistics. The following measures were determined for quantitative variables: central tendency (mean), dispersion (± standard deviation, SD), and location (min–max). For categorical variables, a number (N) and frequency (%) were determined. The selected quantitative variables are presented in box plots. The effect of independent variables on the dependent variable (the number of days with UTRI) was estimated by a general multivariate regression. To clarify which predictors significantly affect the number of days with symptoms of RTI, a moderator stepwise regression model was built. Predictor collinearity was evaluated by calculating two indices: variance inflation factor (VIF) and tolerance.27 The predictors were introduced into the model using forward selection, which is a type of stepwise regression that starts with the null model and adds the fields one by one. The determined standardized regression coefficient for the main relationship (average number of steps per day (on healthy days) → number of days with UTRI) was adjusted for the effects of other independent variables, viz., sex, age, BMI, passive PA, regular sports, smoking, amount of sleep, allergy to hair and vaccinations.
The lag effect was estimated by calculating the average number of steps on infection-free days over the first 14 days of observation. This average was correlated with the cumulative number of days with an infection that occurred after the 15th day of observation (up to day 60).
The interaction between the moderator (sport vs non-sport group or less-active vs active group) and the additional independent variable was estimated by analysis of covariance (ANCOVA). An ANCOVA model with different slopes was used.
To assess the degree of explanation of variability for both regression models, the values of the adjusted R2 statistics were determined. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using the STATISTICA™ 13.3 software (TIBCO® Software, Inc., Palo Alto, California).
Results
Participants’ characteristics
The group of 104 children (55 girls) aged 4–7 years (mean ± SD: 5.3 ± 0.6 years) was analyzed in the present study. The group’s characteristics were as follows: median body mass 18.0 kg (range: 15.0–30.0 kg); mean stature, 112.9 ± 4.4 cm (range: 98.0–123.0 cm); median BMI, 14.6 kg/m2 (range: 11.9–20.2 kg/m2). More than 60% of children have siblings (n = 67, 64.4%). Eight (7.7%) and 44 (42.3%) parents declared their children had been exposed to passive smoking and pet hair, respectively. Children’s regular vaccination was confirmed by 97 (93.3%) parents. All the participants received supplementation with vitamin D3.
Basic PA and sleep behaviors in pre-school children
Realizing that on days with the infection, the child’s activity may be reduced compared to a normal day, we decided to calculate the daily average number of steps only for the days for which the child did not report any symptoms of infection (“healthy day” as a day without infection’s symptoms—6 points in symptom subscale in WURSSk-PL). The mean daily step count on healthy days (± SD) was 7152 ± 1847 steps (range: 3373–11701 steps). The mean (± SD) daily percentage in proportion to different exercise intensities was as follows—low intensity: 26.4 ± 8.3%, medium intensity: 59.7 ± 9.0%, and high intensity: 13.9 ± 6.2%. Regular sport was confirmed for 14 (13.5%) children (sport group). The duration of passive PA (defined as the number of hours spent on screen time) was grouped into 1 h or less per day, 1–2 h per day, 2–3 h per day, and more than 3 h per day, with the number of children in these groups being 36 (35%), 47 (45%), 18 (17%), 3 (3%), respectively.
Median sleep duration was 10.4 h (range: 8.0–13.1 h); 8 h or less, 9–10 h, and more than 10 h of sleep were declared by parents for 10 (9.6%), 55 (52.9%), and 39 (37.5%) children, respectively.
Severity of symptoms of upper respiratory tract infection
The median total number of days with the symptoms of URTI in our group was 26 days, for a 60-day observation period (range: 6–58 days), which is typical for this season and age group. The most predominant symptoms were a running nose and cough (repeated measures ANOVA: F(5, 515) = 52.5, p < 0.001) and infection severity (expressed as a sum of the scores for the symptom subscale – median and range) was computed at 446 points (range: 368–690 points).
Determinants of number of days with the symptoms of URTI
Age, sex, BMI, the average number of steps per day (on healthy days), the daily percentage in proportion to different exercise intensities, passive PA, regular sport, exposure to smoking, sleep duration, exposure to pet hair, vaccinations, and siblings were chosen as potential determinants of the total number of days with symptoms of URTI. Correlations between the total number of days with symptoms of URTI and quantitative determinants are presented in Fig. 2. There was a significant correlation between the total number of days with symptoms of URTI and the average daily step count.
There was a significant difference in the total number of days with symptoms of URTI between children in the sport and non-sport groups (Fig. 3d). Sex, siblings, vaccinations, exposure to pet hair and smoking, and passive PA did not influence the total number of days with symptoms of URTI (Fig. 3).
To verify the association between selected determinants, and consequently to remove redundant variables (to avoid multicollinearity) the VIF and tolerance were calculated (Supplementary Table S1). As there were no redundant determinants, all variables were included in the stepwise regression model (Supplementary Table S2). The total model accounted for 19% of the total number of days with symptoms of URTI variance (Supplementary Table S3).
Increased PA was associated with fewer days with URTIs
The level of PA, expressed as the average number of steps on healthy days in this study was inversely associated with the number of days with symptoms of URTI. A change in the average number of steps per day by 1000 steps changed the total number of days with symptoms of URTI by 4.1 days during the observation period. Furthermore, the average daily step count from healthy days was computed as a significant determinant of the total number of days with the symptoms of URTI, and it independently accounted for 43.5% (F(1, 102) = 80.32; p < 0.001) of this variable variance (Table 1 and Fig. 2). The determined standardized regression coefficient for the main relationship (average daily step count from healthy days –> total number of days with symptoms of UTRI) was corrected for the effects of other independent variables. This model accounted for 39% of the total number of days with symptoms of URTI variance (Table 1).
Regular sport participation in children protects from URTI
Additional analyses revealed that a child’s regular participation in sports activities (as declared by parents) was significantly associated with a decrease in the total number of days with symptoms of URTI (Table 2). Children regularly participating in sports activities have fewer average days with URTI symptoms than children not engaging in sports regularly (Fig. 3d). However, this predictor accounted for only 4% (F (21, 34) = 5.468; p < 0.05) of the total number of days with symptoms of URTI variance.
The results of the last step of the stepwise regression model with interaction are presented in Table 3. This model accounted for 58% (F(3, 100) = 49.09; p < 0.001) of the total number of days with symptoms of URTI variance. The average daily step count on healthy days and regular participation in sports activities were significantly associated with the total number of days with the symptoms of URTI, i.e., fewer days with the symptoms of URTI were observed in children with more daily steps, who regularly participated in sports activities. There was a significant correlation between the average daily step count of healthy days and the total number of days with symptoms of URTI in children who did not participate in sports activities regularly (r = –0.73, p < 0.001). However, there was no significant correlation among children who participated in sports activities regularly (r = 0.06, p = 0.839).
PA and severity of symptoms of URTI depending on sport participation
Furthermore, we decided to separately assess the severity of the symptoms in both the non-sport and the sports groups. The severity of the symptoms of infection (expressed as the sum of points on the symptoms subscale) was inversely associated with the average number of steps per day in the non-sport group, but not in the sports group (Table 4 and Fig. 4).
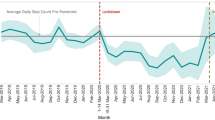
Higher baseline PA is related to fewer days with respiratory symptoms
To investigate the lag effect of PA levels and the risk of URTI, we initially analyzed the average daily number of steps during the first “run-in” of 14 days, i.e., only those days when children did not experience symptoms of infection, which was 7518 (±2299). Subsequently, we extracted two subgroups: the “active group” (i.e., with a higher mean number of steps on days without infection in the run-in: 9368 ± 1495) and the “less-active” one (with a lower mean number of steps: 5668 ± 1207). The observation of 6-week changes in the URTI symptom score revealed a significant effect, indicating an association between the baseline PA level and URTI in children (Table 5 and Fig. 5). The cumulative value of person-days with symptoms of infection over the following 46 days was reported to be significantly lower in the “active group”, vis-a-vis the “less-active group” (the slope of the regression line for “active” as compared with “less-active” group (Z proportion tests, p ≤ 0.05) (Table 6 and Fig. 6).
Discussion
Fewer days with URTIs symptoms were associated with more daily steps and regular participation in sports activities in children aged 4–7 years. Moreover, a significantly higher cumulative number of infectious person-days observed in the “less-active” group indicate that the PA level directly affects the frequency of infections. Importantly, a stronger relationship was observed between the average daily steps and the total number of days with symptoms of URTI in pediatric participants who did not engage in sports activities regularly. In the group of children not regularly participating in sports, the severity of the symptoms of URTI was associated with the daily number of steps. In the entire study population, the number of days with symptoms of URTI was not associated with the child’s sleep duration.
This is a pioneering study on children on the lagged effects of daily PA and their association with children’s URTI. The analysis was conducted on a relatively large group of participants using a reliable, standardized and validated tools to measure the daily activity and the frequency and intensity of symptoms of URTI. The Garmin Vivo Fit 1 accelerometer presented acceptable validity.28 Research on the Garmin Vivo Fit 1 has evaluated the total energy expenditure,29,30,31 time spent in different zones of PA intensity, and step counts per day and per week,29,32 as well as in specific activities.32,33,34,35 WURSSk–PL is an instrument that measures disease-specific symptoms and their impact on the QoL during URTI in children. The tool has been validated, standardized,36 and recently translated into Polish.26 The WURSS questionnaire for kids (WURSS–K) is the newest in the WURSS line of self-report instruments. The long version (WURSS 44), intended for adults, has been widely used in studies focusing on various respiratory diseases.3,37,38,39,40
In pediatric patients up to 5 years, morbidity and mortality due to RTIs continue to prevail in substantial numbers. Moreover, 45% of pre-school children who had experienced frequent colds suffered from infections later in school age.2,41 Recurrent respiratory infections, defined as eight or more infections per year, significantly spoil the QoL of pre-school children and may lead to asthma in the future.9 We demonstrated that a higher number of steps per day in preschoolers resulted in more effective immunity, reflected in fewer days with symptoms of URTI. These results are somewhat in line with those presented for older children.20,21,22,23 Jedrychowski et al. reported that low PA in preadolescents (mean age ± SD: 8.9 ± 0.4 years) is an independent predictor of increased risk of recurrent acute respiratory infections.20 Data on the frequency of respiratory infections diagnosed in children over 2 consecutive years were obtained from a survey completed by the participants’ parents. The PA level was categorized by the answers to questionnaires about engaging in sports and daily screen time. The study showed that RTIs were less frequently reported in highly or moderately active children than in those with a low PA score.20 Cieslak et al. suggested that more active children (of 10–11 years) have a higher level of secretory immunoglobulin A (SIgA) and reduced frequency of URTIs than those who are less active.21 Children filled in a survey on the occurrence of cold and flu each day of the month to monitor the incidence and duration of URTIs. PA and fitness levels were assessed from several angles: the total distance traveled per day (Digi-Walker pedometer), amount of PA and the nature of the participation, free-time activity, organized activity time, total time spent in activities (The Participation Questionnaire, PQ), time spent in all forms of habitual activity (The Habitual Activity Estimation Scale, HAES), and predicted peak aerobic (20-m shuttle run of Leger and Lambert). Similar tools to assess PA (PQ and HAES) were used by Klentrou et al.22 who examined the relationship between regular PA and several antecedents of health–fitness level, body composition, and frequency of URTIs in adolescents (mean age 14 years) in Canada. The authors showed that boys and girls classified in the high activity group reported fewer infection symptom days than those who spent less time on such activities.22 Contrary to the aforesaid studies that suggested an association between PA and RTIs in preadolescents and adolescents, in a study conducted with a group of early- and late-pubertal girls (mean age ± SD: 10 ± 2 and 15 ± 1 years, respectively) the frequency of URTIs was not correlated with PA.23 PA was quantified using Actigraph GT1M accelerometers. The frequency of URTIs was determined using the 1-month health log survey. The log quantifies the duration (number of days) and the frequency of URTIs.23 A lack of significant association between PA and respiratory infections among early- and late-pubertal girls was observed. The discrepancies between the results of Corbett et al. and other findings may be due to the PA level presented by the study group. Both in the pre-pubertal and late-pubertal groups, total MHV (moderate/hard/very hard) activity dose (min per day) was achieved at a similar level (pre-pubertal girls: ~110 min/day; late-pubertal girls: ~60 min/day—assessed based on graphically presented data in Fig. 1),23 as recommended by WHO.16 These findings may suggest that in children who achieve an appropriate PA level, the relationship between the number of days with infections and activity level does not occur. This is, to some extent, in line with the results of our study showing that the relationship between PA and URTI frequency is stronger in less-active children.
Although numerous studies suggest that the frequency of URTIs in children may be influenced by factors like exposure to tobacco smoke, obesity, and/or sleep duration,12,42,43,44,45 the present study did not reveal such relationships. Environmental factors associated with an increased risk of infections, such as daycare attendance, growing up in a rural environment, having older siblings, and having pets13 were also considered, but no correlation with symptom frequency was demonstrated. Interestingly, we did not observe an association between sex and URTIs.
The mechanisms responsible for the observed association between PA and URTI frequency in children have not been thoroughly researched and described so far. Regular PA may reduce the levels of inflammatory cytokines, thus reducing the effects of the chronic inflammatory process related to aging and chronic disease.46 Exercises are considered a factor contributing to a reduction in low-grade inflammation through reduced levels of C-reactive protein, interleukin-6, and blood mononuclear cell production of tumor necrosis factor-alpha and interleukin-1 in patients at risk for heart disease.47 Based on the literature concerning the immune response to PA in adults, it can be assumed that exercise training, especially regular moderate-intensity endurance exercise, upregulates T-helper-cell- (Th) mediated immune functions, increases lymphocyte proliferation and interleukin-2 production, and consequently helps to reduce infection risk and autoimmune diseases in elderly people.47 In addition, a significant increase in the SigA secretion rate and a decrease in URTI symptoms was observed after the 2-week detraining period in a group of young athletes. This indicates that training and competition demands affect the mucosal immune response.48 Conversely, it is known that a physical stressor induced a shift in the Th1/Th2 balance to Th2 predominance, which is associated with increased susceptibility to URTI following exhaustive physical exercise, as in completing a marathon.49
A skeletal muscle has been proven to be a crucial endocrine organ regulating systemic adaptations to exercise, releasing numerous bioactive molecules (e.g., proteins, cytokines) into circulation.50 It has recently been demonstrated that these muscle cells also secrete extracellular vesicles (EVs). EVs are membranous nanoparticles with varying morphology and content produced by every cell type in the human body. These EVs may play an important role in modulating the immune responses and cellular crosstalk following exercise.51,52 Furthermore, viral triggers, which may cause URTIs, were demonstrated to significantly alter the cargo composition of airway epithelial cell-derived EVs, resulting in elevated inflammatory cytokine production.53,54 Although EV research is still nascent and data from human studies are scarce, EVs offer a promising diagnostic potential for the beneficial effects of PA in organs beyond the skeletal muscle.55,56
Investigating the aforesaid mechanisms in children would help to establish specific doses of PA that stimulate the autoimmune response but do not induce immune imbalance.
WHO recommended that children and adolescents should engage in at least an average of 60 min per day of moderate-to-vigorous-intensity, mostly aerobic PA57 that is associated with 10,000–14,000 steps per day in children aged 4–6.58 In our study, only 7 children (5 girls) achieved a mean value of daily step count in this range. In a recent study conducted among Polish pre-school-aged children (5–6 years) from urban areas, only 6% adhered to the aforesaid WHO recommendations.59 There is no evidence to establish that 60 min per day of MVPA decreases the number of days with symptoms of URTIs and/or those symptoms' severity. In adults, regular moderate exercise can lead to a decreased incidence of URTIs and sedentary adults are more susceptible to infectious diseases, compared with active ones.3,60,61,62 Nevertheless, the authors of a systematic review published in 2020, who evaluated the effectiveness of exercise for altering the occurrence, severity, or duration of RTIs, showed that exercise did not reduce the number of URTI episodes, the proportion of participants experiencing at least one URTI during the study, or the number of symptom-days per episode of illness. Notwithstanding this, the authors emphasized that exercise may reduce the severity of URTI symptoms.4
Our study is observational and therefore causality is not obvious. It is unknown whether and for how long a given PA level preceded the effect assessed by repeated acute respiratory infections spells. The measurement of PA was carried out over a selected period, but it lasted long enough, we assume, to reflect the actual activity of children. Moreover, we recorded the average daily step count during the first 2 weeks of observation (for days without symptoms of infection) to exclude the impact of poor condition on daily activity; it is hence possible that the PA of children who experience symptoms of URTI is often limited due to the fear of deterioration of health. Parents who want to avoid the recurrence of the infection, limit the time spent outside the home and in sports activities, which lowers the daily step count.
Conclusions with clinical implications
The inverse association between the incidence of URTIs and the level/intensity of PA in pre-school children was demonstrated. Children who achieved a higher number of steps in the first days of observation had fewer days with symptoms of infection in the following days, than the less-active children. PA is a low-cost and readily available intervention that most people could readily implement.4 The positive impact of PA on the physical health of children and adolescents has been emphasized for years,15 presented in national movement guidelines,63 especially concerning cardiovascular fitness in parent-child health-related behaviors in family settings64,65 and concerning outdoor play. Through contact with the natural environment and socialization opportunities, children benefit from being exposed to sunlight, natural elements, and open air, all of which contribute to a stronger immune system.66 However, the recently observed displacement from a physically active lifestyle and the refrainment from a natural outdoor environment in all segments of the human population, even among the youngest of children, has led to a sedentary indoor lifestyle (due to excessive use of modern technology) and may be reflected in chronic diseases that are endemic to our culture.67 Parents of pre-school children should encourage their wards to engage in PA every day, creating opportunities and possibilities for PA involving entire families, especially if their children do not regularly participate in sports activities.
We desire that our study contributes to changing the habits of parents and pediatricians in many countries who, to protect children presenting with recurrent URTIs, suggest decreasing PA. However, this would require confirmatory evidence through a well-designed study with an intervention in a group of such children.
We believe, however, that this study contributes to supplementing the current recommendations for immune stimulation in children through additional, increased PA.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Schaad, U. B. OM-85 BV, an immunostimulant in pediatric recurrent respiratory tract infections: a systematic review. World J. Pediatr. 6, 5–12 (2010).
Grüber, C. et al. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatr. Allergy Immunol. 19, 505–512 (2008).
Nieman, D. C., Henson, D. A., Austin, M. D. & Sha, W. Upper respiratory tract infection is reduced in physically fit and active adults. Br. J. Sports Med. 45, 987–992 (2011).
Grande, A. J., Keogh, J., Hoffmann, T. C., Beller, E. M. & Del Mar, C. B. Exercise versus no exercise for the occurrence, severity and duration of acute respiratory infections. Cochrane Database Syst. Rev. 4, CD010596 (2020).
Meier, G. C., Watkins, J., McEwan, P. & Pockett, R. D. Resource use and direct medical costs of acute respiratory illness in the UK based on linked primary and secondary care records from 2001 to 2009. PLoS One 15, e0236472 (2020).
Feleszko, W., Ruszczyński, M. & Zalewski, B. M. Nonspecific immune stimulation in respiratory tract infections. Separating the wheat from the chaff. Paediatr. Respir. Rev. 15, 200–206 (2014).
Toivonen, L. et al. Burden of recurrent respiratory tract infections in children: a prospective cohort study. Pediatr. Infect. Dis. J. 35, e362–e369 (2016).
Schaad, U. B., Esposito, S. & Razi, C. H. Diagnosis and management of recurrent respiratory tract infections in children: a practical guide. Arch. Pediatr. Infect. Dis. 4, 1–10 (2016).
Esposito, S. et al. Prevention of new respiratory episodes in children with recurrent respiratory infections: an expert consensus statement. Microorganisms 8, 1810 (2020).
Zhou, B. et al. Risk factors for recurrent respiratory tract infection in preschool-aged children. Pediatr. Res. 90, 223–231 (2021).
Ratajczak, A. et al. Air pollution increases the incidence of upper respiratory tract symptoms among Polish children. J. Clin. Med. 10, 2150 (2021).
Bielska, D. E. et al. Exposure to environmental tobacco smoke and respiratory tract infections in pre-school children – a cross-sectional study in Poland. Ann. Agric. Environ. Med. 22, 524–529 (2015).
Kansen, H. M. et al. Risk factors for atopic diseases and recurrent respiratory tract infections in children. Pediatr. Pulmonol. 55, 3168–3179 (2020).
Hagerhed-Engman, L., Bornehag, C. G., Sundell, J. & Aberg, N. Day-care attendance and increased risk for respiratory and allergic symptoms in pre-school age. Allergy 61, 447–453 (2006).
Dimitri, P., Joshi, K. & Jones, N. Moving more: physical activity and its positive effects on long term conditions in children and young people. Arch. Dis. Child 105, 1035–1040 (2020).
Bull, F. C. et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 54, 1451–1462 (2020).
Tremblay, M. S. et al. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 14, 75 (2017).
Owen, N. et al. Sedentary behavior and public health: integrating the evidence and identifying potential solutions. Annu. Rev. Public Health 41, 265–287 (2020).
Tudor-Locke, C., Johnson, W. D. & Katzmarzyk, P. T. Accelerometer-determined steps per day in US children and youth. Med Sci. Sports Exerc. 42, 2244–2250 (2010).
Jedrychowski, W., Maugeri, U., Flak, E., Mroz, E. & Bianchi, I. Cohort study on low physical activity level and recurrent acute respiratory infections in schoolchildren. Cent. Eur. J. Public Health 9, 126–129 (2001).
Cieslak, T. J., Frost, G. & Klentrou, P. Effects of physical activity, body fat, and salivary cortisol on mucosal immunity in children. J. Appl. Physiol. 95, 2315–2320 (2003).
Klentrou, P., Hay, J. & Plyley, M. Habitual physical activity levels and health outcomes of Ontario youth. Eur. J. Appl. Physiol. 89, 460–465 (2003).
Corbett, L. et al. Correlates of mucosal immunity and upper respiratory tract infections in girls. J. Pediatr. Endocrinol. Metab. 23, 579–587 (2010).
Ostrzyżek-Przeździecka, K., Smeding, C., Bronikowski, M., Panczyk, M. & Feleszko, W. The association of physical activity and sedentary behaviors with upper respiratory tract infections and sleep duration in preschool children-study protocol. Int. J. Environ. Res. Public Health 16, 1496 (2019).
Select Statistical Services. https://select-statistics.co.uk/calculators/sample-size-calculator-population-proportion/ (accessed 13 February 2019).
Ostrzyżek-Przeździecka, K., Panczyk, M., Ratajczak, A., Bronikowski, M. & Feleszko, W. Validation and clinical evaluation of a Polish translation of the Wisconsin Upper Respiratory Symptom Survey for Kids (WURSS-K). Health Qual. Life Outcomes 19, 153 (2021).
Thompson, C. G., Kim, R. S., Aloe, A. M. & Becker, B. J. Extracting the variance inflation factor and other multicollinearity diagnostics from typical regression results. Basic Appl. Soc. Psychol. 39, 81–90 (2017).
Šimůnek, A. et al. Validity of Garmin Vívofit 1 and Garmin Vívofit 3 for school-based physical activity monitoring. Pediatr. Exerc. Sci. 31, 130–136 (2019).
Alsubheen, S. A., George, A. M., Baker, A., Rohr, L. E. & Basset, F. A. Accuracy of the vivofit activity tracker. J. Med. Eng. Technol. 40, 298–306 (2016).
Brooke, S. M. et al. Concurrent validity of wearable activity trackers under free-living conditions. J. Strength Cond. Res. 31, 1097–1106 (2017).
Price, K. et al. Validation of the Fitbit One, Garmin Vivofit and Jawbone UP activity tracker in estimation of energy expenditure during treadmill walking and running. J. Med. Eng. Technol. 41, 208–215 (2017).
An, H. S., Jones, G. C., Kang, S. K., Welk, G. J. & Lee, J. M. How valid are wearable physical activity trackers for measuring steps? Eur. J. Sport Sci. 17, 360–368 (2017).
Chen, M. D., Kuo, C. C., Pellegrini, C. A. & Hsu, M. J. Accuracy of wristband activity monitors during ambulation and activities. Med. Sci. Sports Exerc. 48, 1942–1949 (2016).
Huang, Y., Xu, J., Yu, B. & Shull, P. B. Validity of Fitbit, Jawbone UP, Nike+ and other wearable devices for level and stair walking. Gait Posture 48, 36–41 (2016).
Smith, J. D. Accuracy of wrist-worn activity monitors at three walking speeds on the treadmill. Med. Sci. Sports Exerc. 48, 783 (2016).
Schmit, K. M. et al. Wisconsin Upper Respiratory Symptom Survey for Kids: validation of an illness-specific quality of life instrument. Pediatr. Res. 90, 1207–1214 (2021).
Tiralongo, E., Wee, S. S. & Lea, R. A. Elderberry supplementation reduces cold duration and symptoms in air-travellers: a randomized, double-blind placebo-controlled clinical trial. Nutrients 8, 182 (2016).
Denlinger, L. C. et al. Vitamin D supplementation and the risk of colds in patients with asthma. Am. J. Respir. Crit. Care Med. 193, 634–641 (2016).
Goodall, E. C. et al. Vitamin D3 and gargling for the prevention of upper respiratory tract infections: a randomized controlled trial. BMC Infect. Dis. 14, 273 (2014).
Nieman, D. C. et al. Immune and inflammation responses to a 3-day period of intensified running versus cycling. Brain Behav. Immun. 39, 180–185 (2014).
Zar, H. J. & Ferkol, T. W. The global burden of respiratory disease-impact on child health. Pediatr. Pulmonol. 49, 430–434 (2014).
Arcavi, L. & Benowitz, N. L. Cigarette smoking and infection. Arch. Intern. Med. 164, 2206–2216 (2004).
Huttunen, R., Heikkinen, T. & Syrjänen, J. Smoking and the outcome of infection. J. Intern. Med. 269, 258–269 (2011).
Jedrychowski, W., Maugeri, U., Flak, E., Mroz, E. & Bianchi, I. Predisposition to acute respiratory infections among overweight preadolescent children: an epidemiologic study in Poland. Public Health 112, 189–195 (1998).
Cohen, S., Doyle, W. J., Alper, C. M., Janicki-Deverts, D. & Turner, R. B. Sleep habits and susceptibility to the common cold. Arch. Intern. Med. 169, 62–67 (2009).
Pereira, D. S. et al. TNF-α, IL6, and IL10 polymorphisms and the effect of physical exercise on inflammatory parameters and physical performance in elderly women. Age (Dordr.) 35, 2455–2463 (2013).
Romeo, J., Wärnberg, J., Pozo, T. & Marcos, A. Physical activity, immunity and infection. Proc. Nutr. Soc. 69, 390–399 (2010).
Moreira, A. et al. Salivary IgA response and upper respiratory tract infection symptoms during a 21-week competitive season in young soccer players. J. Strength Cond. Res. 28, 467–473 (2014).
Xiang, L., Rehm, K. E. & Marshall, G. D. Jr. Effects of strenuous exercise on Th1/Th2 gene expression from human peripheral blood mononuclear cells of marathon participants. Mol. Immunol. 60, 129–134 (2014).
Pedersen, B. & Febbraio, M. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
Li, T. et al. Effects of exercise on extracellular vesicles in patients with metabolic dysfunction: a systematic review. J. Cardiovasc. Transl. Res. (2022). Epub ahead of print.
McIlvenna, L. C., Whitham, M. Exercise, healthy ageing, and the potential role of small extracellular vesicles. J. Physiol. (2022). Epub ahead of print.
Chahar, H. S., Corsello, T., Kudlicki, A. S., Komaravelli, N. & Casola, A. Respiratory syncytial virus infection changes cargo composition of exosome released from airway epithelial cells. Sci. Rep. 8, 387 (2018).
Gutierrez, M. J. et al. Airway secretory microRNAome changes during rhinovirus infection in early childhood. PLoS One 11, e0162244 (2016).
Darragh, I. A. J., O’Driscoll, L. & Egan, B. Exercise training and circulating small extracellular vesicles: appraisal of methodological approaches and current knowledge. Front. Physiol. 28, 738333 (2021).
Aoi, W. & Tanimura, Y. Roles of skeletal muscle-derived exosomes in organ metabolic and immunological communication. Front. Endocrinol. (Lausanne) 14, 697204 (2021).
Chaput, J. P. et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 17, 141 (2020).
Tudor-Locke, C. et al. How many steps/day are enough? For children and adolescents. Int. J. Behav. Nutr. Phys. Act. 8, 78 (2011).
Herbert, J. et al. Objectively assessed physical activity of preschool-aged children from urban areas. Int. J. Environ. Res. Public Health 17, 1375 (2020).
Fondell, E. et al. Physical activity, stress, and self-reported upper respiratory tract infection. Med. Sci. Sports Exerc. 43, 272–279 (2011).
Matthews, C. E. et al. Moderate to vigorous physical activity and risk of upper-respiratory tract infection. Med. Sci. Sports Exerc. 34, 1242–1248 (2002).
Klentrou, P., Cieslak, T., MacNeil, M., Vintinner, A. & Plyley, M. Effect of moderate exercise on salivary immunoglobulin A and infection risk in humans. Eur. J. Appl. Physiol. 87, 153–158 (2002).
Okely, A. D. et al. A collaborative approach to adopting/adapting guidelines. The Australian 24-hour movement guidelines for children (5-12 years) and young people (13-17 years): an integration of physical activity, sedentary behaviour, and sleep. Int. J. Behav. Nutr. Phys. Act. 19, 2 (2022).
Erkelenz, N. et al. Relationship of parental health-related behaviours and physical fitness in girls and boys. Z. Gesund. Wiss. 22, 407–414 (2014).
Cleland, V., Venn, A., Fryer, J., Dwyer, T. & Blizzard, L. Parental exercise is associated with Australian children’s extracurricular sports participation and cardiorespiratory fitness: a cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2, 3 (2005).
Bento, G. & Dias, G. The importance of outdoor play for young children’s healthy development. Porto. Biomed. J. 2, 157–160 (2017).
O’Keefe, J. H., Vogel, R., Lavie, C. J. & Cordain, L. Organic fitness: physical activity consistent with our hunter-gatherer heritage. Phys. Sportsmed. 38, 11–18 (2010).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: all authors. Drafting the article or revising it critically for important intellectual content: all authors. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
The legal guardians signed a written consent to their child’s participation in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ostrzyżek-Przeździecka, K., Panczyk, M., Bronikowski, M. et al. Association of low physical activity with higher respiratory tract infections frequency among pre-school children. Pediatr Res 94, 594–602 (2023). https://doi.org/10.1038/s41390-022-02436-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02436-7