Abstract
Background
The aim of this study was to identify distinct trajectories of BMI growth from 2 to 7.5 years and examine their associations with markers of cardiometabolic risk at age 7.5 years among a sample of low-income Mexican American children.
Methods
This longitudinal cohort study recruited 322 mother–child dyads to participate prenatally and at child age 2, 3, 4.5, 6, and 7.5 years. Child height/weight, waist circumference, and blood pressure were assessed at each time point. Blood was collected from child at 7.5 years.
Results
Covarying for birthweight, three BMI trajectories were identified: Low-Stable BMI (73% of the sample), High-Stable BMI (5.6% of the sample), and Increasing BMI over time (21.4% of the sample). The High-Stable and Increasing BMI classes had higher waist circumference and systolic blood pressure and lower HDL-c than the Low-Stable BMI class (ps < 0.05). Among children with BMIs below the 85th percentile, 16% had three or more cardiometabolic risk indicators.
Conclusions
BMI classes were consistent with existing literature. For youth, standard medical practice is to examine cardiometabolic risk indicators when BMI is high; however, this practice would miss 16% of youth in our sample who exhibit cardiometabolic risk but do not screen in based on BMI.
Impact
-
Research indicates Mexican American youth are at risk for cardiometabolic dysregulation relative to other ethnic groups, yet there is a paucity of longitudinal research.
-
An Increasing BMI and a High-Stable BMI class were associated with larger waist circumference, higher systolic blood pressure, and lower HDL cholesterol than the Low-Stable BMI class.
-
BMI trajectories in childhood predict cardiometabolic risk indicators. As the sole screener for deciding when to test cardiometabolic indicators, BMI alone will miss some children exhibiting cardiometabolic dysregulation.
Similar content being viewed by others
Introduction
Cardiometabolic diseases are one of the leading causes of death in the world,1 with common risk factors including excess weight in the abdomen, high triglyceride levels, low high-density lipoprotein cholesterol (HDL-c) levels, high blood pressure, and insulin resistance.2 In a national epidemiological study of adolescents 12–19 years of age, Hispanic youth had the highest prevalence of cardiometabolic risk (11.2%) relative to other racial and ethnic groups, with large waist circumference (WC), high fasting triglycerides, high glucose concentrations, and low HDL-c as salient risk factors.3 Further, in a study of Mexican American children from ages 6 to 18 years with a family history of type 2 diabetes, 31.8% had large WC, 31.9% had low HDL-c, 13.8% had hypertriglyceridemia, 24.9% had hyperinsulinemia, 13.2% had glucose intolerance, 11.9% had elevated blood pressure, with 18.7% of the sample having 3 or more of the risk indicators.4 Higher rates are found in studies with overweight Hispanic youth, with the prevalence of having 3 or more cardiometabolic risk indicators ranging from 27 to 30%.4,5,6 Higher rates of prediabetes and elevated blood pressure have been found in Hispanic boys relative to girls.7 Even Hispanic children as young as 4–6 years old are found with cardiometabolic risk indicators.4,5 Elevated cardiometabolic risk indicators in childhood can persist into adulthood, contribute to the development of type 2 diabetes and cardiovascular disease, and are associated with negative health, economic, and quality of life consequences.8,9,10 Early detection and prevention is critical, but to accomplish this, “ethnicity-inclusive studies on risk identification” are needed.11
Researchers have examined body mass index (BMI) trajectories as predictors of cardiometabolic risk indicators in youth, but a paucity of research exists with Mexican American children. Among youth broadly, BMI trajectories from 0 to 2 years,12,13 0 to 5 years,14,15 0 to 11 years,16 2 to 11 years,17 4 to 18 years,18 and 6 to 18 years19 are associated with cardiometabolic risk indicators in early childhood (i.e., 3 to 5 years),13,14,15 adolescence,12,16,17 and young adulthood.18,19 Collectively, BMI trajectories that are high and stable13,15,17,18 and/or increasing at relatively higher rates than others13,14,15,19 are associated with cardiometabolic risk indicators. However, not all studies assess the same cardiometabolic risk indicators. Specifically, BMI trajectories in childhood have been associated with triglycerides,18 WC,12,14,15 sum of skinfold measurements12,13,16 in childhood and adolescence, and fasting glucose,16 blood pressure,16 and insulin resistance12,16 in adolescence.
There is no accepted or validated definition of cardiometabolic risk in youth11,20 and a current limitation of the existing literature is that different studies use different definitions, cutoffs, and risk indicators.20 Despite this limitation, research on youth collectively finds associations between BMI trajectory and cardiometabolic risk indicators more often than not. Given the lack of research with Mexican American children, the purpose of the current study was to track BMI trajectories from 2 to 7.5 years and examine their associations with cardiometabolic risk indicators at 7.5 years in a sample of low-income Mexican American children. It was hypothesized that BMI trajectory classes would be differentially predictive of cardiometabolic risk indicators. Although it was unknown what BMI trajectory classes would emerge a priori, it was hypothesized to be consistent with the existing literature such that those with steeper slopes in BMI trajectories (i.e., more growth over time) or those with stable high BMI trajectories would exhibit elevated cardiometabolic risk indicators.
Method
Study design and participants
We used data from a longitudinal cohort study conducted in the southwestern United States between 2010 and 2020. Pregnant women were recruited from local community prenatal clinics that serve low-income families. Eligibility criteria included (1) low-income status (e.g., family income <$25,000), (2) age 18 or older, (3) Spanish or English fluency, (4) self-identification as Mexican or Mexican American, (5) singleton delivery, and (6) no prenatal evidence of an infant health or developmental problem. This study was approved by the Institutional Review Boards of Arizona State University and the Maricopa Integrated Health System and was compliant with all ethics requirements.
A total of 322 Mexican American mother-child dyads participated in the study. The current study uses child BMI data collected at 2, 3, 4.5, 6, and 7.5 years of age. Mothers provided written informed consent prior to participation, and children provided verbal assent at the 7.5-year timepoint. Medical records at the hospital of birth were obtained for child birth weight. Child height and weight, waist circumference, and blood pressure were assessed in the lab by trained staff at each timepoint. Blood was collected from children and analyzed for total cholesterol (TC), HDL-c, and hemoglobin A1c (HbA1c) at the 7.5-year timepoint.
Measures
zBMI
Child height and weight were obtained by a trained research assistant at each timepoint using standardized protocols from National Health and Nutrition Examination Survey.21 Child standing height was measured using a wall-mounted stadiometer. Child weight was measured using a calibrated precision Tanita digital scale (SC-331S, Tanita Corporation of American, Inc). BMI was calculated by dividing weight in kilograms by height in meters squared. zBMI were determined using the World Health Organization (WHO) growth standards for age and biological sex,22 and associated software.22 The program flags and sets to missing any WLZ% and BMIz% scores considered “biologically implausible,” based on a z-score <−5.0 or >5.0.
Cardiometabolic risk indicators
The cardiometabolic risk indicators included WC, systolic and diastolic blood pressure, HbA1c, HDL-c, and TC. WC was measured in a standing position with feet together using a non-stretchable measuring tape around the waist at the midaxillary line and uppermost lateral border of the ilium and recorded to the nearest 0.1 cm by trained research assistants (consistent with National Health and Nutrition Examination Survey standardized protocol).23 Age- and sex-based WC percentiles were calculated from established percentiles for Mexican American children.24 Children with WC at the 75th percentile were considered borderline high and those at the 90th percentile or greater as high risk. After children relaxed for 5 min, their systolic and diastolic blood pressure were measured in a sitting position using a blood pressure device with age-appropriate cuffs (Omron 705IT monitor). Measurements are done in duplicate and averaged. Age-, sex-, and height-specific systolic and diastolic blood pressure percentiles were derived according to recommended guidelines.25 Elevated blood pressure was defined as having systolic or diastolic blood pressure ≥90th percentile. Capillary blood samples were obtained using a non-fasting finger stick method with a 40 μL capillary tube, transferred into a cassette, and analyzed by Alere Cholestech LDX machine using Lipid Profile and GLU cassettes (Cholestech Alere Health Hayward, CA).26 These data were used to calculate non-fasting HbA1c, HDL-c, and TC and determine cardiometabolic risk status. Increased cardiovascular risk was determined according to the following criteria: HbA1c ≥ 5.7%;27 HDL-c < 40 mg/dL low, 40–45 borderline low, >45 acceptable;28 TC < 170 mg/dL acceptable, 170–199 mg/dL borderline high, ≥200 mg/dL high.28 Research demonstrates that differences in fasting and non-fasting HDL-c and TC are minimal and clinically negligible.29,30,31
Covariates
Child birth weight was obtained from medical records and recorded in lbs and oz. Maternal BMI was collected at a laboratory visit when children were approximately 2 years of age (pregnant mothers were excluded).
Analytic approach
At the 7.5-year timepoint, we had 87% retention of the original 322 participants collected at birth. However, due to the coronavirus disease 2019 (COVID-19) pandemic and shutdown of in-person research, 182 participants attended the 7.5-year lab visit in person, while the rest of the participants completed phone interviews. Comparing those that did not participate versus those that participated using independent samples t tests and chi-square analyses in SPSS v26, revealed no differences with respect to child sex, mother-reported economic hardship, maternal country of birth, number of years in the U.S., mother’s age, level of education, or number of other children.
A quadratic covariance pattern mixture model (CPMM) with a class-specific heterogenous compound symmetric covariance matrix was fit to BMI data to identify latent groups of growth trajectories from child age 2–7.5 years. CPMMs are theoretically aligned with the more commonly employed growth mixture models (GMMs) and similarly allow for class-specific covariance structures to be flexibly modeled. CPMMs are advantageous in that they avoid within-class random effects and substantially reduce nonconvergence issues common among GMMs that are known to adversely affect parameter estimates, class assignment, and class enumeration.32,33,34 Overall, CPMMs are considered a less computationally complex method that outperform GMMs when answering questions related to population mean trajectories.
CPMMs estimate the probability of class membership for individuals based on similarities in growth trajectories. Birthweight was centered and included as a within-class predictor of intercept and growth parameters. Models with 1–5 classes were tested and class enumeration was informed by the classification likelihood criteria (CLC), with lower values indicating more parsimonious fit.33,34,35,36 Analyses were conducted using Mplus 8.437 using maximum likelihood estimation to account for missing data given that missing values adhere to missing at random assumptions.
After determining the optimal number of BMI classes, the BCH method38,39 was employed to examine mean level differences in metabolic health indicators across classes using the chi-square test of significance. The metabolic health indicators were entered as auxiliary variables, meaning they had no bearing on the CPMM probabilistic classification algorithm, and listwise deletion was used.
Results
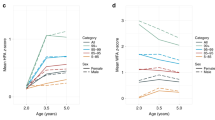
Sample demographics are presented in Table 1. A series of five latent class models were estimated and model fit information is depicted in Table 2. The 3-class solution (see Fig. 1) was retained as the best fitting model based on the lowest CLC value. CLC was considered the best for class enumeration for several reasons. First, it includes no parsimony penalty, but does penalize for entropy and tends to perform well with modest sample sizes.34,35 Second, the integrated classification likelihood metrics that penalize for both parsimony and entropy tend to under-select when relative entropy is below 0.80.34,35 Finally, the 5-class solution provides small classes with relative entropy too low to trust classifications.34 Class 1 had the highest most-likely class membership (n = 235; 73%) and was characterized by low stable BMI values across the time points assessed (linear −0.99 ± 0.09, p = <0.001; quadratic 0.17 ± 0.02, p < 0.001). Class 2 (n = 69; 21.4%) was notable for a pronounced increase in BMI from 2 to 7.5 years (linear −0.22 ± 0.19, p = 0.26; quadratic 0.25 ± 0.04, p < 0.001). The third class accounted for 5.6% of the sample (n = 18) and was characterized by stable high BMI values (linear 0.13 ± 2.85, p = 96; quadratic 0.14 ± 0.37, p = 0.72). This 3-class solution with a Low-Stable BMI, Increasing BMI, and High-Stable BMI is consistent with the existing literature.40 Birthweight was not a significant predictor of intercept and growth parameters in classes 1 or 3, but positively predicted the linear growth (p = 0.015) and negative quadratic growth (p = 0.05) in class 2. A chi-square test of significance revealed no significant differences between classes in maternal BMI (p = 0.099) and no significant pairwise comparisons.
As Table 3 displays, there were significant differences between the classes on WC and HDL-c, such that both the Increasing BMI Class 2 and High-Stable BMI Class 3 had higher scores on WC, and lower scores on HDL-c than the Low-Stable BMI Class 1. The Increasing BMI Class 2 had higher systolic and diastolic blood pressure than the Low Stable BMI Class 1. Systolic blood pressure was higher in the High-Stable BMI Class 3 relative to the Low-Stable BMI Class 1. The number of children in each class that were classified as at risk for each cardiometabolic health indicator is reported in Table 4. Notably, although there were 95 children with a BMI below the 85th percentile at 7.5 years, 23 were classified as borderline high risk and 6 high risk for unhealthy WC, 14 had systolic and 5 had diastolic BP in the high range, 6 had HDL-c in the borderline high and 8 in the high risk, and 15 had borderline high and 4 high risk for TC. There were 16% of children with three or more cardiometabolic risk indicators whose BMI was below the 85th percentile. Thus, there are children in the normal weight range that nonetheless exhibit elevated cardiometabolic risk.
Discussion
Consistent with the existing literature,40 three latent classes of BMI trajectories emerged consisting of High-Stable BMI, Increasing BMI, and Low-Stable BMI among a sample of low-income Mexican American children. The three classes were differentially associated with cardiometabolic risk indicators at 7.5 years of age, such that High-Stable BMI and Increasing BMI Classes had lower HDL-c, higher WC, and higher systolic blood pressure than the Low- Stable BMI Class. Our results are consistent with existing cross-sectional research on Mexican American youth, demonstrating an association between BMI and WC, low HDL-C, and blood pressure.3,4,5,6 In addition, our findings are consistent with longitudinal research demonstrating an association between BMI trajectories and cardiometabolic risk indicators among non-Mexican American samples.13,14,15,17,19 There were no BMI class differences on HbA1c levels; this may be due to the low number of children in the sample with an HbA1c at or above 5.7 (n = 7 children). Overall, findings suggest that children as young as 7.5 years begin to show cardiometabolic dysregulation.
Physical growth in childhood is associated with health and wellness throughout the lifespan. The American Academy of Pediatrics currently recommends annual assessment of BMI for all children, using change in BMI to identify rate of excessive weight gain relative to linear growth, and for those at risk, to monitor chronic health conditions such as hypertension or glucose intolerance. Although our data suggest BMI trajectories predict cardiometabolic risk in Mexican American children, it is noteworthy that approximately 31% of our sample had elevated WC, and 20% had elevated TC but were of normal weight. Further, 16% of children within the normal weight range had three or more cardiometabolic risk indicators. This finding suggests that the use of BMI alone as a screener may miss a critical subgroup of youth displaying cardiometabolic risk factors. Previous research has found associations with WC and cardiometabolic risk indicators, future research should examine if WC trajectories alone or in combination with BMI better screen for cardiometabolic risk indicators among Mexican American children.
Several considerations are relevant to interpretation of the current findings. First, COVID-19 restrictions limited our ability to collect cardiometabolic data on the full sample of children at 7.5 years. Given the uniqueness of the current sample, our results may not generalize to higher SES, non-Mexican American populations. The current study’s analytic approach (CPMMs) may be better suited to answer questions relevant to population mean trajectories, relative to traditional growth mixture modeling approaches. At the 7.5 years of age, there were overweight/obese children in each class due to their weight trajectory over time. For example, children in the Increasing BMI Class 2 had the highest weight increase over time (i.e., slope) from age 2 to 7.5 years with some children classifying as obese by 7.5 years (see Table 4). In contrast, the Low-Stable BMI Class 1 consisted of children who slightly decreased weight at 4.5 and then increased weight by 7.5 years, with 5% classifying as obese at 7.5 years. Thus, the labels for the classes are not perfect descriptors of all the individuals in the class.
The current study extends our understanding of childhood BMI trajectories and subsequent cardiometabolic risk to a sample of low-income, Mexican American children, an understudied population at elevated risk for cardiometabolic dysregulation. Given the lack of research on Mexican American youth, the results will benefit from replication. Additional culturally-informed longitudinal research that examines predictors and moderators of BMI trajectories and cardiometabolic health among Mexican American youth is needed. Equally important is the examination of youth who, despite being in a high-risk environment for obesity, maintain a healthy weight. Finally, research is needed to identify the socio-cultural-environmental factors that contribute to healthy weight development despite a high-risk environment.
Data availability
Data can be made available upon request and subject to Institutional Review Board approval.
References
World Health Organization. Cardiovascular diseases. http://www.who.int/mediacentre/factsheets/fs317/en/ (2021).
National Heart, Lung, and Blood Institute. Metabolic syndrome. https://www.nhlbi.nih.gov/health-topics/metabolic-syndrome (2021).
Johnson, W. D. et al. Prevalence of risk factors for metabolic syndrome in adolescents: National Health and Nutrition Examination Survey (NHANES), 2001–2006. Arch. Pediatr. Adolesc. Med. 163, 371–377 (2009).
Fowler, S. P. et al. Genetic epidemiology of cardiometabolic risk factors and their clustering patterns in Mexican American children and adolescents: the SAFARI Study. Hum. Genet. 132, 1059–1071 (2013).
Butte, N. F. et al. Quantitative genetic analysis of the metabolic syndrome in Hispanic children. Pediatr. Res. 58, 1243–1248 (2005).
Cruz, M. L. et al. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J. Clin. Endocrinol. Metab. 89, 108–113 (2004).
Isasi, C. R. et al. Sex differences in cardiometabolic risk factors among Hispanic/Latino youth. J. Pediatr. 176, 121–127 (2016).
Steinberger, J. et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation 119, 628–647 (2009).
Weiss, R. et al. Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 350, 2362–2374 (2004).
Birnbaum, H. G., Mattson, M. E., Kashima, S. & Williamson, T. E. Prevalence rates and costs of metabolic syndrome and associated risk factors using employees’ integrated laboratory data and health care claims. J. Occup. Environ. Med. 53, 27–33 (2011).
DeBoer, M. D. Ethnicity, obesity, and the metabolic syndrome: implications on assessing risk and targeting intervention. Expert Rev. Endocrinol. Metab. 6, 279–289 (2011).
Aris, I. M. et al. Association of weight for length vs body mass index during the first 2 years of life with cardiometabolic risk in early adolescence. JAMA Netw. Open 1, e182460 (2018).
Aris, I. M. et al. Body mass index trajectories in the first two years and subsequent childhood cardio-metabolic outcomes: a prospective multiethnic Asian cohort study. Sci. Rep. 7, 8424 (2017).
Wibaek, R. et al. Body mass index trajectories in early childhood in relation to cardiometabolic risk profile and body composition at 5 years of age. Am. J. Clin. Nutr. 110, 1175–1185 (2019).
Li, X. et al. The association between body mass index trajectories and cardiometabolic risk in young children. Pediatr. Obes. 15, e12633 (2020).
Beardsall, K. et al. Heritability of childhood weight gain from birth and risk markers for adult metabolic disease in prepubertal twins. J. Clin. Endocrinol. Metab. 94, 3708–3713 (2009).
Lycett, K. et al. Body mass index from early to late childhood and cardiometabolic measurements at 11 to 12 years. Pedatrics 146, e20193666 (2020).
Oluwagbemigun, K. et al. Developmental trajectories of body mass index from childhood into late adolescence and subsequent late adolescence-young adulthood cardiometabolic risk markers. Cardiovasc. Dabetol. 18, 9 (2019).
Yuan, Y. et al. Body mass index trajectories in early life is predictive of cardiometabolic risk. J. Pediatr. 219, 31–37 (2020).
Brambilla, P. & Pietrobelli, A. Behind and beyond the pediatric metabolic syndrome. Ital. J. Pediatr. 35, 41 (2009).
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) Anthropometry Procedures Manual (U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2007).
de Onis, M., Garza, C. & Victora, C. G. The WHO multicentre growth reference study: strategy for developing a new international growth reference. Forum Nutr. 56, 238–240 (2003).
U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. National Health and Nutrition Examination Study (NHANES) anthropometry procedures manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf (2007–2008).
Fernández, J. R., Redden, D. T., Pietrobelli, A. & Allison, D. B. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J. Pediatr. 145, 439–444 (2004).
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents: The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 114, 555–576 (2004).
Alere Cholestech LDX Lipid Profile GLU Cassettes CLSI. (CLSI196 vC 10/17). https://www.alere.com/en/home/product-details/cholestech-ldx-system.html (2004).
Wallace, A. S., Wang, D., Shin, J. & Selvin, E. Screening and diagnosis of prediabetes and diabetes in US children and adolescents. Pediatrics 146, e20200265 (2020).
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Summary Report. Pediatrics 128, S213–S256 (2011).
Szternel, L., Krintus, M., Bergmann, K., Derezinski, T. & Sypniewska, G. Non-fasting lipid profile determination in presumably healthy children: impact on the assessment of lipid abnormalities. PLoS ONE 13, e0198433 (2018).
Sidhu, D. & Naugler, C. Fasting time and lipid levels in a community-based population. A cross-sectional study. Arch. Intern. Med. 172, 1707–1710 (2012).
Langsted, A., Freiberg, J. J. & Nordestgaard, B. G. Fasting and nonfasting lipid levels: influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation 118, 2047–2056 (2008).
McNeish, D. & Harring, J. Covariance pattern mixture models: eliminating random effects to improve convergence and performance. Behav. Res. Methods 52, 947–979 (2019).
McNeish, D. & Harring, J. Improving convergence in growth mixture models without covariance structure constraints. Stat. Methods Med. Res. 30, 994–1012 (2021).
McNeish, D. et al. Facilitating growth mixture model convergence in preventive interventions. Prev. Sci. https://doi.org/10.1007/s11121-021-01262-3 (2021).
McNeish, D., Harring, J. R, & Bauer, D. J. Nonconvergence, covariance constraints, and class enumeration in growth mixture models. Psychol. Methods https://doi.org/10.1037/met0000456 (2022).
Yang, C.-C. Evaluating latent class analysis models in qualitative phenotype identification. Comput. Stat. Data Anal. 50, 1090–1104 (2006).
MPLUS (Version 6.11) (Muthén & Muthén, 2022).
Asparouhov, T. & Muthén, B. Auxiliary variables in mixture modeling: using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes 21, 1–22 (2014).
Bolck, A., Croon, M. & Hagenaars, J. Estimating latent structure models with categorical variables: one-step versus three-step estimators. Political Anal. 12, 3–27 (2004).
Mattsson, M. et al. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes. Rev. 20, 998–1015 (2019).
Acknowledgements
We thank the mothers and children for their participation.
Funding
This research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Minority Health and Health Disparities, and Institute for Educational Sciences. The funding agencies were not involved in the study design, data analysis, writing of this manuscript, or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of funding agencies.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of this manuscript, and no one received payment for the writing of this manuscript. M.P. and L.J.L. were involved in the idea development, study design, data collection, and writing and editing all sections of the manuscript. L.K.W. and D.M. created the data analytic plan, data cleaning, data analyses, and drafting of “Results” section. J.C.H. and S.G.C. contributed to writing all sections, idea development, and data collection. All authors edited all sections of the paper and approved final draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All aspects of the study comply with ethical standards and were approved by Arizona State University’s Institutional Review Board. Written informed consent was obtained from mothers at each study timepoint.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Perez, M., Winstone, L.K., Hernández, J.C. et al. Association of BMI trajectories with cardiometabolic risk among low-income Mexican American children. Pediatr Res 93, 1233–1238 (2023). https://doi.org/10.1038/s41390-022-02250-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02250-1
This article is cited by
-
Changes in general and abdominal obesity in children at 4, 6 and 9 years of age and their association with other cardiometabolic risk factors
European Journal of Pediatrics (2023)