Abstract
Background
We sought to define the frequency of antibiotic resistance over time in a collection of invasive GBS isolates derived from infant early-onset disease (EOD), late-onset disease (LOD), and late-late onset disease (LLOD).
Methods
A multicenter retrospective review of infants born from 1970 to 2021 with GBS isolated from blood, cerebrospinal fluid, synovial fluid, cellulitis, or bone. All isolates were serotyped and antimicrobial susceptibility testing performed using disk diffusion.
Results
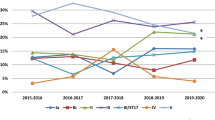
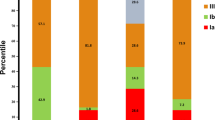
The most common serotypes in our 2017 isolates were III (n = 1112, 55.1%), Ia (n = 445, 22%), Ib (n = 182, 9%) and II (n = 146, 7.2%). A total of 945 (46.8%) isolates were from infants with EOD, 976 (48.3%) from LOD, and 96 (4.75%) from LLOD. All isolates were penicillin-susceptible. Compared to strains isolated <2000, strains isolated ≥2000 showed significantly greater frequency of erythromycin (4.0% to 32.3%, P < 0.0001) and clindamycin (1.5% to 17.5%, P < 0.0001) resistance. Year of isolation (≥2000) and serotype V were significantly associated with erythromycin and/or clindamycin resistance.
Conclusions
We document a rapid and significant increase in clindamycin and erythromycin resistance. As clindamycin may be considered in severely penicillin-allergic women needing GBS intrapartum prophylaxis, obstetricians, pediatricians, and neonatologist should be aware of this disturbing trend.
Impact
-
Group B streptococcal strains isolated from infants with invasive infection have become more resistant to second-line antibiotics over time.
-
In this epidemiologic study of 2017 group B streptococci isolated from 1970 to 2021, penicillin susceptibility remained uniform; however, resistance to erythromycin and clindamycin increased significantly over time across all capsular serotypes. Clindamycin resistance exceeded 20% by 2010 in most serotypes.
-
While penicillin remains the treatment of choice for group B streptococcal infant disease, pediatricians and neonatologists should be aware of the high prevalence of resistance to clindamycin, a recommended alternative drug used for intrapartum-antibiotic prophylaxis in penicillin-allergic women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data are available from the corresponding author upon request.
References
Nanduri, S. A. et al. Epidemiology of invasive early-onset and late-onset group B Streptococcal disease in the United States, 2006 to 2015: multistate laboratory and population-based surveillance. JAMA Pediatr. 173, 224–233 (2019).
Raabe, VN, Shane, AL. Group B Streptococcus (Streptococcus agalactiae). Microbiol Spectr. 2019;7. https://doi.org/10.1128/microbiolspec.GPP3-0007-2018
Madrid, L. et al. Infant group B streptococcal disease incidence and serotypes worldwide: systematic review and meta-analyses. Clin. Infect. Dis. 65, S160–S172 (2017). suppl_2.
Phares, C. R. et al. Epidemiology of invasive group B streptococcal disease in the United States, 1999-2005. JAMA 299, 2056–2065 (2008).
Fernandez, M., Hickman, M. E. & Baker, C. J. Antimicrobial susceptibilities of group B streptococci isolated between 1992 and 1996 from patients with bacteremia or meningitis. Antimicrob. Agents Chemother. 42, 1517–1519 (1998).
Castor, M. L. et al. Antibiotic resistance patterns in invasive group B streptococcal isolates. Infect. Dis. Obstet. Gynecol. 2008, 727505 (2008).
Francois Watkins, L. K. et al. Epidemiology of invasive group B streptococcal infections among nonpregnant adults in the United States, 2008–2016. JAMA Intern. Med. 179, 479–488 (2019).
Cieslewicz, M. J. et al. Structural and genetic diversity of group B streptococcus capsular polysaccharides. Infect. Immun. 73, 3096–3103 (2005).
Edwards, M. S. & Baker, C. J. Group B streptococcal infections in elderly adults. Clin. Infect. Dis. 41, 839–847 (2005).
Borchardt, S. M. et al. Frequency of antimicrobial resistance among invasive and colonizing Group B streptococcal isolates. BMC Infect. Dis. 6, 57 (2006).
McGee, L. et al. Multistate, population-based distributions of candidate vaccine targets, clonal complexes, and resistance features of invasive group B streptococci within the United States, 2015–2017. Clin. Infect. Dis. 72, 1004–1013 (2021).
Murdoch, D. R. & Reller, L. B. Antimicrobial susceptibilities of group B streptococci isolated from patients with invasive disease: 10-year perspective. Antimicrob. Agents Chemother. 45, 3623–3624 (2001).
Flannery, D. D. et al. Antimicrobial susceptibility profiles among neonatal early-onset sepsis pathogens. Pediatr. Infect. Dis. J. 41, 263–271 (2022).
Guo, D. et al. Neonatal colonization of group B streptococcus in China: Prevalence, antimicrobial resistance, serotypes, and molecular characterization. Am. J. Infect. Control. 46, e19–e24 (2018).
Wu, B. et al. Phenotypic and genetic differences among group B Streptococcus recovered from neonates and pregnant women in Shenzhen, China: 8-year study. BMC Microbiol. 19, 185 (2019).
Hays, C. et al. Changing epidemiology of group B streptococcus susceptibility to fluoroquinolones and aminoglycosides in France. Antimicrob. Agents Chemother. 60, 7424–7430 (2016).
Imperi, M. et al. Invasive neonatal GBS infections from an area-based surveillance study in Italy. Clin. Microbiol. Infect. 17, 1834–1839 (2011).
Kadanali, A., Altoparlak, U. & Kadanali, S. Maternal carriage and neonatal colonisation of group B streptococcus in eastern Turkey: prevalence, risk factors and antimicrobial resistance. Int. J. Clin. Pract. 59, 437–440 (2005).
Plainvert, C. et al. Multidrug-Resistant Hypervirulent Group B Streptococcus in Neonatal Invasive Infections, France, 2007–2019. Emerg. Infect. Dis. 26, 2721–2724 (2020).
Capanna, F. et al. Antibiotic resistance patterns among group B Streptococcus isolates: implications for antibiotic prophylaxis for early-onset neonatal sepsis. Swiss Med. Wkly 143, w13778 (2013).
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. U.S. Department of Health and Human Services; 2019.
Active Bacterial Core Surveillance; Centers for Disease Control and Prevention. Accessed 7 June 2022, https://www.cdc.gov/abcs/bact-facts-interactive-dashboard.html
Clinical Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests. 13th ed. Clinical Laboratory Standards Institute; 2018.
Cubria, M. B. et al. Population genomics reveals distinct temporal association with the emergence of ST1 serotype V Group B streptococcus and macrolide resistance in North America. Antimicrob. Agents Chemother. 66, e0071421 (2022).
Olesen SW, et al. The distribution of antibiotic use and its association with antibiotic resistance. Elife. 2018;7
Shenoy, E. S., Macy, E., Rowe, T. & Blumenthal, K. G. Evaluation and management of penicillin allergy: a review. JAMA 321, 188–199 (2019).
Richards VP, et al. Population gene introgression and high genome plasticity for the zoonotic pathogen Streptococcus agalactiae. Mol. Biol. Evol. 2019.
Da Cunha, V. et al. Streptococcus agalactiae clones infecting humans were selected and fixed through the extensive use of tetracycline. Nat. Commun. 5, 4544 (2014).
Teatero, S. et al. Clonal Complex 17 Group B Streptococcus strains causing invasive disease in neonates and adults originate from the same genetic pool. Sci. Rep. 6, 20047 (2016).
Author information
Authors and Affiliations
Contributions
E.M.S., M.A.S.I., M.R., T.M., H.H., M.E., C.J.B., A.R.F.: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. E.M.S., M.A.S.I., C.J.B., A.R.F.: Drafting the article or revising it critically for important intellectual content. E.M.S., M.A.S.I., C.J.B., A.R.F.: Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sabroske, E.M., Iglesias, M.A.S., Rench, M. et al. Evolving antibiotic resistance in Group B Streptococci causing invasive infant disease: 1970–2021. Pediatr Res 93, 2067–2071 (2023). https://doi.org/10.1038/s41390-022-02375-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02375-3