Summary
Background
Preterm infants develop smaller brain volumes compared to term newborns. Our aim is to study early brain growth related to perinatal factors in very low birth weight infants (VLBWI).
Methods
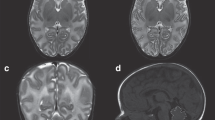
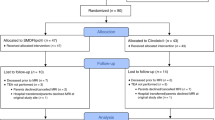
Manual segmentation of total brain volume (TBV) was performed in weekly 3D-ultrasonographies in our cohort of VLBWI. We studied the brain growth pattern related to term magnetic resonance image (term-MRI).
Results
We found different brain growth trajectories, with smaller brain volumes and a decrease in brain growth rate in those VLBWI who would later have an abnormal term-MRI (mean TBV 190.68 vs. 213.9 cm3; P = 0.0001 and mean TBV growth rate 14.35 (±1.27) vs. 16.94 (±2.29) cm3/week; P = 0.0001). TBV in those with normal term-MRI was related to gestational age (GA), being small for gestational age (SGA), sex, and duration of parenteral nutrition (TPN) while in those with abnormal term-MRI findings it was related to GA, SGA, TPN, and comorbidities. We found a deceleration in brain growth rate in those with ≥3 comorbidities.
Conclusions
An altered brain growth pattern in VLBWI who subsequently present worst scores on term-MRI is related to GA, being SGA and comorbidities. Early ultrasonographic monitoring of TBV could be useful to detect deviated patterns of brain growth.
Impact statement
-
We describe the brain growth pattern in very low birth weight infants during their first postnatal weeks.
-
Brain growth may be affected in the presence of certain perinatal factors and comorbidities, conditioning a deviation of the normal growth pattern.
-
The serial ultrasound follow-up of these at-risk patients allows identifying these brain growth patterns early, which offers a window of opportunity for implementing earlier interventions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available in the OSF repository: https://osf.io/hm9y7/?view_only=accdb3061be04b7b867512f29850cc39.
References
Ream, M. A. & Lehwald, L. Neurologic Consequences of Preterm Birth. Curr. Neurol. Neurosci. Rep. 18, 48 (2018).
Moore, T. et al. Neurological and Developmental Outcome in Extremely Preterm Children Born in England in 1995 and 2006: The Epicure Studies. BMJ 345, e7961 (2012).
Pierrat, V. et al. Neurodevelopmental Outcome at 2 Years for Preterm Children Born at 22 to 34 Weeks’ Gestation in France in 2011: Epipage-2 Cohort Study. BMJ 358, j3448 (2017).
Serenius, F. et al. Neurodevelopmental Outcome in Extremely Preterm Infants at 2.5 Years after Active Perinatal Care in Sweden. JAMA 309, 1810–1820 (2013).
Hirschberger, R. G. et al. Co-Occurrence and Severity of Neurodevelopmental Burden (Cognitive Impairment, Cerebral Palsy, Autism Spectrum Disorder, and Epilepsy) at Age Ten Years in Children Born Extremely Preterm. Pediatr. Neurol. 79, 45–52 (2018).
García, P. et al. Outcome at Two Years Corrected Age of a Cohort of Very Low Birth Weight Infants from Hospitals within the Neonatal Sen1500 Network. Pediatria 79, 279–287 (2013).
Nagy, Z. et al. Structural Correlates of Preterm Birth in the Adolescent Brain. Pediatrics 124, e964–e972 (2009).
Hinojosa-Rodriguez, M. et al. Clinical Neuroimaging in the Preterm Infant: Diagnosis and Prognosis. Neuroimage Clin. 16, 355–368 (2017).
Back, S. A. & Miller, S. P. Brain Injury in Premature Neonates: A Primary Cerebral Dysmaturation Disorder? Ann. Neurol. 75, 469–486 (2014).
Woodward, L. J., Clark, C. A., Bora, S. & Inder, T. E. Neonatal White Matter Abnormalities an Important Predictor of Neurocognitive Outcome for Very Preterm Children. PLoS ONE 7, e51879 (2012).
Inder, T. E., Wells, S. J., Mogridge, N. B., Spencer, C. & Volpe, J. J. Defining the Nature of the Cerebral Abnormalities in the Premature Infant: A Qualitative Magnetic Resonance Imaging Study. J. Pediatr. 143, 171–179 (2003).
Kidokoro, H., Neil, J. J. & Inder, T. E. New Mr Imaging Assessment Tool to Define Brain Abnormalities in Very Preterm Infants at Term. AJNR Am. J. Neuroradiol. 34, 2208–2214 (2013).
Thompson, D. K. et al. Characterisation of Brain Volume and Microstructure at Term-Equivalent Age in Infants Born across the Gestational Age Spectrum. Neuroimage Clin. 21, 101630 (2019).
Young, J. M. et al. Altered White Matter Development in Children Born Very Preterm. Brain Struct. Funct. 223, 2129–2141 (2018).
Krsnik, Z., Majic, V., Vasung, L., Huang, H. & Kostovic, I. Growth of Thalamocortical Fibers to the Somatosensory Cortex in the Human Fetal Brain. Front Neurosci. 11, 233 (2017).
Benavente-Fernández, I. et al. Ultrasonographic Estimation of Total Brain Volume: 3d Reliability and 2d Estimation. Enabling Routine Estimation During Nicu Admission in the Preterm Infant. Front Pediatr. 9, 708396 (2021).
Voss, W., Jungmann, T., Wachtendorf, M. & Neubauer, A. P. Long-Term Cognitive Outcomes of Extremely Low-Birth-Weight Infants: The Influence of the Maternal Educational Background. Acta Paediatr. 101, 569–573 (2012).
Patra, K., Greene, M. M., Patel, A. L. & Meier, P. Maternal Education Level Predicts Cognitive, Language, and Motor Outcome in Preterm Infants in the Second Year of Life. Am. J. Perinatol. 33, 738–744 (2016).
Bell, M. J. et al. Neonatal Necrotizing Enterocolitis. Therapeutic Decisions Based Upon Clinical Staging. Ann. Surg. 187, 1–7 (1978).
Bancalari, E. & Claure, N. Definitions and Diagnostic Criteria for Bronchopulmonary Dysplasia. Semin Perinatol. 30, 164–170 (2006).
International Committee for the Classification of Retinopathy of, P. The International Classification of Retinopathy of Prematurity Revisited. Arch. Ophthalmol. 123, 991–999 (2005).
Volpe, J. J. Neurology of the Newborn. Major Probl. Clin. Pediatr. 22, 1–648 (1981).
Agut, T. et al. Preterm White Matter Injury: Ultrasound Diagnosis and Classification. Pediatr. Res 87, 37–49 (2020).
Benavente-Fernandez, I. et al. Ultrasound Lineal Measurements Predict Ventricular Volume in Posthaemorrhagic Ventricular Dilatation in Preterm Infants. Acta Paediatr. 106, 211–217 (2017).
Benavente-Fernández, I. et al. Normal Cerebellar Growth by Using Three-Dimensional Us in the Preterm Infant from Birth to Term-Corrected Age. Radiology 288, 254–261 (2018).
Bouyssi-Kobar, M. et al. Third Trimester Brain Growth in Preterm Infants Compared with in Utero Healthy Fetuses. Pediatrics 138, 1–11 (2016).
Makropoulos, A. et al. Regional Growth and Atlasing of the Developing Human Brain. Neuroimage 125, 456–478 (2016).
Thompson, D. K. et al. Tracking Regional Brain Growth up to Age 13 in Children Born Term and Very Preterm. Nat. Commun. 11, 696 (2020).
de Kieviet, J. F., Zoetebier, L., van Elburg, R. M., Vermeulen, R. J. & Oosterlaan, J. Brain Development of Very Preterm and Very Low-Birthweight Children in Childhood and Adolescence: A Meta-Analysis. Dev. Med Child Neurol. 54, 313–323 (2012).
Gui, L. et al. Longitudinal Study of Neonatal Brain Tissue Volumes in Preterm Infants and Their Ability to Predict Neurodevelopmental Outcome. Neuroimage 185, 728–741 (2019).
Kersbergen, K. J. et al. Longitudinal Regional Brain Development and Clinical Risk Factors in Extremely Preterm Infants. J. Pediatr. 178, 93–100.e106 (2016).
Thompson, D. K. et al. Early Life Predictors of Brain Development at Term-Equivalent Age in Infants Born across the Gestational Age Spectrum. Neuroimage 185, 813–824 (2019).
Setanen, S. et al. Prediction of Neuromotor Outcome in Infants Born Preterm at 11 Years of Age Using Volumetric Neonatal Magnetic Resonance Imaging and Neurological Examinations. Dev. Med. Child Neurol. 58, 721–727 (2016).
Peterson, B. S. et al. Regional Brain Volume Abnormalities and Long-Term Cognitive Outcome in Preterm Infants. JAMA 284, 1939–1947 (2000).
Peterson, B. S. et al. Regional Brain Volumes and Their Later Neurodevelopmental Correlates in Term and Preterm Infants. Pediatrics 111, 939–948 (2003).
Loh, W. Y. et al. Neonatal Basal Ganglia and Thalamic Volumes: Very Preterm Birth and 7-Year Neurodevelopmental Outcomes. Pediatr. Res. 82, 970–978 (2017).
Brouwer, M. J. et al. Preterm Brain Injury on Term-Equivalent Age Mri in Relation to Perinatal Factors and Neurodevelopmental Outcome at Two Years. PLoS ONE 12, e0177128 (2017).
Asztalos, E. V. et al. Neonatal Factors Associated with a Good Neurodevelopmental Outcome in Very Preterm Infants. Am. J. Perinatol. 34, 388–396 (2017).
Parikh, N. A., Lasky, R. E., Kennedy, K. A., McDavid, G. & Tyson, J. E. Perinatal Factors and Regional Brain Volume Abnormalities at Term in a Cohort of Extremely Low Birth Weight Infants. PLoS ONE 8, e62804 (2013).
Coviello, C. et al. Effects of Early Nutrition and Growth on Brain Volumes, White Matter Microstructure, and Neurodevelopmental Outcome in Preterm Newborns. Pediatr. Res. 83, 102–110 (2018).
van Beek, P. E. et al. Increase in Brain Volumes after Implementation of a Nutrition Regimen in Infants Born Extremely Preterm. J. Pediatr. 223, 57–63 e55 (2020).
Cormack, B. E., Harding, J. E., Miller, S. P. & Bloomfield, F. H. The Influence of Early Nutrition on Brain Growth and Neurodevelopment in Extremely Preterm Babies: A Narrative Review. Nutrients 11, 1–24 (2019).
Miller, S. L., Huppi, P. S. & Mallard, C. The Consequences of Fetal Growth Restriction on Brain Structure and Neurodevelopmental Outcome. J. Physiol. 594, 807–823 (2016).
Tolsa, C. B. et al. Early Alteration of Structural and Functional Brain Development in Premature Infants Born with Intrauterine Growth Restriction. Pediatr. Res 56, 132–138 (2004).
Morsing, E., Asard, M., Ley, D., Stjernqvist, K. & Marsal, K. Cognitive Function after Intrauterine Growth Restriction and Very Preterm Birth. Pediatrics 127, e874–e882 (2011).
Aarnoudse-Moens, C. S., Weisglas-Kuperus, N., van Goudoever, J. B. & Oosterlaan, J. Meta-Analysis of Neurobehavioral Outcomes in Very Preterm and/or Very Low Birth Weight Children. Pediatrics 124, 717–728 (2009).
Guellec, I. et al. Neurologic Outcomes at School Age in Very Preterm Infants Born with Severe or Mild Growth Restriction. Pediatrics 127, e883–e891 (2011).
Levine, T. A. et al. Early Childhood Neurodevelopment after Intrauterine Growth Restriction: A Systematic Review. Pediatrics 135, 126–141 (2015).
Gilmore, J. H. et al. Regional Gray Matter Growth, Sexual Dimorphism, and Cerebral Asymmetry in the Neonatal Brain. J. Neurosci. 27, 1255–1260 (2007).
Lehtola, S. J. et al. Associations of Age and Sex with Brain Volumes and Asymmetry in 2-5-Week-Old Infants. Brain Struct. Funct. 224, 501–513 (2019).
Benavides, A. et al. Sex-Specific Alterations in Preterm Brain. Pediatr. Res. 85, 55–62 (2019).
Burnett, A. C., Cheong, J. L. Y. & Doyle, L. W. Biological and Social Influences on the Neurodevelopmental Outcomes of Preterm Infants. Clin. Perinatol. 45, 485–500 (2018).
Benavente-Fernandez, I., Siddiqi, A. & Miller, S. P. Socioeconomic Status and Brain Injury in Children Born Preterm: Modifying Neurodevelopmental Outcome. Pediatr. Res. 87, 391–398 (2020).
Benavente-Fernandez, I. et al. Association of Socioeconomic Status and Brain Injury with Neurodevelopmental Outcomes of Very Preterm Children. JAMA Netw. Open 2, e192914 (2019).
Bennet, L. et al. Chronic Inflammation and Impaired Development of the Preterm Brain. J. Reprod. Immunol. 125, 45–55 (2018).
Galinsky, R. et al. Complex Interactions between Hypoxia-Ischemia and Inflammation in Preterm Brain Injury. Dev. Med Child Neurol. 60, 126–133 (2018).
Novak, C. M., Ozen, M. & Burd, I. Perinatal Brain Injury: Mechanisms, Prevention, and Outcomes. Clin. Perinatol. 45, 357–375 (2018).
Hintz, S. R. et al. Neuroimaging and Neurodevelopmental Outcome in Extremely Preterm Infants. Pediatrics 135, e32–e42 (2015).
Schneider, J. & Miller, S. P. Preterm Brain Injury: White Matter Injury. Handb. Clin. Neurol. 162, 155–172 (2019).
Funding
This study was funded by the Cadiz integrated territorial initiative for biomedical research European Regional Development Fund (ERDF) 2014–2020. Andalusian Ministry of Health and Families, Spain. (PI-0052-2017 and ITI-0019-2019).
Author information
Authors and Affiliations
Contributions
E.R.G. and I.B.F. have played a fundamental role in the conception and design of the work, in the analysis and interpretation of the study data, in the editing of the paper and in the approval of its final version. M.L.G. has actively contributed to the data acquisition, interpretation/measurement of images, and has been involved in the approval of the final version of the paper. A.S.A. has actively contributed to the data acquisition, medical assistance in the performance of MRI scans, and has been involved in the approval of the final version of the document. P.Z.R. has actively contributed to the data acquisition, medical assistance in the performance of MRI scans, and has been involved in the approval of the final version of the document. P.M.A. has actively contributed to the data acquisition, medical assistance in the performance of MRI scans, and has been involved in the approval of the final version of the document. S.P.L.L. has played a fundamental role in the conception and design of the work, in the interpretation of the study data, and in the correction of the paper and approval of its final version.
Corresponding author
Ethics declarations
Competing interests
The first author of the paper, on behalf of himself and all the authors, declares that there is no competing interests.
Ethics approval and consent to participate
Ethics approval and consent to participate. Informed consent was obtained from all participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplemantary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ruiz-González, E., Benavente-Fernández, I., Lubián-Gutiérrez, M. et al. Ultrasonographic evaluation of the early brain growth pattern in very low birth weight infants. Pediatr Res 94, 296–303 (2023). https://doi.org/10.1038/s41390-022-02425-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02425-w
This article is cited by
-
Relationship of early brain growth pattern measured by ultrasound with neurological outcome at two years of age in very low birth weight infants
European Journal of Pediatrics (2023)